Korean J Orthod.
2018 Mar;48(2):113-124. 10.4041/kjod.2018.48.2.113.
Orthodontic and orthopedic treatment for a growing patient with Tessier number 0 cleft
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Seoul National University, Seoul, Korea. drwhite@snu.ac.kr
- 2Dental Research Institute, Seoul National University, Seoul, Korea.
- 3Department of Plastic and Reconstructive Surgery, Seoul National University Hospital, Seoul, Korea.
- 4Department of Plastic and Reconstructive Surgery, Seoul National University College of Medicine, Seoul, Korea.
- 5Department of Oral and Maxillofacial Surgery, School of Dentistry, Seoul National University, Seoul, Korea.
- KMID: 2406820
- DOI: http://doi.org/10.4041/kjod.2018.48.2.113
Abstract
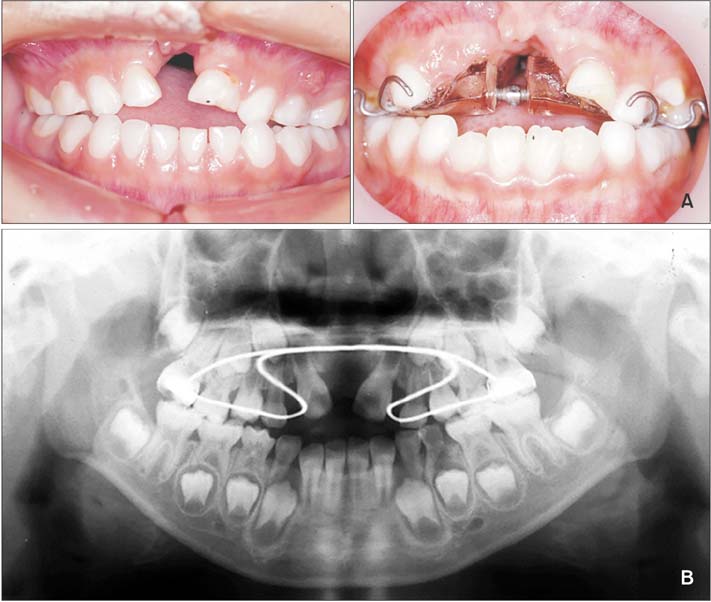
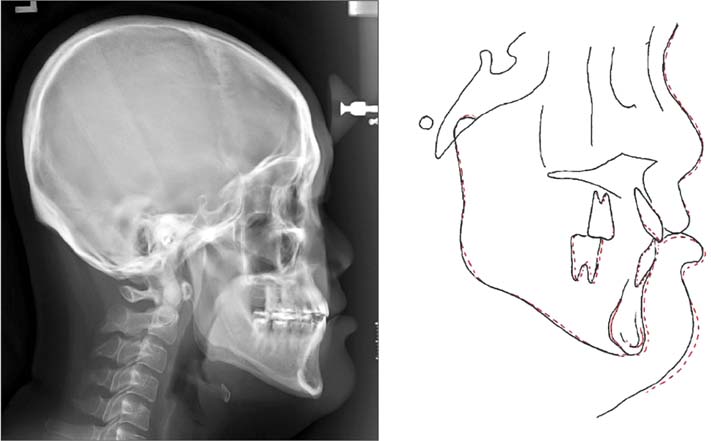
- The purpose of this case report was to introduce the concept of orthodontic and orthopedic treatment for a growing patient with Tessier number 0 cleft. A 5-year-old boy patient with Tessier number 0 cleft presented congenitally missing maxillary central incisors (MXCI), a bony defect at the premaxilla, a constricted maxillary arch, an anterior openbite, and maxillary hypoplasia. His treatment was divided into three stages: management of the bony defect at the premaxilla and the congenitally missing MXCIs using a fan-type expansion plate, iliac bone grafting, and eruption guidance of the maxillary lateral incisors into the graft area for substitution of MXCIs; management of the maxillary hypoplasia using sequential facemask therapy with conventional and skeletal anchorage; and management of the remaining occlusal problems using fixed orthodontic treatment. The total treatment duration was 15 years and 10 months. Class I canine and Class II molar relationships and normal overbite and overjet were achieved at the end of treatment. Although the long-term use of facemask therapy resulted in significant protraction of the retrusive maxilla, the patient exhibited Class III profile because of continued mandibular growth. However, the treatment result was well maintained after 2 years of retention. The findings from this case suggest that interdisciplinary and customized approaches are mandatory for successful management of maxillary hypoplasia, bony defect, and dental problems in Tessier number 0 cleft. Moreover, considering the potential of orthognathic surgery or distraction osteogenesis, meticulous monitoring of mandibular growth until growth completion is important.
MeSH Terms
Figure
Cited by 1 articles
-
Distribution, side involvement, phenotype and associated anomalies of Korean patients with craniofacial clefts from single university hospital-based data obtained during 1998–2018
Jee Hyeok Chung, Sunjin Yim, Il-Sik Cho, Seung-Weon Lim, Il-Hyung Yang, Jeong Hyun Ha, Sukwha Kim, Seung-Hak Baek
Korean J Orthod. 2020;50(6):383-390. doi: 10.4041/kjod.2020.50.6.383.
Reference
-
1. Kawamoto HK. Rare craniofacial clefts. In : McCarthy JG, editor. Plastic surgery. Philadelphia: WB Saunders;1990. p. 389–550.2. Tessier P. Anatomical classification facial, craniofacial and latero-facial clefts. J Maxillofac Surg. 1976; 4:69–92.3. da Silva Freitas R, Alonso N, Shin JH, Busato L, Ono MC, Cruz GA. Surgical correction of Tessier number 0 cleft. J Craniofac Surg. 2008; 19:1348–1352.
Article4. Guruprasad Y, Chauhan DS. Midline nasal dermoid cyst with Tessier's 0 cleft. J Nat Sci Biol Med. 2014; 5:479–482.
Article5. Council of the University Faculties of Orthodontics in Korea. Textbook of orthodontics. Seoul: Jeesung Pub. Co;2014.6. Delaire J. Maxillary development revisited: relevance to the orthopaedic treatment of Class III malocclusions. Eur J Orthod. 1997; 19:289–311.
Article7. Baek SH, Kim KW, Choi JY. New treatment modality for maxillary hypoplasia in cleft patients. Protraction facemask with miniplate anchorage. Angle Orthod. 2010; 80:783–791.8. Ahn HW, Kim KW, Yang IH, Choi JY, Baek SH. Comparison of the effects of maxillary protraction using facemask and miniplate anchorage between unilateral and bilateral cleft lip and palate patients. Angle Orthod. 2012; 82:935–941.
Article9. Seo YJ, Park JW, Kim YH, Baek SH. Initial growth pattern of children with cleft before alveolar bone graft stage according to cleft type. Angle Orthod. 2011; 81:1103–1110.
Article10. Enemark H, Sindet-Pedersen S, Bundgaard M. Long-term results after secondary bone grafting of alveolar clefts. J Oral Maxillofac Surg. 1987; 45:913–919.
Article11. De Riu G, Lai V, Congiu M, Tullio A. Secondary bone grafting of alveolar cleft. Minerva Stomatol. 2004; 53:571–579.12. Schultze-Mosgau S, Nkenke E, Schlegel AK, Hirschfelder U, Wiltfang J. Analysis of bone resorption after secondary alveolar cleft bone grafts before and after canine eruption in connection with orthodontic gap closure or prosthodontic treatment. J Oral Maxillofac Surg. 2003; 61:1245–1248.
Article13. Susami T, Okayasu M, Inokuchi T, Ohkubo K, Uchino N, Uwatoko K, et al. Maxillary protraction in patients with cleft lip and palate in mixed dentition: cephalometric evaluation after completion of growth. Cleft Palate Craniofac J. 2014; 51:514–524.
Article14. Seo J, Kim S, Yang IH, Baek SH. Effect of secondary alveolar bone grafting on the maxillary growth: unilateral versus bilateral cleft lip and palate patients. J Craniofac Surg. 2015; 26:2128–2132.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anatomical repair of a bilateral Tessier No. 3 cleft by midfacial advancement
- Tessier number 7 cleft with unilateral complete cleft lip and palate: a case report
- A Case of Rare Craniofacial Clefts: Tessier No .7 Cleft
- A Wedge-Shaped Anterior Hairline Extension Associated with a Tessier Number 10 Cleft
- Tessier No. 2 Oblique Facial Cleft Not Associated with Cleft Lip or Palate: a Case Report