Evaluation of the effects of miniscrew incorporation in palatal expanders for young adults using finite element analysis
- Affiliations
-
- 1Department of Orthodontics, College of Dentistry, Yonsei University, Seoul, Korea. orthojn@yuhs.ac
- 2Institute of Craniofacial Deformity, College of Dentistry, Yonsei University, Seoul, Korea.
- 3Division of Anatomy and Developmental Biology, Department of Oral Biology, Human Identification Research Institution, BK21 PLUS Project, College of Dentistry, Yonsei University, Seoul, Korea.
- KMID: 2406816
- DOI: http://doi.org/10.4041/kjod.2018.48.2.81
Abstract
OBJECTIVE
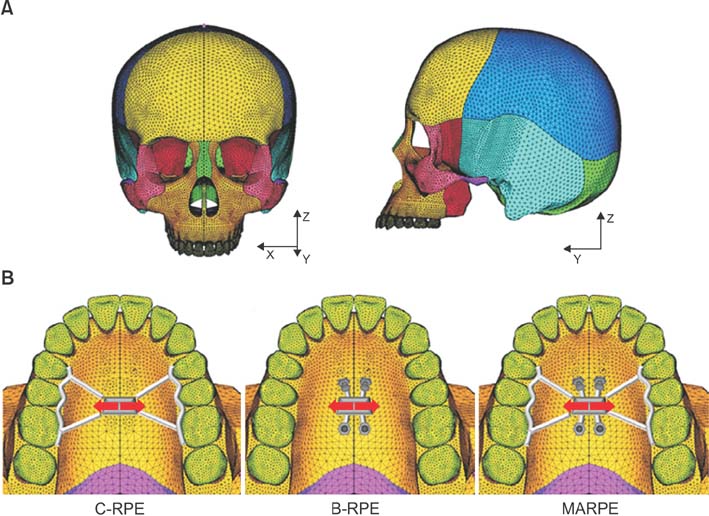
The aim of this study was to evaluate the stress distribution and displacement of various craniofacial structures after nonsurgical rapid palatal expansion (RPE) with conventional (C-RPE), bone-borne (B-RPE), and miniscrew-assisted (MARPE) expanders for young adults using three-dimensional finite element analysis (3D FEA).
METHODS
Conventional, bone-borne, and miniscrew-assisted palatal expanders were designed to simulate expansion in a 3D FE model created from a 20-year-old human dry skull. Stress distribution and the displacement pattern for each circumaxillary suture and anchor tooth were calculated.
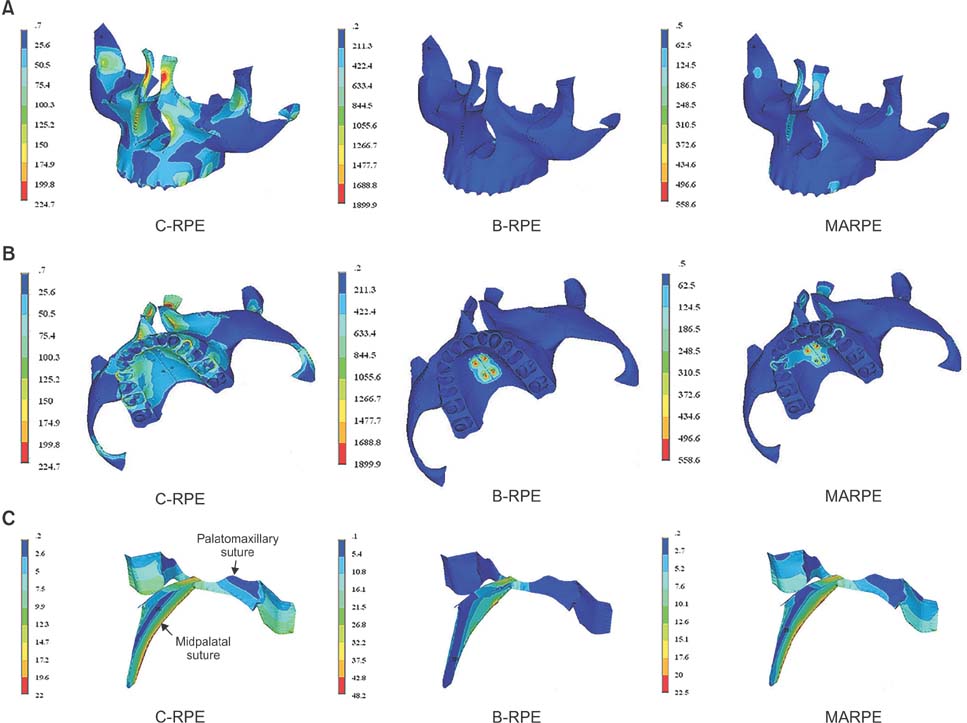
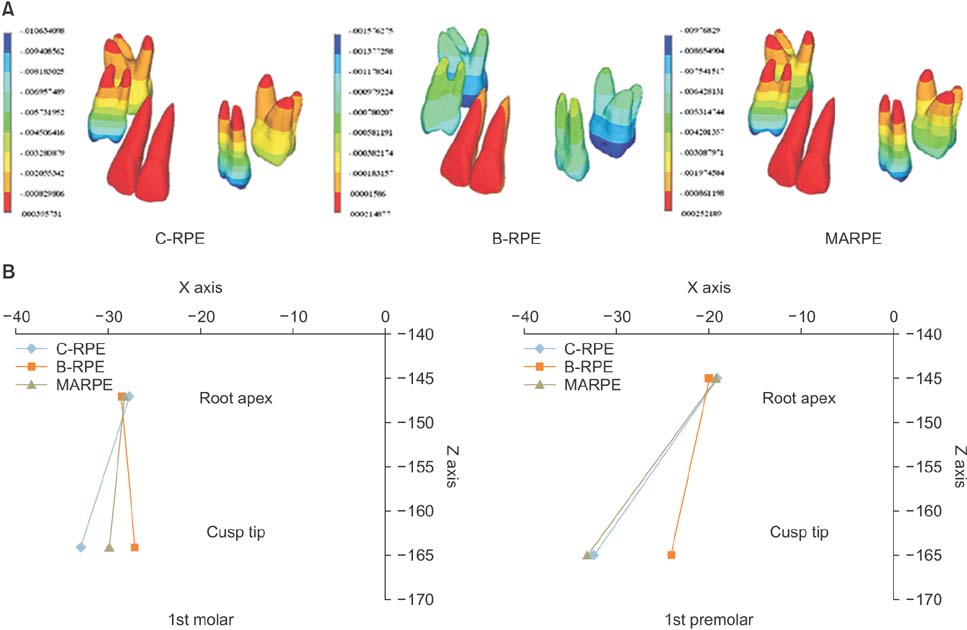
RESULTS
The results showed that C-RPE induced the greatest stress along the frontal process of the maxilla and around the anchor teeth, followed by the suture area, whereas B-RPE generated the greatest stress around the miniscrew, although the area was limited within the suture. Compared with the other appliances, MARPE caused relatively even stress distribution, decreased the stress on the buccal plate of the anchor teeth, and reduced tipping of the anchor teeth.
CONCLUSIONS
The findings of this study suggest that the incorporation of miniscrews in RPE devices may contribute to force delivery to the sutures and a decrease in excessive stress on the buccal plate. Thus, MARPE may serve as an effective modality for the nonsurgical treatment of transverse maxillary deficiency in young adults.
Figure
Cited by 4 articles
-
Stability of bimaxillary surgery involving intraoral vertical ramus osteotomy with or without presurgical miniscrew-assisted rapid palatal expansion in adult patients with skeletal Class III malocclusion
Yoon-Soo Ahn, Sung-Hwan Choi, Kee-Joon Lee, Young-Soo Jung, Hyoung-Seon Baik, Hyung-Seog Yu
Korean J Orthod. 2020;50(5):304-313. doi: 10.4041/kjod.2020.50.5.304.Influence of changing various parameters in miniscrew-assisted rapid palatal expansion: A three-dimensional finite element analysis
Soungjun Yoon, Dong-Yul Lee, Seok-Ki Jung
Korean J Orthod. 2019;49(3):150-160. doi: 10.4041/kjod.2019.49.3.150.Nonsurgical maxillary expansion in a 60-year-old patient with gingival recession and crowding
Harim Kim, Sun-Hyung Park, Jae Hyun Park, Kee-Joon Lee
Korean J Orthod. 2021;51(3):217-227. doi: 10.4041/kjod.2021.51.3.217.Short-term impact of microimplant-assisted rapid palatal expansion on the nasal soft tissues in adults: A three-dimensional stereophotogrammetry study
Seung-Ryeol Lee, Jin-woo Lee, Dong-Hwa Chung, Sang-min Lee
Korean J Orthod. 2020;50(2):75-85. doi: 10.4041/kjod.2020.50.2.75.
Reference
-
1. Angell EH. Treatment of irregularity of the permanent or adult teeth. Dent Cosmos. 1860; 1:540–544. 599–600.2. Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977; 72:42–52.
Article3. Melsen B, Melsen F. The postnatal development of the palatomaxillary region studied on human autopsy material. Am J Orthod. 1982; 82:329–342.
Article4. Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010; 137:830–839.
Article5. Melsen B. Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod. 1975; 68:42–54.6. Holm E, Persson RB. Radiochemical studies of 241Pu in Swedish reindeer lichens. Health Phys. 1977; 33:471–473.7. Wehrbein H, Yildizhan F. The mid-palatal suture in young adults. A radiological-histological investigation. Eur J Orthod. 2001; 23:105–114.
Article8. Handelman CS, Wang L, BeGole EA, Haas AJ. Nonsurgical rapid maxillary expansion in adults: report on 47 cases using the Haas expander. Angle Orthod. 2000; 70:129–144.9. Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 2015; 85:253–262.
Article10. Northway WM, Meade JB Jr. Surgically assisted rapid maxillary expansion: a comparison of technique, response, and stability. Angle Orthod. 1997; 67:309–320.11. Vanarsdall RL Jr. Transverse dimension and long-term stability. Semin Orthod. 1999; 5:171–180.
Article12. Song JW, Lim JK, Lee KJ, Sung SJ, Chun YS, Mo SS. Finite element analysis of maxillary incisor displacement during en-masse retraction according to orthodontic mini-implant position. Korean J Orthod. 2016; 46:242–252.
Article13. Lee HK, Bayome M, Ahn CS, Kim SH, Kim KB, Mo SS, et al. Stress distribution and displacement by different bone-borne palatal expanders with micro-implants: a three-dimensional finite-element analysis. Eur J Orthod. 2014; 36:531–540.
Article14. Tanne K, Hiraga J, Kakiuchi K, Yamagata Y, Sakuda M. Biomechanical effect of anteriorly directed extraoral forces on the craniofacial complex: a study using the finite element method. Am J Orthod Dentofacial Orthop. 1989; 95:200–207.
Article15. Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972; 62:296–309.
Article16. Coolidge ED. The thickness of the human periodontal membrane. J Am Dent Assoc Dent Cosm. 1937; 24:1260–1270.
Article17. Kronfeld R. Histologic study of the influence of function on the human periodontal membrane. J Am Dent Assoc. 1931; 18:1242–1274.
Article18. Provatidis CG, Georgiopoulos B, Kotinas A, McDonald JP. Evaluation of craniofacial effects during rapid maxillary expansion through combined in vivo/ in vitro and finite element studies. Eur J Orthod. 2008; 30:437–448.
Article19. Guan F, Han X, Mao H, Wagner C, Yeni YN, Yang KH. Application of optimization methodology and specimen-specific finite element models for investigating material properties of rat skull. Ann Biomed Eng. 2011; 39:85–95.
Article20. Zimring JF, Isaacson RJ. Forces produced by rapid maxillary expansion. 3. Forces present during retention. Angle Orthod. 1965; 35:178–186.21. Carvalho Trojan L, Andrés González-Torres L, Claudia Moreira Melo A, Barbosa de Las Casas E. Stresses and strains analysis using different palatal expander appliances in upper jaw and midpalatal Suture. Artif Organs. 2017; 41:E41–E51.
Article22. Koo YJ, Choi SH, Keum BT, Yu HS, Hwang CJ, Melsen B, et al. Maxillomandibular arch width differences at estimated centers of resistance: comparison between normal occlusion and skeletal Class III malocclusion. Korean J Orthod. 2017; 47:167–175.
Article23. Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016; 86:713–720.
Article24. Pickard MB, Dechow P, Rossouw PE, Buschang PH. Effects of miniscrew orientation on implant stability and resistance to failure. Am J Orthod Dentofacial Orthop. 2010; 137:91–99.
Article25. Frost HM. A 2003 update of bone physiology and Wolff's Law for clinicians. Angle Orthod. 2004; 74:3–15.26. Duyck J, Rønold HJ, Van Oosterwyck H, Naert I, Vander Sloten J, Ellingsen JE. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: an animal experimental study. Clin Oral Implants Res. 2001; 12:207–218.
Article27. Margulies SS, Thibault KL. Infant skull and suture properties: measurements and implications for mechanisms of pediatric brain injury. J Biomech Eng. 2000; 122:364–371.
Article28. Radhakrishnan P, Mao JJ. Nanomechanical properties of facial sutures and sutural mineralization front. J Dent Res. 2004; 83:470–475.
Article29. Verrue V, Dermaut L, Verhegghe B. Three-dimensional finite element modelling of a dog skull for the simulation of initial orthopaedic displacements. Eur J Orthod. 2001; 23:517–527.
Article30. Tanne K, Hiraga J, Sakuda M. Effects of directions of maxillary protraction forces on biomechanical changes in craniofacial complex. Eur J Orthod. 1989; 11:382–391.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of changing various parameters in miniscrew-assisted rapid palatal expansion: A three-dimensional finite element analysis
- Three dimensional finite element method for stress distribution on the length and diameter of orthodontic miniscrew and cortical bone thickness
- Factors influencing primary stability of miniplate anchorage: a three-dimensional finite element analysis
- Stress distributions in peri-miniscrew areas from cylindrical and tapered miniscrews inserted at different angles
- A study on the stress analysis of three root-form implants with finite element analysis