J Neurocrit Care.
2017 Dec;10(2):107-111. 10.18700/jnc.170015.
Aneurysmal Subarachnoid Hemorrhage Following Intravenous Thrombolysis in Acute Ischemic Stroke
- Affiliations
-
- 1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sbjeonmd@gmail.com
- KMID: 2405765
- DOI: http://doi.org/10.18700/jnc.170015
Abstract
- BACKGROUND
An incidental finding of unruptured aneurysm, which is a contraindication to the recombinant tissue plasminogen activator (rtPA), is common in patients with acute ischemic strokes. However, reports describing the rupture of intracranial aneurysm following the administration of rtPA are extremely rare.
CASE REPORT
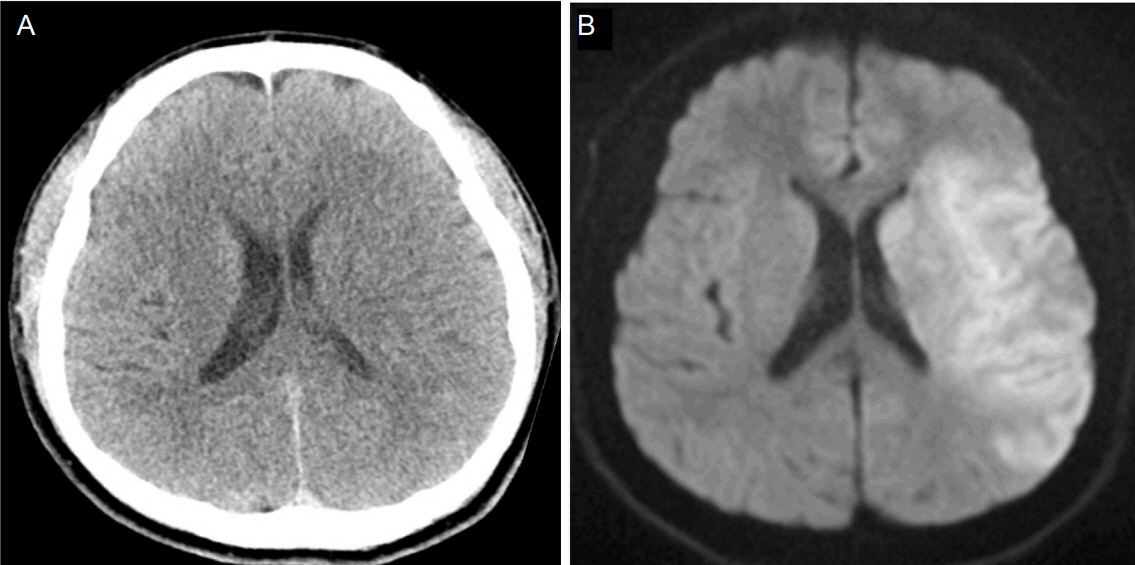
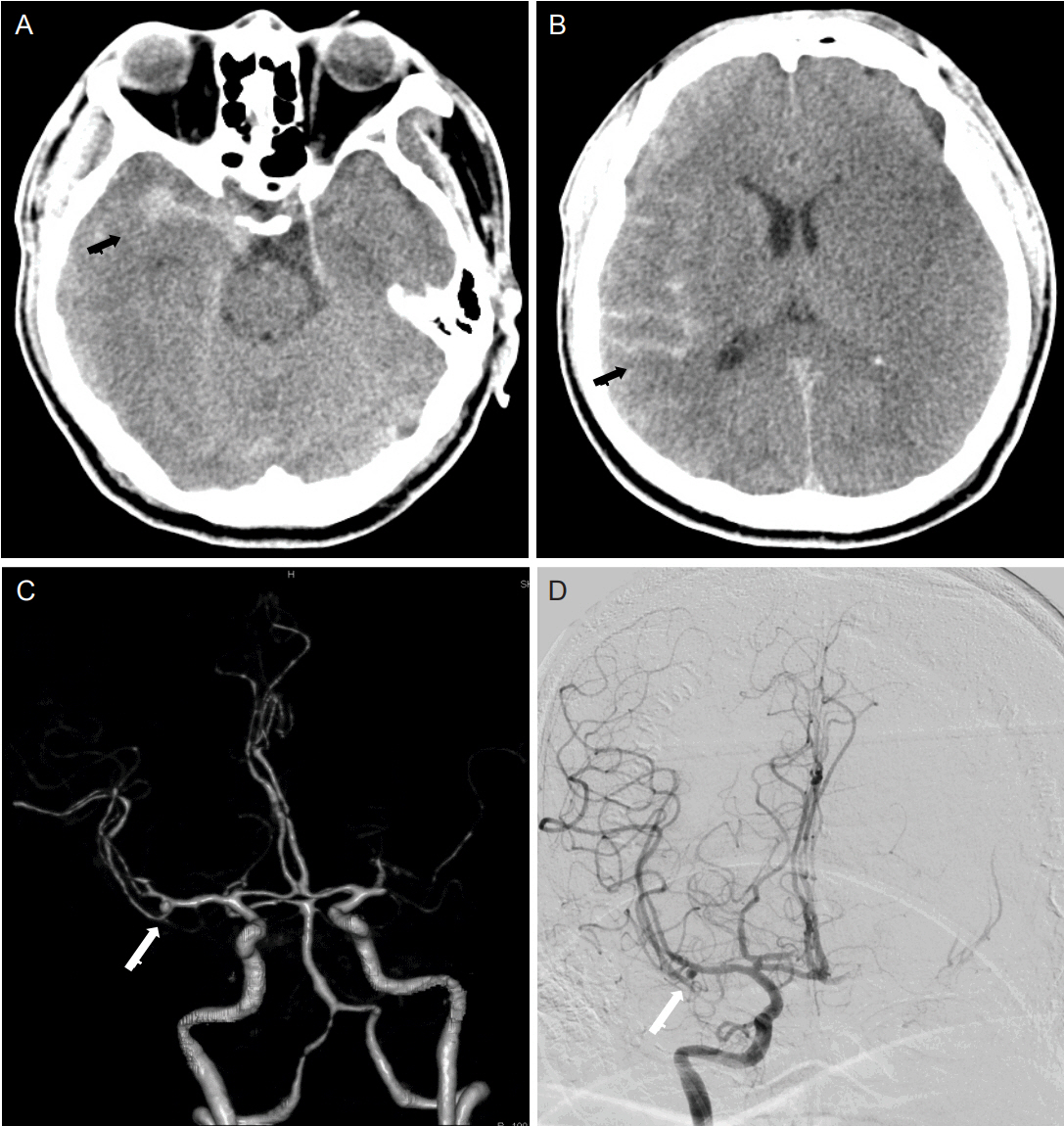
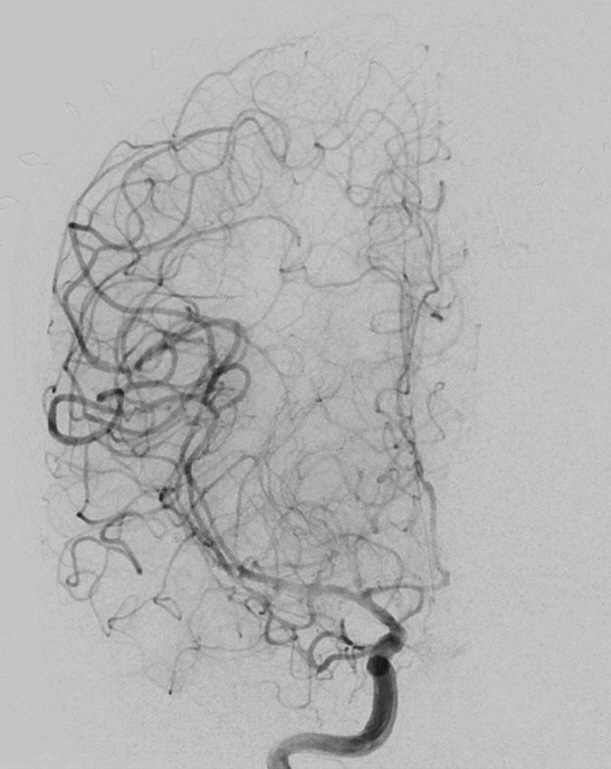
A 51-year-old man presented to the emergency room with global aphasia. A computed tomography (CT) of the brain revealed no intracranial hemorrhage. Since global aphasia occurred in an hour, rtPA was administrated intravenously. A CT angiography was performed 2 hours after an infusion of rtPA, which despite the absence of neurological deterioration and blood pressure surge, revealed subarachnoid hemorrhage in the right cerebral hemisphere, in addition to a 3-mm saccular aneurysm with a bleb in the right middle cerebral artery.
CONCLUSIONS
Aneurysmal subarachnoid hemorrhage can develop following the infusion of rtPA. Hence, unruptured aneurysm may not simply be an "incidental finding" in stroke patients receiving rtPA.
MeSH Terms
-
Aneurysm*
Angiography
Aphasia
Blister
Blood Pressure
Brain
Cerebral Infarction
Cerebrum
Emergency Service, Hospital
Humans
Incidental Findings
Intracranial Aneurysm
Intracranial Hemorrhages
Middle Aged
Middle Cerebral Artery
Rupture
Stroke*
Subarachnoid Hemorrhage*
Thrombolytic Therapy
Tissue Plasminogen Activator
Tissue Plasminogen Activator
Figure
Reference
-
1. Edwards NJ, Kamel H, Josephson SA. The safety of intravenous thrombolysis for ischemic stroke in patients with preexisting cerebral aneurysms: a case series and review of the literature. Stroke. 2012; 43:412–6.
Article2. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol. 2011; 10:626–36.
Article3. Oh YS, Lee SJ, Shon YM, Yang DW, Kim BS, Cho AH. Incidental unruptured intracranial aneurysms in patients with acute ischemic stroke. Cerebrovasc Dis. 2008; 26:650–3.
Article4. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.5. Goyal N, Tsivgoulis G, Zand R, Sharma VK, Barlinn K, Male S, et al. Systemic thrombolysis in acute ischemic stroke patients with unruptured intracranial aneurysms. Neurology. 2015; 85:1452–8.
Article6. Sheth KN, Shah N, Morovati T, Hermann LD, Cronin CA. Intravenous rt-PA is not associated with increased risk of hemorrhage in patients with intracranial aneurysms. Neurocritical Care. 2012; 17:199–203.
Article7. Mittal MK, Seet RC, Zhang Y, Brown RD Jr, Rabinstein AA. Safety of intravenous thrombolysis in acute ischemic stroke patients with saccular intracranial aneurysms. J Stroke Cere brovasc Dis. 2013; 22:639–43.
Article8. Rammos SK, Neils DM, Fraser K, Klopfenstein JD. Anterior communicating artery aneurysm rupture after intravenous thrombolysis for acute middle cerebral artery thromboembolism: case report. Neurosurgery. 2012; 70:E1603–7. discussion E1607.9. Haji F, van Adel BV, Avery M, Megyesi J, Young GB. Intracranial aneurysm rupture following intravenous thrombolysis for stroke. Can J Neurol Sci. 2014; 41:95–8.
Article10. Briosa E Gala D, Almeida A, Monteiro N, Paiva Nunes A, Ferreira P, Mendonça N, et al. Successful Thrombolysis despite Having an Incidental Unruptured Cerebral Aneurysm. Case Rep Neurol Med. 2014; 2014:323049.
Article11. Yoo SH, Kwon SU, Lee DH, Kim SJ, Kim JS, Kang DW. Comparison between MRI screening and CT-plus-MRI screening for thrombolysis within 3 h of ischemic stroke. J Neurol Sci. 2010; 294:119–23.12. Lagares A, Gómez PA, Lobato RD, Alén JF, Campollo J, Benito-León J. Cerebral aneurysm rupture after r-tPA thrombolysis for acute myocardial infarction. Surg Neurol. 1999; 52:623–6.
Article13. Chalouhi N, Hoh BL, Hasan D. Review of cerebral aneurysm formation, growth, and rupture. Stroke. 2013; 44:3613–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Terson Syndrome after Subarachnoid Hemorrhage Occurred by Thrombolysis and Mechanical Thrombectomy to Treat Acute Ischemic Stroke: A Case Report
- Treatment of Acute Ischemic Stroke: Thrombolysis
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Cerebrovascular Disease : Overview and Classification
- A ruptured aneurysmal subarachnoid hemorrhage and vasospasm initially manifesting as acute ischemic stroke: a case report