J Korean Soc Radiol.
2018 Mar;78(3):200-211. 10.3348/jksr.2018.78.3.200.
Lesions that Mimic Musculoskeletal Infection: A Pictorial Essay
- Affiliations
-
- 1Department of Radiology, Kyung Hee University Hospital, College of Medicine, Kyung Hee University, Seoul, Korea. t2star@naver.com
- 2Department of Radiology, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 2405723
- DOI: http://doi.org/10.3348/jksr.2018.78.3.200
Abstract
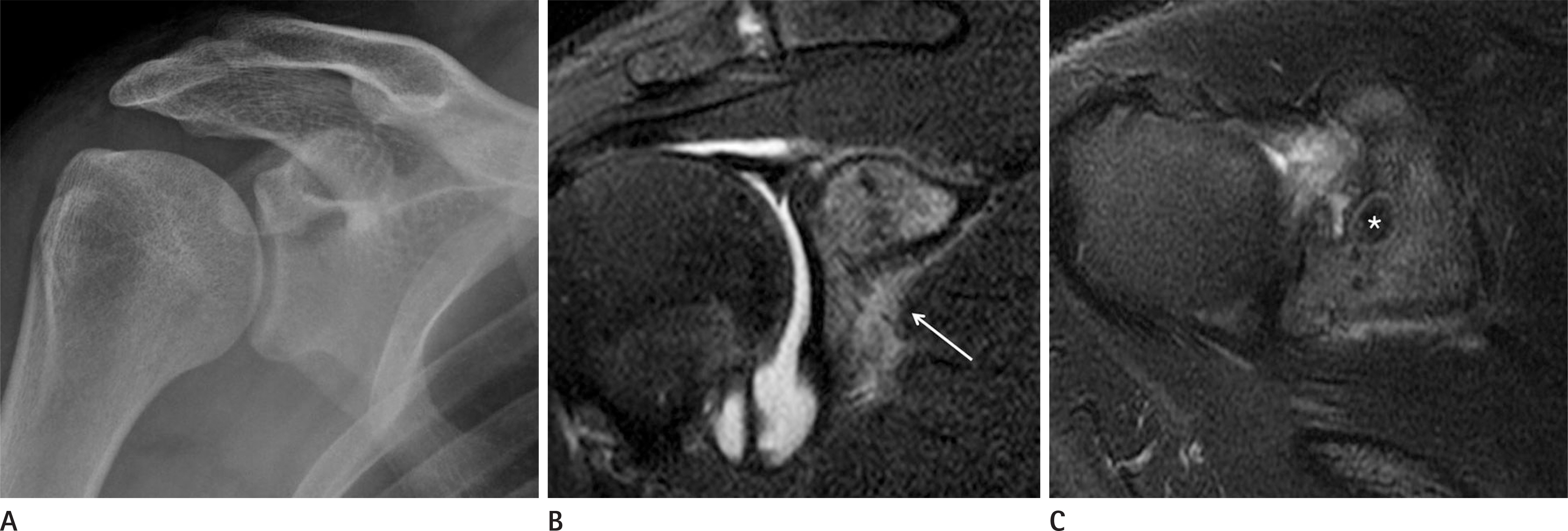
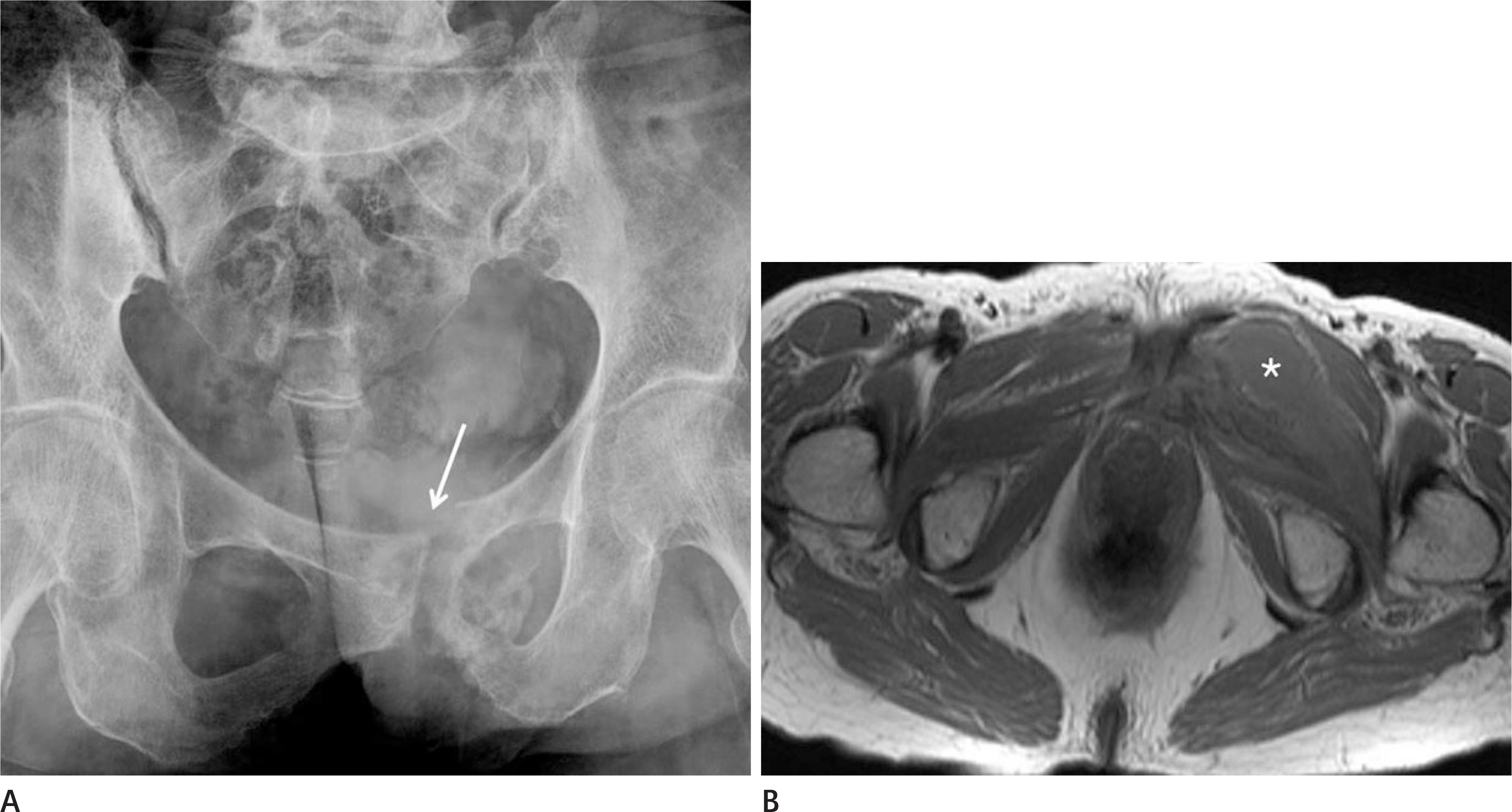
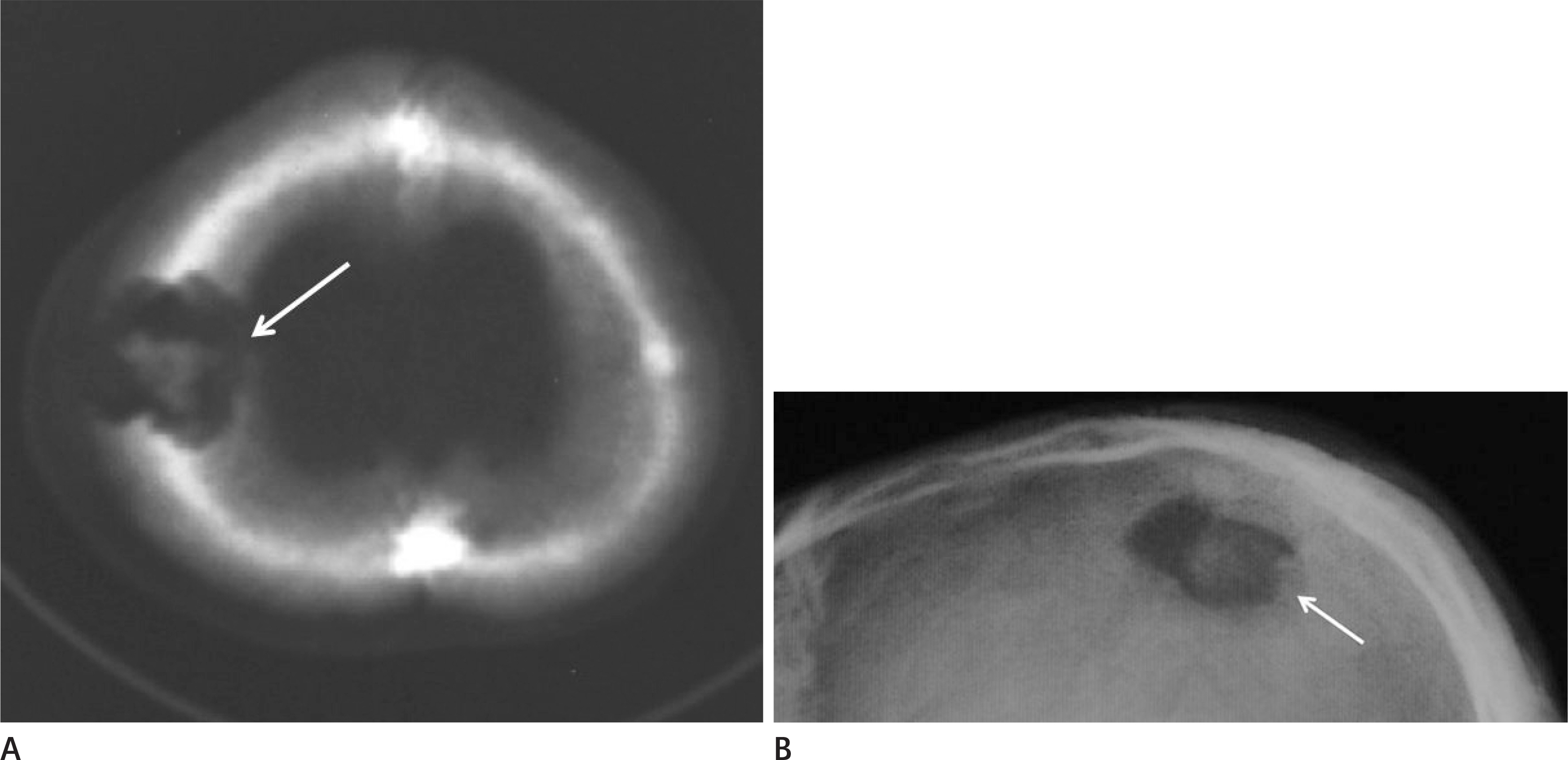
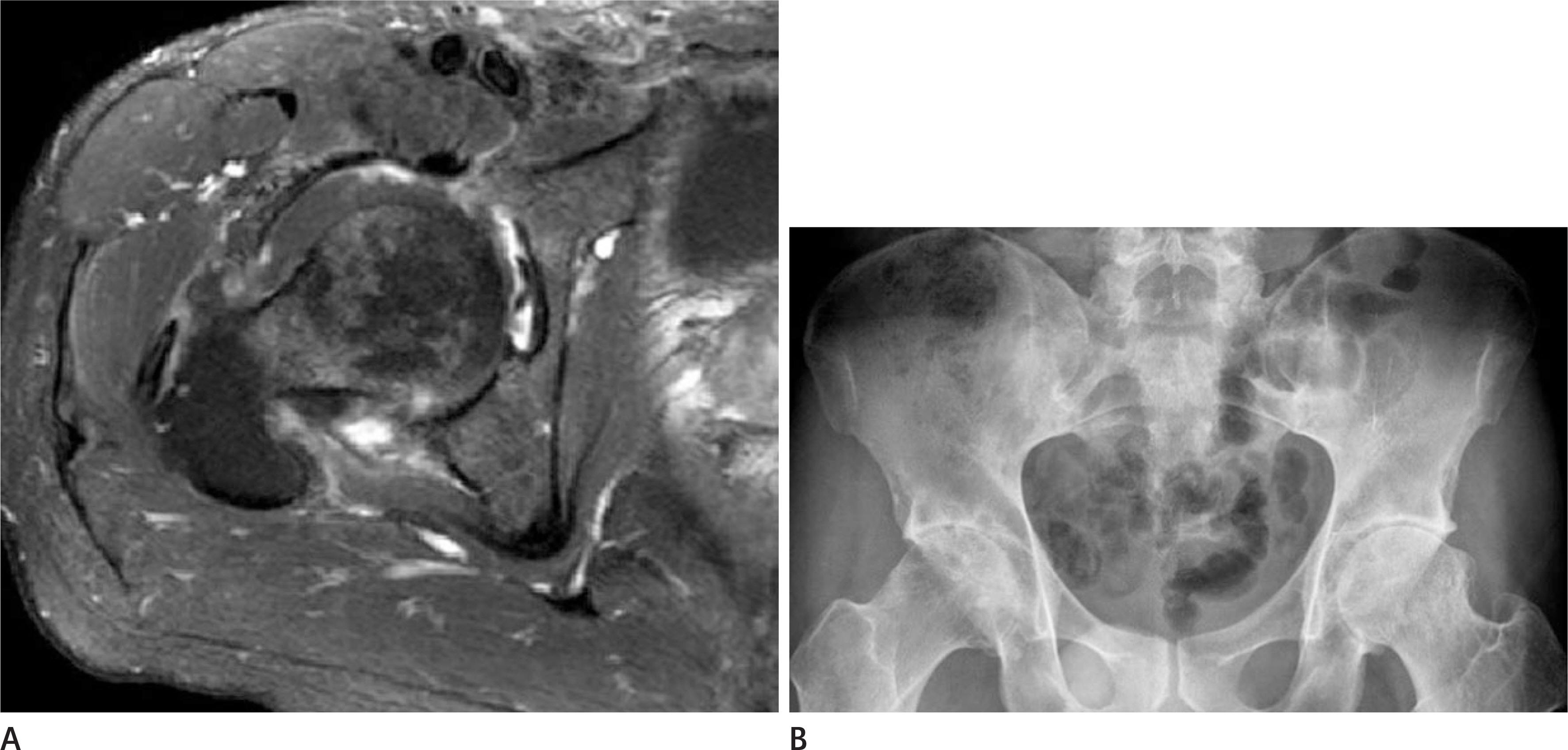
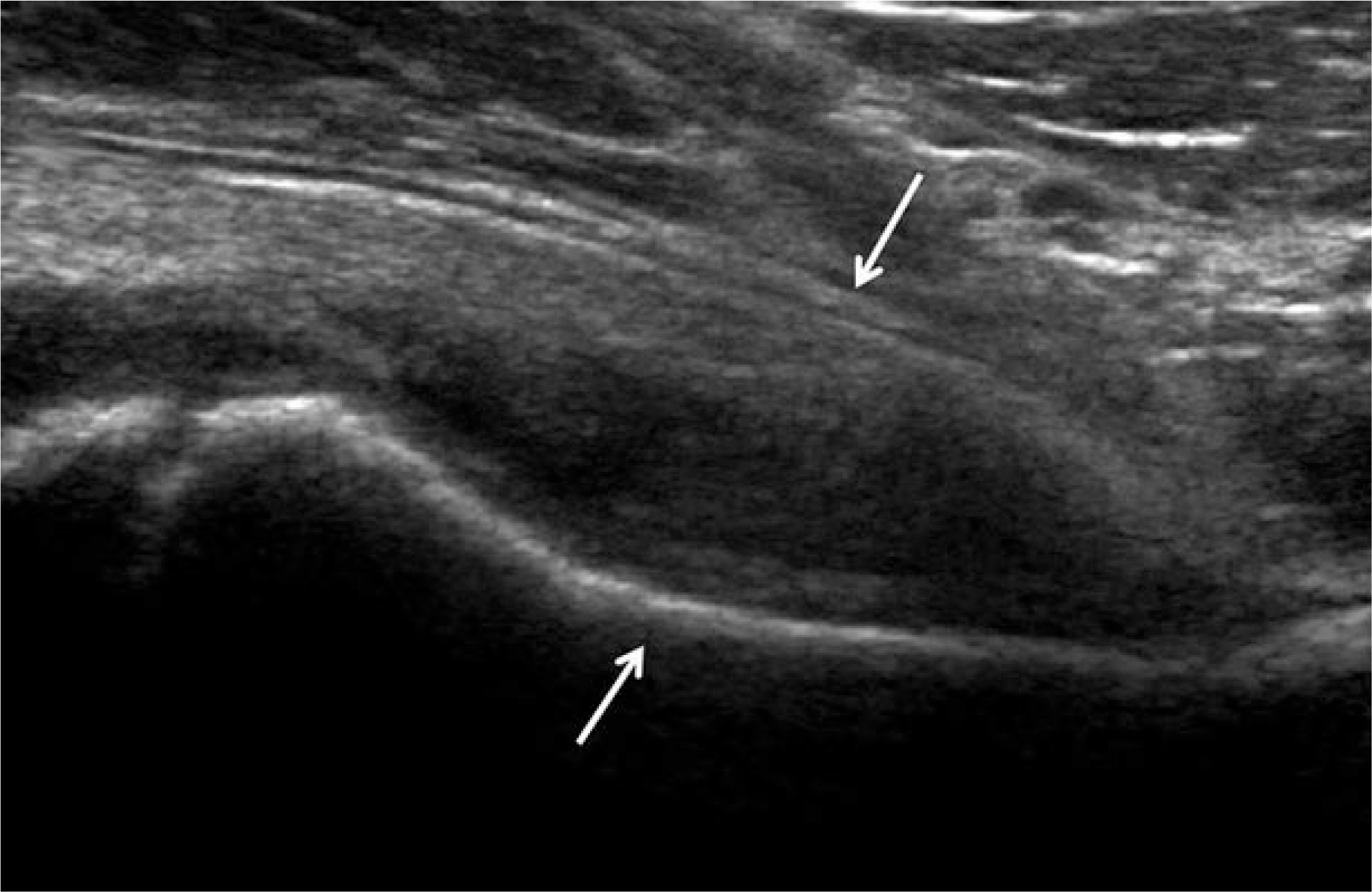
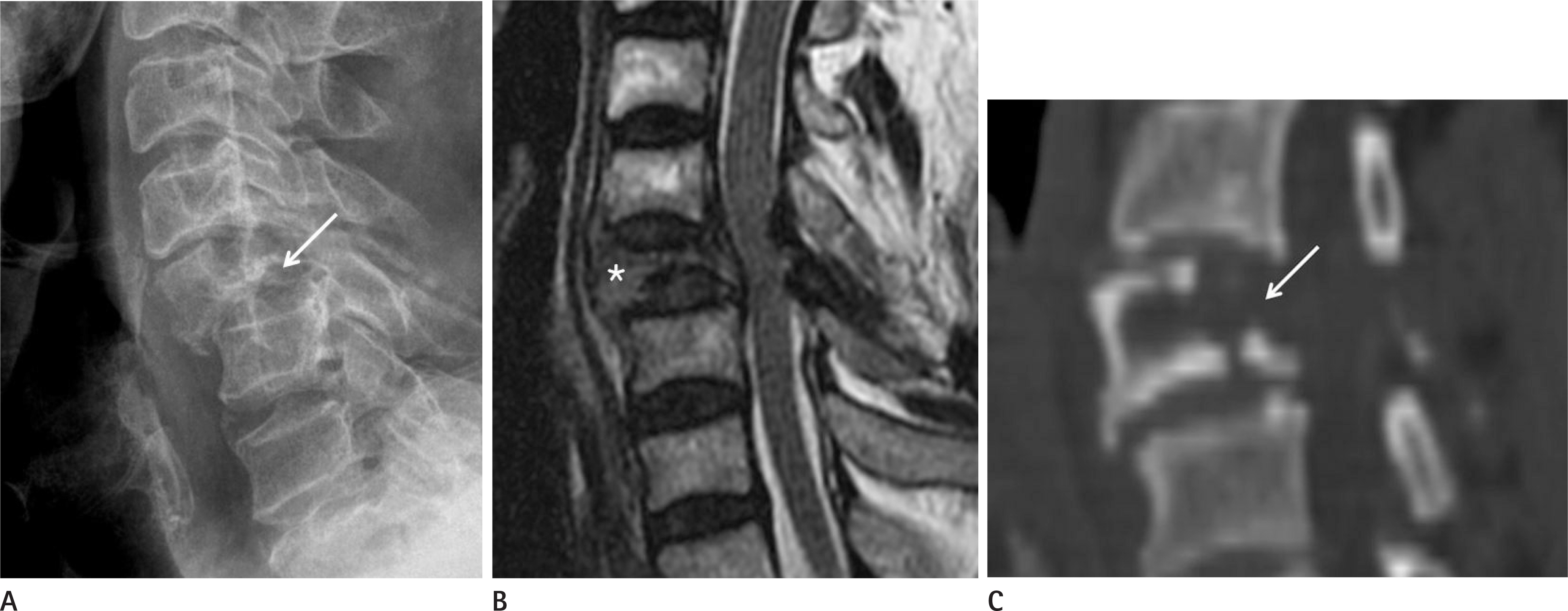
- Musculoskeletal (MSK) infections, such as osteomyelitis, infectious arthritis and spondylitis have variable radiographic findings depending on their underlying cause and clinical infection stage. Other disease entities, ranging from simple degenerative lesions to tumorous bone conditions, in which there is no evidence of infectious origin, can share similar radiographic findings. It is important to be aware, when interpreting radiographic features that are typically associated with MSK infections, that a non-infectious MSK disease may be mimicking the radiographic findings of infectious diseases.
MeSH Terms
Figure
Reference
-
References
1. Poultsides LA, Liaropoulos LL, Malizos KN. The socioeconomic impact of musculoskeletal infections. J Bone Joint Surg Am. 2010; 92:e13.
Article2. Manaster BJ. Diagnostic imaging: musculoskeletal non-traumatic disease. Philadelphia, PA: Elsevier Health Sciences;2016.3. Resnick D. Osteomyelitis, septic arthritis, and soft tissue infection: organisms. In Resnick D, ed. Bone and Joint Imaging. Philadelphia, PA: Saunders;2006. p. 753–788.4. Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009; 23:80–89.
Article5. Peh WC, Khong PL, Yin Y, Ho WY, Evans NS, Gilula LA, et al. Imaging of pelvic insufficiency fractures. Radiographics. 1996; 16:335–348.
Article6. Hayes CS, Heinrich SD, Craver R, MacEwen GD. Subacute osteomyelitis. Orthopedics. 1990; 13:363–366.
Article7. Mhuircheartaigh JN, Lin YC, Wu JS. Bone tumor mimickers: a pictorial essay. Indian J Radiol Imaging. 2014; 24:225–236.
Article8. Khung S, Budzik JF, Amzallag-Bellenger E, Lambilliote A, Soto Ares G, Cotten A, et al. Skeletal involvement in Langerhans cell histiocytosis. Insights Imaging. 2013; 4:569–579.
Article9. Kaul R, Gupta N, Gupta S, Gupta M. Eosinophilic granuloma of skull bone. J Cytol. 2009; 26:156–157.
Article10. Joo I, Choi JA, Chung JH, Oh JH, Hong SH, Kang HS. Fibroblastic type osteosarcoma of the ulna: a case report of a tumor in a rare location with atypical imaging findings. Korean J Radiol. 2009; 10:85–88.
Article11. Sundaram M, Totty WG, Kyriakos M, McDonald DJ, Merkel K. Imaging findings in pseudocystic osteosarcoma. AJR Am J Roentgenol. 2001; 176:783–788.
Article12. Perron AD, Brady WJ, Miller MD. Orthopedic pitfalls in the ED: osteomyelitis. Am J Emerg Med. 2003; 21:61–67.
Article13. Khanna G, Sato TSP, Ferguson P. Imaging of chronic recurrent multifocal osteomyelitis. Radiographics. 2009; 29:1159–1177.
Article14. Giurato L, Uccioli L. The diabetic foot: Charcot joint and osteomyelitis. Nucl Med Commun. 2006; 27:745–749.
Article15. Vander Cruyssen B, Muñoz-Gomariz E, Font P, Mulero J, de Vlam K, Boonen A, et al. ASPECT-REGISPONSER-RESPON-DIA working group. Hip involvement in ankylosing spondylitis: epidemiology and risk factors associated with hip replacement surgery. Rheumatology (Oxford). 2010; 49:73–81.
Article16. Jeong H, Eun YH, Kim IY, Kim H, Lee J, Koh EM, et al. Characteristics of hip involvement in patients with ankylosing spondylitis in Korea. Korean J Intern Med. 2017; 32:158–164.
Article17. Hong SH, Choi JY, Lee JW, Kim NR, Choi JA, Kang HS. MR imaging assessment of the spine: infection or an imitation? Radiographics. 2009; 29:599–612.
Article18. Shah LM, Salzman KL. Imaging of spinal metastatic disease. Int J Surg Oncol. 2011; 2011:769753.
Article19. Khattry N, Thulkar S, Das A, Khan SA, Bakhshi S. Spinal tuberculosis mimicking malignancy: atypical imaging features. Indian J Pediatr. 2007; 74:297–298.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Musculoskeletal Applications of Elastography: a Pictorial Essay of Our Initial Experience
- RE: Musculoskeletal Applications of Elastography: a Pictorial Essay of Our Initial Experience
- Incidental Musculoskeletal Lesions Detected on Abdominopelvic CT Scans: A Pictorial Essay
- Imaging Features of the Mesenchymal Tumors of the Breast according to WHO Classification: A Pictorial Essay
- Breast lesions during pregnancy and lactation: a pictorial essay