J Korean Orthop Assoc.
2018 Feb;53(1):29-37. 10.4055/jkoa.2018.53.1.29.
The Effect of Screw Apophysiodesis of Greater Trochanter in Legg-Calve-Perthes Disease
- Affiliations
-
- 1Department of Orthopedic Surgery, Dong-A University College of Medicine, Busan, Korea. hyeonjun@dau.ac.kr
- 2The 22nd Infantry Division of Republic of Korea Army, Goseong, Korea.
- KMID: 2405396
- DOI: http://doi.org/10.4055/jkoa.2018.53.1.29
Abstract
- PURPOSE
To evaluate the interstitial and appositional growth of greater trochanter post-screw apophysiodesis in Legg-Calve-Perthes (LCP) disease.
MATERIALS AND METHODS
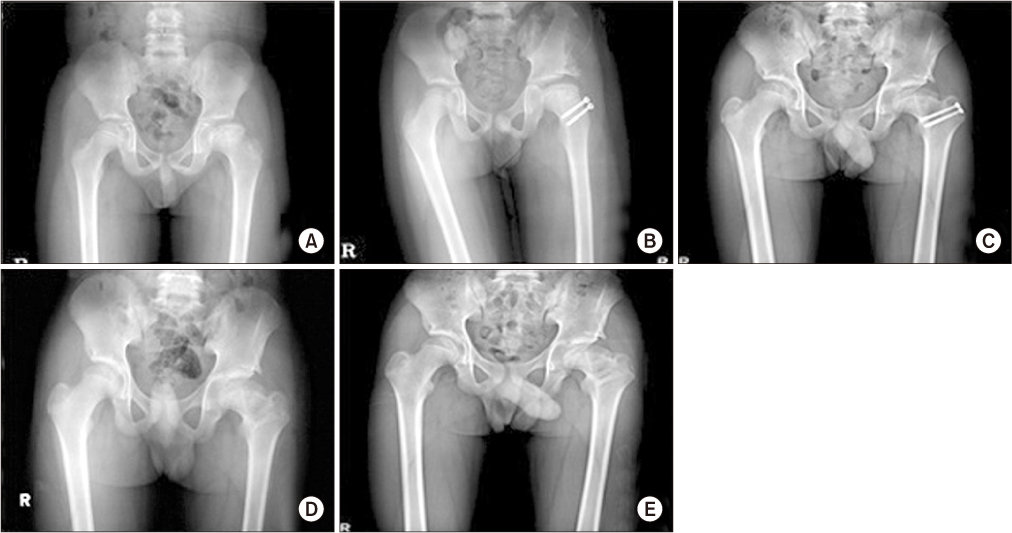
A total of 17 patients, who were diagnosed with LCP and underwent greater trochanter screw apophysiodesis and metal removal between December 2003 and December 2012, and were followed-up for at least 4 years, were selected. Anterioposterior radiologic images were taken in each process of apophysiodesis, metal removal, and last follow-up. From such images, articulotrochanter tip distance (ATD), trochanter tip-screw distance (TSD), trochanter tip-trochanter lower margin distance (TLD), and screw-trochanter lower margin distance (SLD) were measured. Appositional growth and greater trochanter growth rates were compared using paired t-test, independent t-test, and correlation analysis.
RESULTS
The average ATD of the affected and unaffected sides was 14.2 and 16.8 mm, respectively at apophysiodesis and 9.2 and 14.8 mm at the last follow-up, with a significantly greater decrease observed on the affected side the unaffected side (p=0.030). TLD of the affected side during the follow-up increased 11.0 mm, from an average of 30.8 to 41.8 mm, while the un-affected side increased 14.3 mm, from an average of 26.7 to 41.0 mm. The growth of greater trochanter after the operation in the affected side was 76.7% of that in unaffected side. The ratio of TLD of the affected side to the unaffected side was significantly reduced, from 1.15 to 1.02 (p=0.014) at the final follow-up. TSD was significantly increased from 4.5 to 14.4 mm at metal removal (p < 0.001) and increased to 17.0 mm at the last follow-up. Moreover, the ratio of TSD to SLD was significantly increased from 0.20 to 0.74 at metal removal (p < 0.001) and increased to 0.84 at the final follow-up.
CONCLUSION
The results of this study showed that screw apophysiodesis can suppress the overall growth, but not the appositional growth of the greater trochanter. Therefore, screw apophysiodesis may not be a good procedure to inhibit the growth of greater trochanter.
Figure
Reference
-
1. Van Tongel A, Fabry G. Epiphysiodesis of the greater trochanter in Legg-Calvé-Perthes disease: the importance of timing. Acta Orthop Belg. 2006; 72:309–313.2. Matan AJ, Stevens PM, Smith JT, Santora SD. Combination trochanteric arrest and intertrochanteric osteotomy for Perthes' disease. J Pediatr Orthop. 1996; 16:10–14.
Article3. Maquet P. Importance of the position of the greater trochanter. Acta Orthop Belg. 1990; 56:307–322.4. Iwersen LJ, Kalen V, Eberle C. Relative trochanteric overgrowth after ischemic necrosis in congenital dislocation of the hip. J Pediatr Orthop. 1989; 9:381–385.
Article5. Leitch JM, Paterson DC, Foster BK. Growth disturbance in Legg-Calvé-Perthes disease and the consequences of surgical treatment. Clin Orthop Relat Res. 1991; (262):178–184.
Article6. Gage JR, Cary JM. The effects of trochanteric epiphyseodesis on growth of the proximal end of the femur following necrosis of the capital femoral epiphysis. J Bone Joint Surg Am. 1980; 62:785–794.
Article7. Litt R, Albassir A, Willems S, Debry R. Coxa vara. Isolated growth of the greater trochanter. Prevention-treatment. Acta Orthop Belg. 1990; 56:301–306.8. Garrido IM, Moltó FJ, Lluch DB. Distal transfer of the greater trochanter in acquired coxa vara. Clinical and radiographic results. J Pediatr Orthop B. 2003; 12:38–43.
Article9. Takata K, Maniwa S, Ochi M. Surgical treatment of high-standing greater trochanter. Arch Orthop Trauma Surg. 1999; 119:461–463.
Article10. Hasler CC, Morscher EW. Femoral neck lengthening osteotomy after growth disturbance of the proximal femur. J Pediatr Orthop B. 1999; 8:271–275.
Article11. Fernbach SK, Poznanski AK, Kelikian AS, Tachjdian MO, Marzano MJ. Greater trochanteric overgrowth: development and surgical correction. Radiology. 1985; 154:661–664.
Article12. Schneidmueller D, Carstens C, Thomsen M. Surgical treatment of overgrowth of the greater trochanter in children and adolescents. J Pediatr Orthop. 2006; 26:486–490.
Article13. Edgren W. Coxa plana. A clinical and radiological investigation with particular reference to the importance of the metaphyseal changes for the final shape of the proximal part of the femur. Acta Orthop Scand Suppl. 1965; Suppl 84. 1–129.14. Langenskiöld A, Salenius P. Epiphyseodesis of the greater trochanter. Acta Orthop Scand. 1967; 38:199–219.
Article15. McCarthy JJ, Weiner DS. Greater trochanteric epiphysiodesis. Int Orthop. 2008; 32:531–534.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Observation of the Legg-Calve-Perthes Disease: Preliminary Report
- Legg - Calve Perthes disease in Monozygotic Male Twins
- Osteochondritis Dissecans of Femoral Head Following Legg-Calve-Perthes Disease
- Innominate Osteotomy in Legg-Calve-Perthes Disease
- Late Complications of Legg-Calve-Perthes Disease