J Dent Anesth Pain Med.
2018 Feb;18(1):41-46. 10.17245/jdapm.2018.18.1.41.
Effect of relative head position on the anesthetic efficacy of inferior alveolar nerve block during endodontic treatment of patients with irreversible pulpitis
- Affiliations
-
- 1Department of Conservative Dentistry & Endodontics, Faculty of Dentistry, Jamia Millia Islamia, New Delhi, India. drvivekaggarwal@gmail.com
- 2Department of Conservative Dentistry & Endodontics, SGT Dental College, Gurgaon, India.
- KMID: 2405382
- DOI: http://doi.org/10.17245/jdapm.2018.18.1.41
Abstract
- BACKGROUND
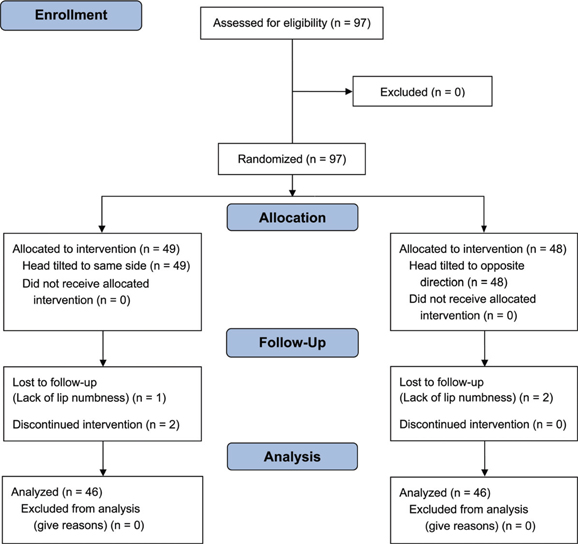
The purpose of this prospective randomized single-blind clinical trial was to evaluate the effect of tilting the head on the anesthetic efficacy of inferior alveolar nerve block (IANB) in patients with symptomatic irreversible pulpitis.
METHODS
Ninety-two patients were divided into two groups: the first group received IANB and the head was tilted in the direction of the block for 15 min, whereas the second group received IANB and the head was tilted to the opposite side. Access cavity preparation was initiated after 15 min. Success was defined as no pain or faint/weak/mild pain during endodontic access preparation and instrumentation. The anesthetic success rates were analyzed by Pearson chi-square test at 5% significance levels.
RESULTS
The same side position and opposite side position yielded 41% and 30% anesthetic success rates, respectively; there was no significant difference between the two sides.
CONCLUSIONS
Relative head position has no effect on the anesthetic success rate of IANB.
Keyword
MeSH Terms
Figure
Reference
-
1. Hargreaves KM, Keiser K. Local anesthetic failure in endodontics: mechanisms and management. Endod Topics. 2002; 1:26–39.2. Khoury JN, Mihailidis S, Ghabriel M, Townsend G. Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Aust Dent J. 2011; 56:112–121.
Article3. Raymond SA, Steffensen SC, Gugliano LD, Strichartz GR. The role of length of nerve exposed to local anesthetics in impulse blocking action. Anesth Analg. 1989; 68:563–570.
Article4. Rucci F, Pippa P, Boccaccini A, Barbagli R. Effect of injection speed on anaesthetic spread during axillary block using the orthogonal two-needle technique. Eur J Anaesthesiol. 1995; 12:505–511.5. Kanaa MD, Meechan JG, Corbett IP, Whitworth JM. Speed of injection influences efficacy of inferior alveolar nerve blocks: a double-blind randomized controlled trial in volunteers. J Endod. 2006; 32:919–923.
Article6. Aggarwal V, Singla M, Miglani S, Kohli S, Irfan M. A prospective, randomized single-blind evaluation of effect of injection speed on anesthetic efficacy of inferior alveolar nerve block in patients with symptomatic irreversible pulpitis. J Endod. 2012; 38:1578–1580.
Article7. Whitworth JM, Kanaa MD, Corbett IP, Meechan JG. Influence of injection speed on the effectiveness of incisive/mental nerve block: a randomized, controlled, doubleblind study in adult volunteers. J Endod. 2007; 33:1149–1154.
Article8. Ridenour S, Reader A, Beck M, Weaver J. Anesthetic efficacy of a combination of hyaluronidase and lidocaine with epinephrine in inferior alveolar nerve blocks. Anesth Prog. 2001; 48:9–15.9. Wohlrab J, Finke R, Franke WG, Wohlrab A. Efficacy study of hyaluronidase as a diffusion promoter for lidocaine in infiltration analgesia of skin. Plast Reconstr Surg. 2012; 129:771e–772e.
Article10. Remy M, Pinter F, Nentwich MM, Kampik A, Schönfeld CL. Efficacy and safety of hyaluronidase 75 IU as an adjuvant to mepivacaine for retrobulbar anesthesia in cataract surgery. J Cataract Refract Surg. 2008; 34:1966–1969.
Article11. Tempestini Horliana AC, de Brito MA, Perez FE, Simonetti MP, Rocha RG, Borsatti MA. Hyaluronidase increases the duration of mepivacaine in inferior alveolar nerve blocks. J Oral Maxillofac Surg. 2008; 66:286–290.
Article12. Loubert C, Hallworth S, Fernando R, Columb M, Patel N, Sarang K, Sodhi V. Does the baricity of bupivacaine influence intrathecal spread in the prolonged sitting position before elective cesarean delivery? A prospective randomized controlled study. Anesth Analg. 2011; 113:811–817.
Article13. Yang MK, Kim JA, Ahn HJ, Choi DH. Influence of the baricity of a local anaesthetic agent on sedation with propofol during spinal anaesthesia. Br J Anaesth. 2007; 98:515–518.
Article14. Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JA. Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth. 2005; 94:107–111.
Article15. Stienstra R, Gielen M, Kroon JW, Van Poorten F. The influence of temperature and speed of injection on the distribution of a solution containing bupivacaine and methylene blue in a spinal canal model. Reg Anesth. 1990; 15:6–11.16. Aggarwal V, Jain A, Kabi D. Anesthetic efficacy of supplemental buccal and lingual infiltrations of articaine and lidocaine following an inferior alveolar nerve block in patients with irreversible pulpitis. J Endod. 2009; 35:925–929.
Article17. Heft MW, Parker SR. An experimental basis for revising the graphic rating scale for pain. Pain. 1984; 19:153–161.
Article18. McCartney M, Reader A, Beck M. Injection pain of the inferior alveolar nerve block in patients with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:571–575.
Article19. Aggarwal V, Singla M, Rizvi A, Miglani S. Comparative evaluation of local infiltration of articaine, articaine plus ketorolacand dexamethasone on anesthetic efficacy of inferior alveolar nerve block with lidocaine in patients with irreversible pulpitis. J Endod. 2011; 37:445–449.
Article20. Takeuchi T, Tasaki I. Ubertrangung de nervenimpulses in der polarisierten nervenfaser. Pfluegers Arch Gesamte Physiol Menshchen Tiere. 1942; 246:32–43.21. Coleman RD, Smith RA. The anatomy of mandibular anesthesia: review and analysis. Oral Surg Oral Med Oral Pathol. 1982; 54:148–153.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anesthetic efficacy of Gow-Gates versus inferior alveolar nerve block for irreversible pulpitis: a systematic quantitative review
- Efficacy of buccal piroxicam infiltration and inferior alveolar nerve block in patients with irreversible pulpitis: a prospective, double-blind, randomized clinical trial
- Photobiomodulation by soft laser irradiation with and without ibuprofen improves success rate of inferior alveolar nerve block using 2% lignocaine with adrenaline in symptomatic irreversible pulpitis of mandibular molar teeth: a double-blind, randomized placebo-controlled trial
- Addition of 2 mg dexamethasone to improve the anesthetic efficacy of 2% lidocaine with 1:80,000 epinephrine administered for inferior alveolar nerve block to patients with symptomatic irreversible pulpitis in the mandibular molars: a randomized double-blind clinical trial
- Assessment of the effect of premedication on the success of inferior alveolar nerve block in tobacco chewing patients with symptomatic irreversible pulpitis: a randomized control trial