Ann Surg Treat Res.
2018 Mar;94(3):147-153. 10.4174/astr.2018.94.3.147.
Comparison of the short-term outcomes of reduced-port laparoscopic surgery and conventional multiport surgery in colon cancer: a propensity score matching analysis
- Affiliations
-
- 1Department of Surgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea. kimyjin@jnu.ac.kr
- 2Department of Surgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2405327
- DOI: http://doi.org/10.4174/astr.2018.94.3.147
Abstract
- PURPOSE
The feasibility of reduced-port laparoscopic surgery (RPS) in colon cancer remains uncertain. This study aimed to compare the short-term outcomes of RPS and multiport surgery (MPS) in colon cancer using propensity score matching analysis.
METHODS
A total of 302 patients with colon cancer who underwent laparoscopic anterior resection (AR) (n = 184) or right hemicolectomy (RHC) (n = 118) by a single surgeon between January 2011 and January 2017 were included. Short-term outcomes were compared between RPS and MPS.
RESULTS
Seventy-three patients in the AR group and 23 in the RHC group underwent RPS. After propensity score matching, the RPS and MPS groups showed similar baseline characteristics. In the AR group, patients who underwent RPS (n = 72) showed a shorter operation time (114.4 ± 28.7 minutes vs. 126.7 ± 34.5 minutes, P = 0.021) and a longer time to gas passage (3.6 ± 1.7 days vs. 2.6 ± 1.5 days, P = 0.005) than MPS (n = 72). Similarly, in the RHC group, the operation time was shorter (112.6 ± 26.0 minutes vs. 146.5 ± 31.2 minutes, P = 0.005), and the time to first flatus was longer (2.7 ±1.1 days vs. 3.8 ± 1.3 days, P = 0.004) in the RPS group (n = 23) than in the MPS group (n = 23). Other short-term outcomes were similar for RPS and MPS in both the AR and RHC groups.
CONCLUSION
The short-term outcomes of RPS were found to be acceptable compared to those of MPS in colon cancer surgery.
Keyword
MeSH Terms
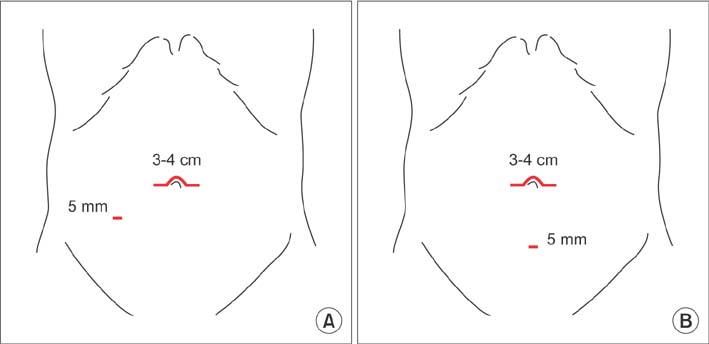
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017; 67:7–30.
Article2. Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017; 49:292–305.
Article3. Law WL, Chu KW, Tung PH. Laparoscopic colorectal resection: a safe option for elderly patients. J Am Coll Surg. 2002; 195:768–773.
Article4. Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol. 2010; 11:637–645.
Article5. Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002; 359:2224–2229.
Article6. Clinical Outcomes of Surgical Therapy Study Group. Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350:2050–2059.
Article7. Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007; 25:3061–3068.
Article8. Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, et al. Longterm follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg. 2013; 100:75–82.
Article9. Lorenzon L, La Torre M, Ziparo V, Montebelli F, Mercantini P, Balducci G, et al. Evidence based medicine and surgical approaches for colon cancer: evidences, benefits and limitations of the laparoscopic vs open resection. World J Gastroenterol. 2014; 20:3680–3692.10. Sammour T, Jones IT, Gibbs P, Chandra R, Steel MC, Shedda SM, et al. Comparing oncological outcomes of laparoscopic versus open surgery for colon cancer: analysis of a large prospective clinical database. J Surg Oncol. 2015; 111:891–898.
Article11. Scarpa M, Erroi F, Ruffolo C, Mollica E, Polese L, Pozza G, et al. Minimally invasive surgery for colorectal cancer: quality of life, body image, cosmesis, and functional results. Surg Endosc. 2009; 23:577–582.
Article12. Choi SI, Lee KY, Park SJ, Lee SH. Single port laparoscopic right hemicolectomy with D3 dissection for advanced colon cancer. World J Gastroenterol. 2010; 16:275–278.
Article13. Hamzaoglu I, Karahasanoglu T, Baca B, Karatas A, Aytac E, Kahya AS. Single-port laparoscopic sphincter-saving mesorectal excision for rectal cancer: report of the first 4 human cases. Arch Surg. 2011; 146:75–81.14. Merchant AM, Lin E. Single-incision laparoscopic right hemicolectomy for a colon mass. Dis Colon Rectum. 2009; 52:1021–1024.
Article15. Ramos-Valadez DI, Patel CB, Ragupathi M, Bartley Pickron T, Haas EM. Single-incision laparoscopic right hemicolectomy: safety and feasibility in a series of consecutive cases. Surg Endosc. 2010; 24:2613–2616.
Article16. Poon JT, Cheung CW, Fan JK, Lo OS, Law WL. Single-incision versus conventional laparoscopic colectomy for colonic neoplasm: a randomized, controlled trial. Surg Endosc. 2012; 26:2729–2734.
Article17. Yu H, Shin JY. Short-term outcomes following reduced-port, single-port, and multi-port laparoscopic surgery for colon cancer: tailored laparoscopic approaches based on tumor size and nodal status. Int J Colorectal Dis. 2016; 31:115–122.
Article18. Bae SU, Baek SJ, Min BS, Baik SH, Kim NK, Hur H. Reduced-port laparoscopic surgery for a tumor-specific mesorectal excision in patients with colorectal cancer: initial experience with 20 consecutive cases. Ann Coloproctol. 2015; 31:16–22.
Article19. Tsutsumi S, Morita H, Fujii T, Suto T, Yajima R, Takada T, et al. Feasibility of reduced port laparoscopic colectomy for colon cancer. Hepatogastroenterology. 2015; 62:873–875.20. Nakanishi M, Kuriu Y, Murayama Y, Arita T, Ito H, Kosuga T, et al. Usefulness of reduced port surgery for left colon cancer. Anticancer Res. 2016; 36:4749–4752.
Article21. Song JM, Kim JH, Lee YS, Kim HY, Lee IK, Oh ST, et al. Reduced port laparoscopic surgery for colon cancer is safe and feasible in terms of short-term outcomes: comparative study with conventional multiport laparoscopic surgery. Ann Surg Treat Res. 2016; 91:195–201.
Article22. Huh JW, Kim CH, Kim HR, Kim YJ. Factors predicting oncologic outcomes in patients with fewer than 12 lymph nodes retrieved after curative resection for colon cancer. J Surg Oncol. 2012; 105:125–129.
Article23. Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003; 21:2912–2919.
Article24. Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol. 2003; 10:65–71.
Article25. Sarli L, Bader G, Iusco D, Salvemini C, Mauro DD, Mazzeo A, et al. Number of lymph nodes examined and prognosis of TNM stage II colorectal cancer. Eur J Cancer. 2005; 41:272–279.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reduced port laparoscopic surgery for colon cancer is safe and feasible in terms of short-term outcomes: comparative study with conventional multiport laparoscopic surgery
- Short- and long-term outcomes of laparoscopic segmental left colectomy for splenic flexure colon cancer: comparison with propensity score matching
- Clinical Outcomes of Reduced-Port Laparoscopic Surgery for Patients With Sigmoid Colon Cancer: Surgery With 1 Surgeon and 1 Camera Operator
- Current Status of Single-port Colectomy in Korea
- D2 Lymph Node Dissections during Reduced-port Robotic Distal Subtotal Gastrectomy and Conventional Laparoscopic Surgery Performed by a Single Surgeon in a High-volume Center: a Propensity Score-matched Analysis