Ann Surg Treat Res.
2018 Mar;94(3):142-146. 10.4174/astr.2018.94.3.142.
In vivo porcine training model of laparoscopic common bile duct repair with T-tube insertion under the situation of iatrogenic common bile duct injury
- Affiliations
-
- 1Department of Trauma and Surgical Critical Care, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. gshth@catholic.ac.kr
- KMID: 2405326
- DOI: http://doi.org/10.4174/astr.2018.94.3.142
Abstract
- PURPOSE
We introduce a training porcine model for laparoscopic common bile duct (CBD) repair with T-tube insertion. The model could be the feasible training tool for a surgeon learning hepatobiliary surgery.
METHODS
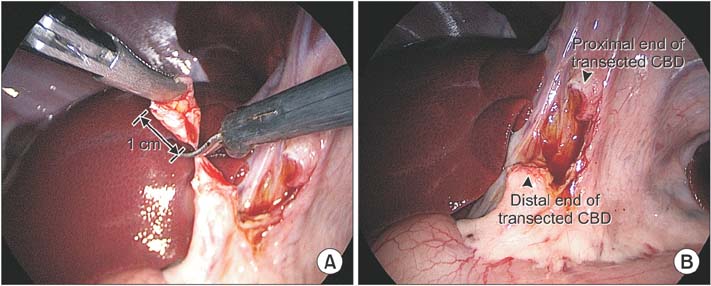
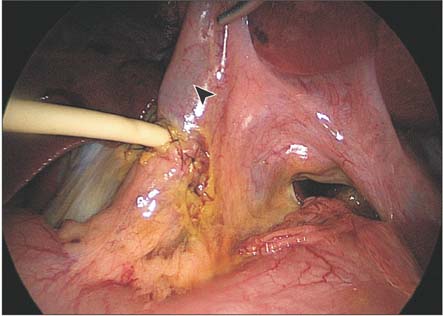
Totally laparoscopic CBD repair with T-tube insertion was performed on 9 pigs by 9 trainees naïve in hepatobiliary surgery. Similar to the situation of iatrogenic injury, CBD was transected by laparoscopic scissors at the middle part about 1 cm in length, and the transected CBD was repaired through end-to-end anastomosis with T-tube insertion. A secureness of anastomosis was confirmed by saline leakage test and all animals were sacrificed after the surgery.
RESULTS
All novice surgeons completed operations successfully without complications. Total mean operative time was 85 ± 1.7 minutes and the mean time spent performing the CBD repair with T-tube insertion was 71 ± 3 minutes. There was no bile leakage after primary anastomosis in all animals.
CONCLUSION
This porcine training model for laparoscopic CBD repair with T-tube insertion could be a feasible and effective training tool for surgeons with little experience in laparoscopic hepatobiliary surgery.
Keyword
Figure
Reference
-
1. Dagash H, Chowdhury M, Pierro A. When can I be proficient in laparoscopic surgery? A systematic review of the evidence. J Pediatr Surg. 2003; 38:720–724.
Article2. Schoffl H, Hager D, Hinterdorfer C, Dunst KM, Froschauer S, Steiner W, et al. Pulsatile perfused porcine coronary arteries for microvascular training. Ann Plast Surg. 2006; 57:213–216.
Article3. Pettigrew RA, Burns HJ, Carter DC. Evaluating surgical risk: the importance of technical factors in determining outcome. Br J Surg. 1987; 74:791–794.
Article4. Wu JS, Strasberg SM, Luttmann DR, Meininger TA, Talcott MR, Soper NJ. Laparoscopic hepatic lobectomy in the porcine model. Surg Endosc. 1998; 12:232–235.
Article5. Hua J, Lin S, Qian D, He Z, Zhang T, Song Z. Primary closure and rate of bile leak following laparoscopic common bile duct exploration via choledochotomy. Dig Surg. 2015; 32:1–8.
Article6. Cameron BH, O'Regan PJ, Anderson DL. A pig model for advanced laparoscopic biliary procedures. Surg Endosc. 1994; 8:1423–1424.
Article7. Watson DI, Treacy PJ, Williams JA. Developing a training model for laparoscopic common bile duct surgery. Surg Endosc. 1995; 9:1116–1118.
Article8. Ferrer J, Scott WE 3rd, Weegman BP, Suszynski TM, Sutherland DE, Hering BJ, et al. Pig pancreas anatomy: implications for pancreas procurement, preservation, and islet isolation. Transplantation. 2008; 86:1503–1510.
Article9. Strasberg SM, Callery MP, Soper NJ. Laparoscopic surgery of the bile ducts. Gastrointest Endosc Clin N Am. 1996; 6:81–105.
Article10. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995; 180:101–125.11. Lee JS, Hong TH. In vivo porcine training model for laparoscopic Roux-en-Y choledochojejunostomy. Ann Surg Treat Res. 2015; 88:306–310.12. Sanchez A, Otano N, Rodriguez O, Sanchez R, Benitez G, Schweitzer M. Laparoscopic common bile duct exploration four-task training model: construct validity. JSLS. 2012; 16:10–15.
Article13. Leida Z, Ping B, Shuguang W, Yu H. A randomized comparison of primary closure and T-tube drainage of the common bile duct after laparoscopic choledochotomy. Surg Endosc. 2008; 22:1595–1600.
Article14. Lee JS, Hong TH. The rat choledochojejunostomy model for microsurgical training. Ann Surg Treat Res. 2016; 90:246–249.
Article15. Palter VN, Orzech N, Aggarwal R, Okrainec A, Grantcharov TP. Resident perceptions of advanced laparoscopic skills training. Surg Endosc. 2010; 24:2830–2834.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent classifications of the common bile duct injury
- Laparoscopic cholecystectomy and common bile duct exploration for gallstone and common bile duct stone in a patient with a left-sided gallbladder: a case report
- Laparoscopic Surgery for Common Bile Duct Stone
- Primary common bile duct closure and antegrade stent insertion in choledocholithiasis patients
- A Case of Villous Adenomas in the Common Bile Duct and Cystic Duct