Cancer Res Treat.
2018 Jan;50(1):275-282. 10.4143/crt.2017.041.
No Association of Positive Superficial and/or Deep Margins with Local Recurrence in Invasive Breast Cancer Treated with Breast-Conserving Surgery
- Affiliations
-
- 1Department of Surgery, Hanyang University College of Medicine, Seoul, Korea.
- 2Division of Breast and Endocrine Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jjjongwr@hanmail.net
- 3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 5Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2403496
- DOI: http://doi.org/10.4143/crt.2017.041
Abstract
- PURPOSE
We evaluated the effect of positive superficial and/or deep margin status on local recurrence (LR) in invasive breast cancer treated with breast-conserving surgery (BCS) followed by radiotherapy.
MATERIALS AND METHODS
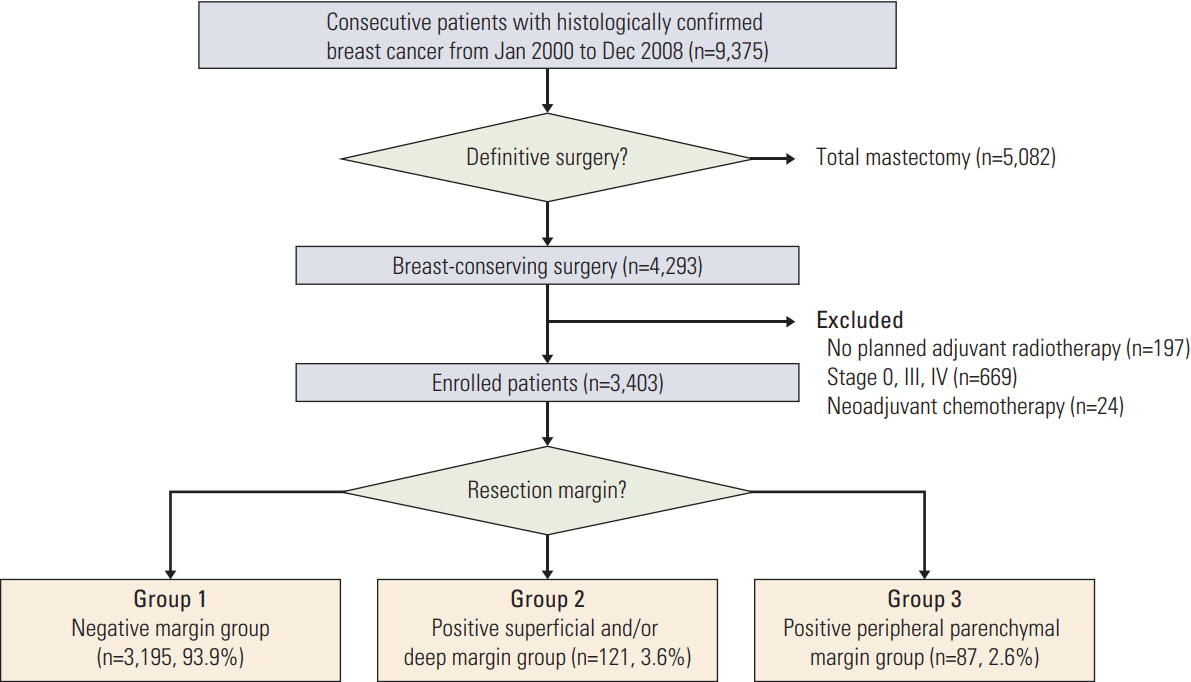
In total, 3,403 stage 1 and 2 invasive breast cancer patients treated with BCS followed by radiotherapy from January 2000 to December 2008 were included in this study. These patients were divided into three groups according to margin status: clear resection margin status for all sections (group 1, n=3,195); positive margin status in superficial and/or deep sections (group 2, n=121); and positive peripheral parenchymal margin regardless of superficial and/or deep margin involvement (group 3, n=87). The LR-free survival between these three groups was compared and the prognostic role of margin status was analyzed.
RESULTS
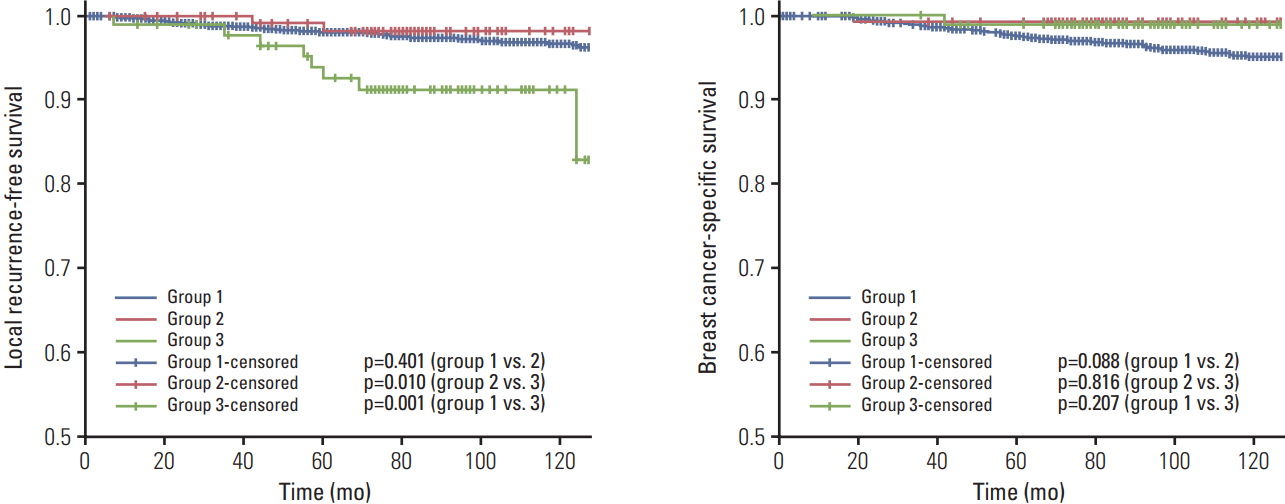
Across all groups, age, tumor size, nodal status, and human epidermal growth factor receptor 2 status did not significantly differ. High grade, positive extensive intraductal component, hormone receptor positivity, hormone therapy received, and chemotherapy not received were more prevalent in groups 2 and 3 than in group 1. Five-year LR rates in groups 1, 2, and 3 were 1.9%, 1.7%, and 7.7%, respectively. Multivariate analysis revealed that group 3 was a significant predictor for LR (hazard ratio [HR], 4.78; p < 0.001), but that positive superficial and/or deep margin was not (HR, 0.66; p=0.57).
CONCLUSION
Superficial and/or deep margin involvement following BCS is not an important predictor for LR.
MeSH Terms
Figure
Cited by 1 articles
-
Assessment of Eligibility and Utilization of Accelerated Partial Breast Irradiation in Korean Breast Cancer Patients (KROG 22-15)
Seok-Joo Chun, Ji Hwan Jo, Yong Bae Kim, Sangjoon Park, Sung-Ja Ahn, Su Ssan Kim, Kyubo Kim, Kyung Hwan Shin
Cancer Res Treat. 2024;56(2):549-556. doi: 10.4143/crt.2023.1109.
Reference
-
References
1. Forrest AP, Stewart HJ, Everington D, Prescott RJ, McArdle CS, Harnett AN, et al. Randomised controlled trial of conservation therapy for breast cancer: 6-year analysis of the Scottish trial. Scottish Cancer Trials Breast Group. Lancet. 1996; 348:708–13.2. Malmstrom P, Holmberg L, Anderson H, Mattsson J, Jonsson PE, Tennvall-Nittby L, et al. Breast conservation surgery, with and without radiotherapy, in women with lymph node-negative breast cancer: a randomised clinical trial in a population with access to public mammography screening. Eur J Cancer. 2003; 39:1690–7.3. Ko BS, Noh WC, Kang SS, Park BW, Kang EY, Paik NS, et al. Changing patterns in the clinical characteristics of korean breast cancer from 1996-2010 using an online nationwide breast cancer database. J Breast Cancer. 2012; 15:393–400.
Article4. Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans V, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005; 366:2087–106.5. Houssami N, Macaskill P, Marinovich ML, Dixon JM, Irwig L, Brennan ME, et al. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur J Cancer. 2010; 46:3219–32.
Article6. Singletary SE. Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy. Am J Surg. 2002; 184:383–93.
Article7. Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, et al. Tailoring therapies: improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015; 26:1533–46.8. NIH consensus conference. Treatment of early-stage breast cancer. JAMA. 1991; 265:391–5.9. McIntosh A, Freedman G, Eisenberg D, Anderson P. Recurrence rates and analysis of close or positive margins in patients treated without re-excision before radiation for breast cancer. Am J Clin Oncol. 2007; 30:146–51.
Article10. Fisher ER, Sass R, Fisher B, Gregorio R, Brown R, Wickerham L. Pathologic findings from the National Surgical Adjuvant Breast Project (protocol 6). II. Relation of local breast recurrence to multicentricity. Cancer. 1986; 57:1717–24.11. Veronesi U, Marubini E, Mariani L, Galimberti V, Luini A, Veronesi P, et al. Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol. 2001; 12:997–1003.
Article12. Lupe K, Truong PT, Alexander C, Lesperance M, Speers C, Tyldesley S. Subsets of women with close or positive margins after breast-conserving surgery with high local recurrence risk despite breast plus boost radiotherapy. Int J Radiat Oncol Biol Phys. 2011; 81:e561–8.
Article13. Heimann R, Powers C, Halpem HJ, Michel AG, Ewing CA, Wyman B, et al. Breast preservation in stage I and II carcinoma of the breast. The University of Chicago experience. Cancer. 1996; 78:1722–30.
Article14. Moran MS, Schnitt SJ, Giuliano AE, Harris JR, Khan SA, Horton J, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Ann Surg Oncol. 2014; 21:704–16.
Article15. Cellini C, Hollenbeck ST, Christos P, Martins D, Carson J, Kemper S, et al. Factors associated with residual breast cancer after re-excision for close or positive margins. Ann Surg Oncol. 2004; 11:915–20.
Article16. Mullen R, Macaskill EJ, Khalil A, Elseedawy E, Brown DC, Lee AC, et al. Involved anterior margins after breast conserving surgery: is re-excision required? Eur J Surg Oncol. 2012; 38:302–6.
Article17. Losken A, Dugal CS, Styblo TM, Carlson GW. A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg. 2014; 72:145–9.
Article18. De Lorenzi F, Hubner G, Rotmensz N, Bagnardi V, Loschi P, Maisonneuve P, et al. Oncological results of oncoplastic breast-conserving surgery: Long term follow-up of a large series at a single institution: A matched-cohort analysis. Eur J Surg Oncol. 2016; 42:71–7.19. Tenofsky PL, Dowell P, Topalovski T, Helmer SD. Surgical, oncologic, and cosmetic differences between oncoplastic and nononcoplastic breast conserving surgery in breast cancer patients. Am J Surg. 2014; 207:398–402.
Article20. Chakravorty A, Shrestha AK, Sanmugalingam N, Rapisarda F, Roche N, Querci Della Rovere G, et al. How safe is oncoplastic breast conservation? Comparative analysis with standard breast conserving surgery. Eur J Surg Oncol. 2012; 38:395–8.
Article21. Kaur N, Petit JY, Rietjens M, Maffini F, Luini A, Gatti G, et al. Comparative study of surgical margins in oncoplastic surgery and quadrantectomy in breast cancer. Ann Surg Oncol. 2005; 12:539–45.
Article22. de Bock GH, van der Hage JA, Putter H, Bonnema J, Bartelink H, van de Velde CJ. Isolated loco-regional recurrence of breast cancer is more common in young patients and following breast conserving therapy: long-term results of European Organisation for Research and Treatment of Cancer studies. Eur J Cancer. 2006; 42:351–6.
Article23. Koca B, Kuru B, Yuruker S, Gokgul B, Ozen N. Factors affecting surgical margin positivity in invasive ductal breast cancer patients who underwent breast-conserving surgery after preoperative core biopsy diagnosis. J Korean Surg Soc. 2013; 84:154–9.
Article24. Schnitt SJ, Connolly JL. Processing and evaluation of breast excision specimens: a clinically oriented approach. Am J Clin Pathol. 1992; 98:125–37.
Article25. Cabioglu N, Hunt KK, Sahin AA, Kuerer HM, Babiera GV, Singletary SE, et al. Role for intraoperative margin assessment in patients undergoing breast-conserving surgery. Ann Surg Oncol. 2007; 14:1458–71.
Article26. Gabos Z, Thoms J, Ghosh S, Hanson J, Deschenes J, Sabri S, et al. The association between biological subtype and locoregional recurrence in newly diagnosed breast cancer. Breast Cancer Res Treat. 2010; 124:187–94.
Article27. Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010; 363:1938–48.
Article28. Lowery AJ, Kell MR, Glynn RW, Kerin MJ, Sweeney KJ. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat. 2012; 133:831–41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Outcomes of Standard and Oncoplastic Breast-Conserving Surgery
- Oncoplastic Breast Surgery
- Clinical and Histopathological Analysis of Reoperation Cases in Breast Conserving Surgery
- Breast-Conserving Surgery With or Without Radiation Therapy for Early Breast Cancer
- Follow-Up after Volume Replacement Using Acellular Dermal Matrix in Oncoplastic Breast-Conserving Surgery