J Dent Anesth Pain Med.
2017 Dec;17(4):271-280. 10.17245/jdapm.2017.17.4.271.
A retrospective analysis of outpatient anesthesia management for dental treatment of patients with severe Alzheimer's disease
- Affiliations
-
- 1Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, Korea. stone90@snu.ac.kr
- 2Special Care Clinic, Seoul National University Dental Hospital, Seoul, Korea.
- 3Department of anesthesiology and pain medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 2399797
- DOI: http://doi.org/10.17245/jdapm.2017.17.4.271
Abstract
- BACKGROUND
The number of patients with Alzheimer's disease is growing worldwide, and the proportion of patients requiring dental treatment under general anesthesia increases with increasing severity of the disease. However, outpatient anesthesia management for these patients involves great risks, as most patients with Alzheimer's disease are old and may show reduced cardiopulmonary functions and have cognitive disorders.
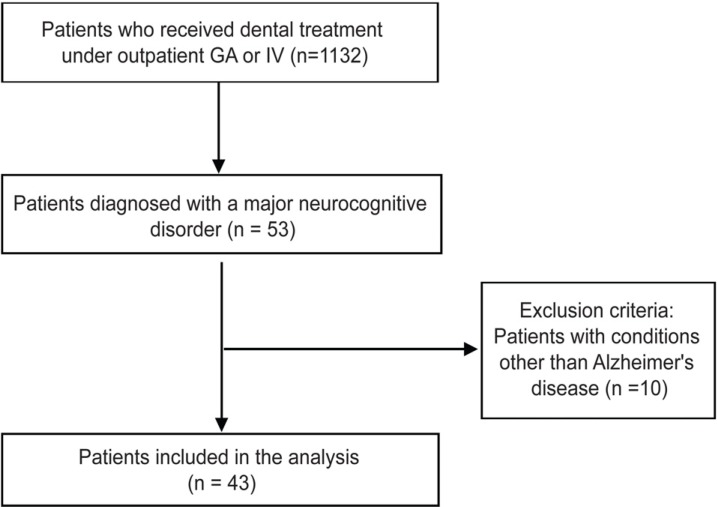
METHODS
This study retrospectively investigated 43 patients with Alzheimer's disease who received outpatient anesthesia for dental treatment between 2012-2017. Pre-anesthesia patient evaluation, dental treatment details, anesthetics dose, blood pressure, duration and procedure of anesthesia, and post-recovery management were analyzed and compared between patients who underwent general anesthesia or intravenous sedation.
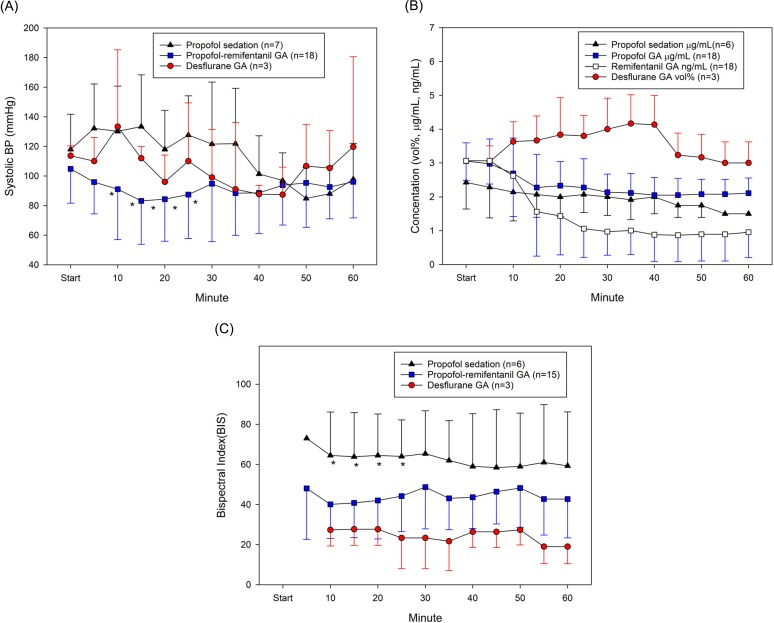
RESULTS
Mean age of patients was about 70 years; mean duration of Alzheimer's disease since diagnosis was 6.3 years. Severity was assessed using the global deterioration scale; 62.8% of patients were in level ≥ 6. Mean duration of anesthesia was 178 minutes for general anesthesia and 85 minutes for intravenous sedation. Mean recovery time was 65 minutes. Eleven patients underwent intravenous sedation using propofol, and 22/32 cases involved total intravenous anesthesia using propofol and remifentanil. Anesthesia was maintained with desflurane for other patients. While maintaining anesthesia, inotropic and atropine were used for eight and four patients, respectively. No patient developed postoperative delirium. All patients were discharged without complications.
CONCLUSION
With appropriate anesthetic management, outpatient anesthesia was successfully performed without complications for dental treatment for patients with severe Alzheimer's disease.
MeSH Terms
Figure
Cited by 1 articles
-
Effects site concentrations of propofol using target-controlled infusion in dental treatment under deep sedation among different intellectual disability types
Keyling S. Salinas Salmeron, Hyun Jeong Kim, Kwang-Suk Seo
J Dent Anesth Pain Med. 2019;19(4):217-226. doi: 10.17245/jdapm.2019.19.4.217.
Reference
-
1. Hugo J, Ganguli M. Dementia and cognitive impairment: Epidemiology, diagnosis, and treatment. Clin Geriatr Med. 2014; 30:421–442. PMID: 25037289.2. Alzheimer's Association. 2017 Alzheimer's disease facts and figures. Alzheimers Dement. 2017; 13:325–373.3. Ellefsen B, Holm-Pedersen P, Morse DE, Schroll M, Andersen BB, Waldemar G. Assessing caries increments in elderly patients with and without dementia: A one-year follow-up study. J Am Dent Assoc. 2009; 140:1392–1400. PMID: 19884398.4. Chen X, Clark JJ, Naorungroj S. Oral health in nursing home residents with different cognitive statuses. Gerodontology. 2013; 30:49–60. PMID: 22364512.
Article5. Kieser J, Jones G, Borlase G, MacFadyen E. Dental treatment of patients with neurodegenerative disease. N Z Dent J. 1999; 95:130–134. PMID: 10687380.6. Kocaelli H, Yaltirik M, Yargic LI, Özbas H. Alzheimer's disease and dental management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:521–524. PMID: 12075198.
Article7. Lim MA, Borromeo GL. The use of general anesthesia to facilitate dental treatment in adult patients with special needs. J Dent Anesth Pain Med. 2017; 17:91–103. PMID: 28879336.
Article8. Caputo AC. Providing deep sedation and general anesthesia for patients with special needs in the dental office-based setting. Spec Care Dentist. 2009; 29:26–30. PMID: 19152565.
Article9. Rosenthal RA, Kavic SM. Assessment and management of the geriatric patient. Crit Care Med. 2004; 32(4 Suppl):S92–S105. PMID: 15064668.
Article10. Kim MS, Seo KS, Kim HJ, Han HJ, Shin TJ, Chang J. Dental treatment of a patient with alzheimer disease under ambulatory general anesthesia. J Korean Dent Soc Anesthesiol. 2011; 11:146–152.
Article11. Reisberg B, Ferris SH, de Leon MJ, Crook T. The global deterioration scale for assessment of primary degenerative dementia. American journal of psychiatry. Am J Psychiatry. 1982; 139:1136–1139. PMID: 7114305.12. Seo KS, Shin TJ, Kim HJ, Han HJ, Han JH, Kim HJ, et al. Clinico-statistical analysis of cooperation and anesthetic induction method of dental patients with special needs. J Korean Dent Soc Anesthesiol. 2009; 9:9–16.
Article13. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: A systematic review and metaanalysis. Alzheimers Dement. 2013; 9:63–75.e2. PMID: 23305823.
Article14. Kim YJ, Han JW, So YS, Seo JY, Kim KY, Kim KW. Prevalence and trends of dementia in korea: A systematic review and meta-analysis. J Korean Med Sci. 2014; 29:903–912. PMID: 25045221.
Article15. Rocchi A, Pellegrini S, Siciliano G, Murri L. Causative and susceptibility genes for alzheimer's disease: A review. Brain Res Bull. 2003; 61:1–24. PMID: 12788204.
Article16. Selkoe DJ. Alzheimer's disease: Genes, proteins, and therapy. Physiol Rev. 2001; 81:741–766. PMID: 11274343.
Article17. Warren JJ, Chalmers JM, Levy SM, Blanco VL, Ettinger RL. Oral health of persons with and without dementia attending a geriatric clinic. Spec Care Dentist. 1997; 17:47–53. PMID: 9582699.
Article18. Turner LN, Balasubramaniam R, Hersh EV, Stoopler ET. Drug therapy in alzheimer disease: An update for the oral health care provider. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:467–476. PMID: 18928896.
Article19. Mancini M, Grappasonni I, Scuri S, Amenta F. Oral health in alzheimer's disease: A review. Curr Alzheimer Res. 2010; 7:368–373. PMID: 20043813.
Article20. Zuo C, Zuo Z. Spine surgery under general anesthesia may not increase the risk of alzheimer's disease. Dement Geriatr Cogn Disord. 2010; 29:233–239. PMID: 20375503.
Article21. Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH, et al. Prevalence of prehypertension and hypertension in a korean population: Korean national health and nutrition survey 2001. J Hypertens. 2006; 24:1515–1521. PMID: 16877953.
Article22. Qaseem A, Snow V, Fitterman N, Hornbake ER, Lawrence VA, Smetana GW, et al. Risk assessment for and strategies to reduce perioperative pulmonary complications for patients undergoing noncardiothoracic surgery: A guideline from the american college of physicians. Ann Intern Med. 2006; 144:575–580. PMID: 16618955.
Article23. Kalia M. Dysphagia and aspiration pneumonia in patients with alzheimer's disease. Metabolism. 2003; 52(10 Suppl 2):36–38. PMID: 14577062.
Article24. Allan LM, Ballard CG, Allen J, Murray A, Davidson AW, McKeith IG, et al. Autonomic dysfunction in dementia. J Neurol Neurosurg Psychiatry. 2007; 78:671–677. PMID: 17178816.
Article25. Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology. 1997; 86:24–33. PMID: 9009936.26. Bianchi SL, Caltagarone BM, Laferla FM, Eckenhoff RG, Kelz MB. Inhaled anesthetic potency in aged alzheimer mice. Anesth Analg. 2010; 110:427–430. PMID: 19820240.
Article27. Culley DJ, Baxter MG, Yukhananov R, Crosby G. Long-term impairment of acquisition of a spatial memory task following isoflurane-nitrous oxide anesthesia in rats. Anesthesiology. 2004; 100:309–314. PMID: 14739805.
Article28. Aranake A, Mashour GA, Avidan MS. Minimum alveolar concentration: Ongoing relevance and clinical utility. Anaesthesia. 2013; 68:512–522. PMID: 23414556.
Article29. Nickalls RW, Mapleson WW. Age-related iso-mac charts for isoflurane, sevoflurane and desflurane in man. Br J Anaesth. 2003; 91:170–174. PMID: 12878613.30. Schultz A, Grouven U, Zander I, Beger FA, Siedenberg M, Schultz B. Age-related effects in the EEG during propofol anaesthesia. Acta Anaesthesiol Scand. 2004; 48:27–34. PMID: 14674970.
Article31. Papon MA, Whittington RA, El-Khoury NB, Planel E. Alzheimer's disease and anesthesia. Front Neurosci. 2011; 4:272. PMID: 21344011.
Article32. Rudolph JL, Marcantonio ER. Review articles: Postoperative delirium: Acute change with long-term implications. Anesth Analg. 2011; 112:1202–1211. PMID: 21474660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outpatient General Anesthesia for Mentally and Physically Handicapped Children Undergoing Extensive Dental Treatment
- The Analysis of Outpatient Anesthesia for Dental Treatment in Handicapped Patients with Behavior Disorder
- Treatment of severe pain in a patient with complex regional pain syndrome undergoing dental treatment under general anesthesia: A case report
- A Survey of the Sedation or Outpatient General Anesthesia in Department of Pediatric Dentistry, Chonnam National University Dental Hospital and Gwangju Dental Clinic for the Disabled
- A Survey of the Outpatient General Anesthesia and Dental Treatment in Chungnam Dental Clinic for the Disabled