Ann Surg Treat Res.
2017 Sep;93(3):119-124. 10.4174/astr.2017.93.3.119.
Comparison of morbidity-related seroma formation following conventional latissimus dorsi flap versus muscle-sparing latissimus dorsi flap breast reconstruction
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Kyoto Prefectural University of Medicine, Graduate School of Medical Sciences, Kyoto, Japan. sowawan@kpu-m.ac.jp
- 2Department of Endocrine and Breast Surgery, Kyoto Prefectural University of Medicine, Graduate School of Medical Sciences, Kyoto, Japan.
- KMID: 2398957
- DOI: http://doi.org/10.4174/astr.2017.93.3.119
Abstract
- PURPOSE
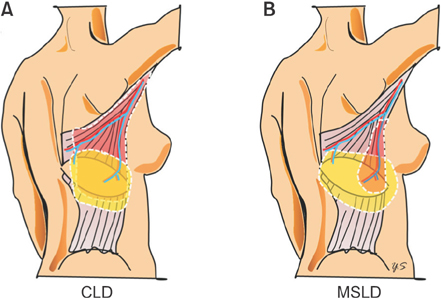
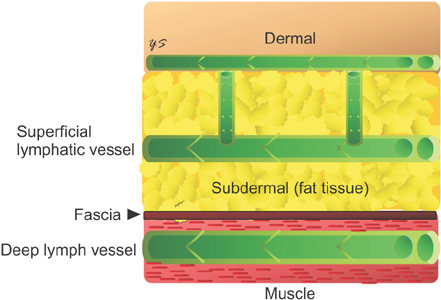
The pedicled, descending-branch muscle-sparing latissimus dorsi (MSLD) flap has been widely used for breast reconstruction following total mastectomy. However, the superiority of the MSLD flap compared to the conventional latissimus dorsi (CLD) flap in preventing seroma formation has not been demonstrated. This study compares the morbidities related to seroma formation following pedicled MSLD flap and CLD flap breast reconstruction.
METHODS
A total of 15 women who underwent partial mastectomy and immediate partial breast reconstruction with MSLD flaps were compared with 15 women under identical conditions with CLD flap breast reconstruction. The medical records were reviewed for both complications and demographic data. The authors compared morbidity, including donor-site seroma, total volume of drain discharge, indwelling period of drainage, and length of hospital stay following both MSLD flap and CLD flap breast reconstruction.
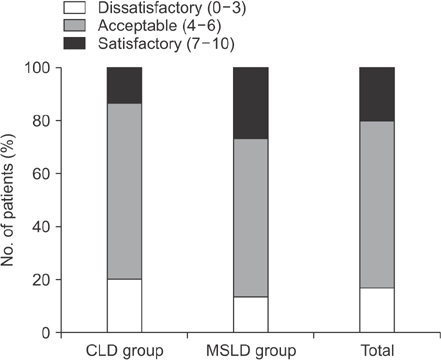
RESULTS
The demographic data of the 2 groups were not significantly different. Donor-site seroma occurred in 2 MSLD patients (13.3%) and in 6 CLD patients (40.0%). The total volume of the drain discharge and the indwelling period of drainage at donor site were significantly lower in the MSLD group. The length of hospital stay was significantly shorter (by approximately a day and a half) for the MSLD group.
CONCLUSION
The MSLD flap, with its low complication rate and associated minimal functional and aesthetic deficits at the donor site, may be a useful option for small breast reconstruction if earlier discharge from hospital is demanded.
Keyword
MeSH Terms
Figure
Reference
-
1. Clough KB, Louis-Sylvestre C, Fitoussi A, Couturaud B, Nos C. Donor site sequelae after autologous breast reconstruction with an extended latissimus dorsi flap. Plast Reconstr Surg. 2002; 109:1904–1911.2. Roy MK, Shrotia S, Holcombe C, Webster DJ, Hughes LE, Mansel RE. Complications of latissimus dorsi myocutaneous flap breast reconstruction. Eur J Surg Oncol. 1998; 24:162–165.3. Schwabegger A, Ninkovic M, Brenner E, Anderl H. Seroma as a common donor site morbidity after harvesting the latissimus dorsi flap: observations on cause and prevention. Ann Plast Surg. 1997; 38:594–597.4. Saint-Cyr M, Nagarkar P, Schaverien M, Dauwe P, Wong C, Rohrich RJ. The pedicled descending branch muscle-sparing latissimus dorsi flap for breast reconstruction. Plast Reconstr Surg. 2009; 123:13–24.5. Brackley PT, Mishra A, Sigaroudina M, Iqbal A. Modified muscle sparing latissimus dorsi with implant for total breast reconstruction - extending the boundaries. J Plast Reconstr Aesthet Surg. 2010; 63:1495–1502.6. Colohan S, Wong C, Lakhiani C, Cheng A, Maia M, Arbique G, et al. The free descending branch muscle-sparing latissimus dorsi flap: vascular anatomy and clinical applications. Plast Reconstr Surg. 2012; 130:776e–787e.7. Zhu L, Mohan AT, Saint-Cyr M. A simple approach to harvest of the pedicled descending branch muscle-sparing latissimus dorsi flap. J Plast Reconstr Aesthet Surg. 2015; 68:e179–e181.8. Kim H, Wiraatmadja ES, Lim SY, Pyon JK, Bang SI, Oh KS, et al. Comparison of morbidity of donor site following pedicled muscle-sparing latissimus dorsi flap versus extended latissimus dorsi flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2013; 66:640–646.9. Tremp M, di Summa PG, Schaakxs D, Oranges CM, Wettstein R, Kalbermatten DF. Nipple reconstruction after autologous or expander breast reconstruction: a multimodal and 3-dimensional analysis. Aesthet Surg J. 2017; 37:179–187.10. Tobin GR, Moberg AW, DuBou RH, Weiner LJ, Bland KI. The split latissimus dorsi myocutaneous flap. Ann Plast Surg. 1981; 7:272–280.11. Hamdi M, Van Landuyt K, Hijjawi JB, Roche N, Blondeel P, Monstrey S. Surgical technique in pedicled thoracodorsal artery perforator flaps: a clinical experience with 99 patients. Plast Reconstr Surg. 2008; 121:1632–1641.12. Santanelli F, Longo B, Germano S, Rubino C, Laporta R, Hamdi M. Total breast reconstruction using the thoracodorsal artery perforator flap without implant. Plast Reconstr Surg. 2014; 133:251–254.13. Woodworth PA, McBoyle MF, Helmer SD, Beamer RL. Seroma formation after breast cancer surgery: incidence and predicting factors. Am Surg. 2000; 66:444–450.14. McCaul JA, Aslaam A, Spooner RJ, Louden I, Cavanagh T, Purushotham AD. Aetiology of seroma formation in patients undergoing surgery for breast cancer. Breast. 2000; 9:144–148.15. Di Monta G, Caraco C, Crispo A, Marone U, Mozzillo N. Collagen sealant patch to reduce lymphatic drainage after lymph node dissection. World J Surg Oncol. 2012; 10:275.16. Suami H, Taylor GI, Pan WR. The lymphatic territories of the upper limb: anatomical study and clinical implications. Plast Reconstr Surg. 2007; 119:1813–1822.17. Campisi C, Bellini C, Campisi C, Accogli S, Bonioli E, Boccardo F. Microsurgery for lymphedema: clinical research and long-term results. Microsurgery. 2010; 30:256–260.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast reconstruction using extended latissimus dorsi muscle flap
- Axillary Reconstruction Using a Pedicled Thoracodorsal Artery Perforator Flap Including Latissimus Dorsi Muscle Strip
- Breast Reconstruction with the Extended Latissimus Dorsi Musculocutancous Flap
- Efficacy of Quilting Sutures and Fibrin Sealant Together for Prevention of Seroma in Extended Latissimus Dorsi Flap Donor Sites
- A Combined Scapular Flap and Latissimus Dorsi Flap