J Breast Cancer.
2017 Dec;20(4):327-332. 10.4048/jbc.2017.20.4.327.
Selective Radiation Therapy for Ductal Carcinoma In Situ Following Breast-Conserving Surgery According to Age and Margin Width: Korean Radiation Oncology Group 11-04 and 16-02 Studies
- Affiliations
-
- 1Department of Radiation Oncology, Ewha Womans University College of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 3Department of Radiation Oncology, Yonsei Cancer Center, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. radiat@snu.ac.kr
- 5Proton Therapy Center, National Cancer Center, Goyang, Korea.
- 6Center for Breast Cancer, National Cancer Center, Goyang, Korea.
- 7Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 8Department of Radiation Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 9Department of Radiation Oncology, Yeungnam University College of Medicine, Daegu, Korea.
- 10Department of Radiation Oncology, Kyungpook National University School of Medicine, Daegu, Korea.
- 11Department of Radiation Oncology, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2398201
- DOI: http://doi.org/10.4048/jbc.2017.20.4.327
Abstract
- PURPOSE
The optimal indications for omitting adjuvant radiation therapy (RT) after breast-conserving surgery are still controversial in ductal carcinoma in situ (DCIS) of the breast. The purpose of this study was to validate the role of postoperative RT in DCIS patients aged ≤50 years and with tumor margin widths of <1 cm, both of which have been proven to be high-risk features for recurrence in cohorts not receiving RT.
METHODS
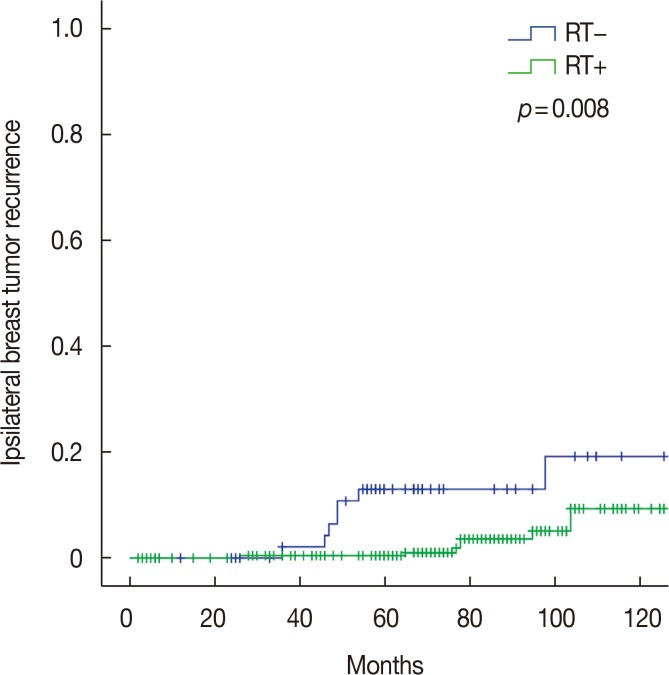
Using two multicenter retrospective studies on DCIS, a pooled analysis was performed among patients aged ≤50 years and with margin widths < 1 cm. All patients underwent breast-conserving surgery. Two hundred thirty-two patients received postoperative RT, while 54 did not. The median follow-up period was 77 months (range, 2-190 months) and 70 months (range, 5-166 months) in the patients who received RT and those who did not, respectively.
RESULTS
The patients who received RT had larger tumors (p < 0.001), higher nuclear grade (p < 0.001), closer margin width (p < 0.001), and negative estrogen receptor expression (p=0.010) compared with those who did not receive RT. During the follow-up period, there were 17 ipsilateral breast tumor recurrences (IBTRs) as follows: invasive carcinoma in 10 patients and DCIS in seven. In the univariate analysis, the treatment with RT and human epidermal growth factor receptor 2 (HER2) status were significant risk factors for IBTR. The 7-year IBTR rates with and without postoperative RT were 3.6% and 13.1%, respectively (p=0.008). HER2-positive tumors had a higher IBTR rate than the HER2-negative tumors (7-year rate, 13.6% vs. 3.9%; p=0.003).
CONCLUSION
Postoperative RT following breast-conserving surgery significantly reduced the 7-year IBTR rate in the DCIS patients aged ≤50 years and with margin widths < 1 cm. HER2 positivity was associated with increased IBTR in these patients.
MeSH Terms
-
Age Factors
Breast
Breast Neoplasms
Carcinoma, Ductal*
Carcinoma, Intraductal, Noninfiltrating*
Cohort Studies
Estrogens
Follow-Up Studies
Humans
Mastectomy, Segmental*
Radiation Oncology*
Radiotherapy
Receptor, Epidermal Growth Factor
Recurrence
Retrospective Studies
Risk Factors
Estrogens
Receptor, Epidermal Growth Factor
Figure
Reference
-
1. Wärnberg F, Garmo H, Emdin S, Hedberg V, Adwall L, Sandelin K, et al. Effect of radiotherapy after breast-conserving surgery for ductal carcinoma in situ: 20 years follow-up in the randomized SweDCIS Trial. J Clin Oncol. 2014; 32:3613–3618. PMID: 25311220.
Article2. Donker M, Litière S, Werutsky G, Julien JP, Fentiman IS, Agresti R, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma in situ: 15-year recurrence rates and outcome after a recurrence, from the EORTC 10853 randomized phase III trial. J Clin Oncol. 2013; 31:4054–4059. PMID: 24043739.
Article3. Cuzick J, Sestak I, Pinder SE, Ellis IO, Forsyth S, Bundred NJ, et al. Effect of tamoxifen and radiotherapy in women with locally excised ductal carcinoma in situ: long-term results from the UK/ANZ DCIS trial. Lancet Oncol. 2011; 12:21–29. PMID: 21145284.
Article4. Fisher B, Dignam J, Wolmark N, Mamounas E, Costantino J, Poller W, et al. Lumpectomy and radiation therapy for the treatment of intraductal breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-17. J Clin Oncol. 1998; 16:441–452. PMID: 9469327.
Article5. Rakovitch E, Nofech-Mozes S, Narod SA, Hanna W, Thiruchelvam D, Saskin R, et al. Can we select individuals with low risk ductal carcinoma in situ (DCIS)? A population-based outcomes analysis. Breast Cancer Res Treat. 2013; 138:581–590. PMID: 23456231.
Article6. Van Zee KJ, Subhedar P, Olcese C, Patil S, Morrow M. Relationship between margin width and recurrence of ductal carcinoma in situ: analysis of 2996 women treated with breast-conserving surgery for 30 years. Ann Surg. 2015; 262:623–631. PMID: 26366541.7. Solin LJ, Gray R, Hughes LL, Wood WC, Lowen MA, Badve SS, et al. Surgical excision without radiation for ductal carcinoma in situ of the breast: 12-year results from the ECOG-ACRIN E5194 Study. J Clin Oncol. 2015; 33:3938–3944. PMID: 26371148.
Article8. Wong JS, Chen YH, Gadd MA, Gelman R, Lester SC, Schnitt SJ, et al. Eight-year update of a prospective study of wide excision alone for small low- or intermediate-grade ductal carcinoma in situ (DCIS). Breast Cancer Res Treat. 2014; 143:343–350. PMID: 24346130.
Article9. McCormick B, Winter K, Hudis C, Kuerer HM, Rakovitch E, Smith BL, et al. RTOG 9804: a prospective randomized trial for good-risk ductal carcinoma in situ comparing radiotherapy with observation. J Clin Oncol. 2015; 33:709–715. PMID: 25605856.
Article10. Min SY, Kim Z, Hur MH, Yoon CS, Park EH, Jung KW, et al. The basic facts of Korean breast cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2016; 19:1–7. PMID: 27066090.
Article11. Kang JK, Kim MS, Jang WI, Seo YS, Kim HJ, Cho CK, et al. The clinical utilization of radiation therapy in Korea between 2009 and 2013. Radiat Oncol J. 2016; 34:88–95. PMID: 27381419.
Article12. Kim K, Jung SY, Shin KH, Kim JH, Han W, Lee HB, et al. Recurrence outcomes after omission of postoperative radiotherapy following breast-conserving surgery for ductal carcinoma in situ of the breast: a multicenter, retrospective study in Korea (KROG 16-02). Breast Cancer Res Treat. 2017; 162:77–83. PMID: 28083820.
Article13. Kim JH, Choi DH, Park W, Ahn SD, Kim SS, Ha SW, et al. Influence of boost radiotherapy in patients with ductal carcinoma in situ breast cancer: a multicenter, retrospective study in Korea (KROG 11-04). Breast Cancer Res Treat. 2014; 146:341–345. PMID: 24939061.
Article14. Morrow M, Van Zee KJ, Solin LJ, Houssami N, Chavez-MacGregor M, Harris JR, et al. Society of Surgical Oncology-American Society for Radiation Oncology-American Society of Clinical Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. J Clin Oncol. 2016; 34:4040–4046. PMID: 27528719.
Article15. Tadros AB, Smith BD, Shen Y, Lin H, Krishnamurthy S, Lucci A, et al. Ductal carcinoma in situ and margins <2 mm: contemporary outcomes with breast conservation. Ann Surg. 2017; 7. 24. Epub. DOI: 10.1097/SLA.0000000000002439.16. Haffty BG. Molecular and genetic markers in the local-regional management of breast cancer. Semin Radiat Oncol. 2002; 12:329–340. PMID: 12382191.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment outcome of ductal carcinoma in situ patients treated with postoperative radiation therapy
- Preliminary Results of Postoperative Radiotherapy after Breast Conserving Surgery in Early Breast Cancer
- Treatment Outcome and Analysis of the Prognostic Factors of Ductal Carcinoma in situ Treated with Breast Conserving Surgery and Radiotherapy
- Radiotherapy for Breast Cancer
- Patterns of Practice in Radiotherapy for Breast Cancer in Korea