Imaging Sci Dent.
2017 Dec;47(4):261-267. 10.5624/isd.2017.47.4.261.
Frequency of different maxillary sinus septal patterns found on cone-beam computed tomography and predicting the associated risk of sinus membrane perforation during sinus lifting
- Affiliations
-
- 1Department of Maxillofacial Surgery, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
- 2Dental Sciences Research Center, Department of Maxillofacial Radiology, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran. zahradalili@yahoo.com
- 3Private Dental Office, Guilan University of Medical Sciences, Rasht, Iran.
- 4Dental Sciences Research Center, Department of Prosthodontics, School of Dentistry, Guilan University of Medical Sciences, Rasht, Iran.
- KMID: 2397841
- DOI: http://doi.org/10.5624/isd.2017.47.4.261
Abstract
- PURPOSE
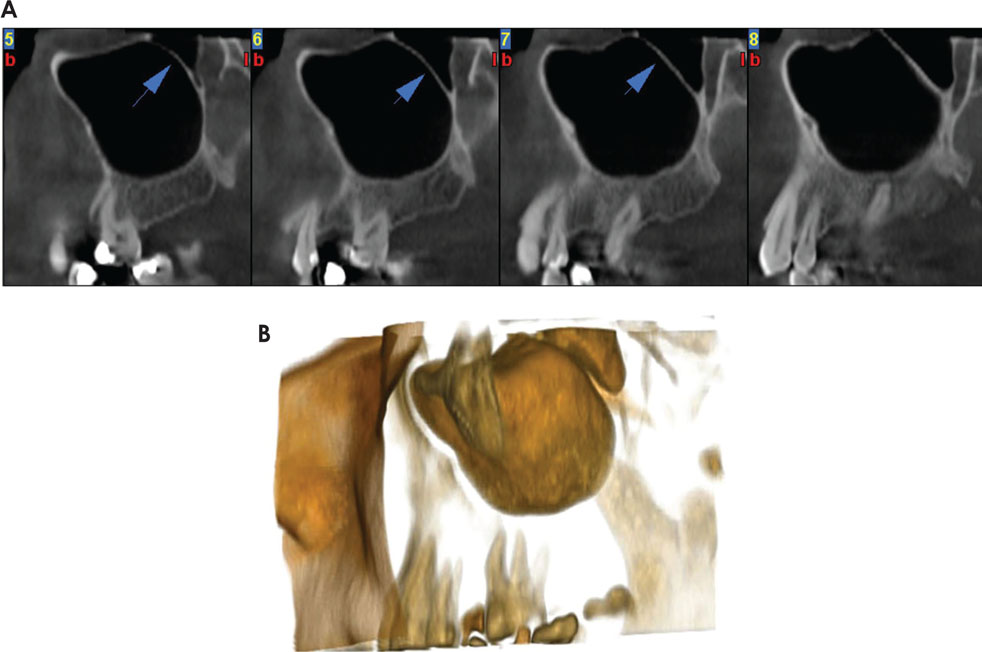
Analyzing different patterns of maxillary sinus septa in cone-beam computed tomography (CBCT) images and predicting maxillary sinus membrane perforations.
MATERIALS AND METHODS
In this cross-sectional study, CBCT images of 222 patients ranging from 20 to 81 years old were evaluated. One hundred fifty-two patients (93 females and 59 males) who had maxillary sinus septa in axial views were included in this study. Cross-sectional images were used to determine classifications of sinus septa and the risk of membrane perforation using a method modified from Al-Faraje et al. Variables of sex, age, and dental status were considered. Chi-squared and Kruskal-Wallis tests were used for data analysis (P < .05).
RESULTS
In this study, 265 maxillary sinus septal patterns were found. The mean age of the patients was 44.1±14.7 years old. The Class I and VII-div II patterns had the greatest and least prevalence, respectively. Furthermore, there was a significant relationship between the location of septa and the frequency of membrane perforation risk (P < .05). In this study, the relationship of different patterns of septa with dental status did not differ significantly (P>0.05).
CONCLUSION
A higher prevalence of moderate risk of membrane perforation in the molar region relative to the premolar region was observed. Furthermore, maxillary sinus septa occur most frequently in the molar region, demonstrating the importance of paying attention to this region during sinus lift surgery. This study did not show any relationship between tooth loss and the presence of septa.
MeSH Terms
Figure
Cited by 1 articles
-
Osseous metaplasia showing heterotopic ossification in the maxillary sinus
Sang-Hoon Kang, Jung Hyun Chang
Imaging Sci Dent. 2018;48(2):127-129. doi: 10.5624/isd.2018.48.2.127.
Reference
-
1. Al-Faraje L. Surgical complications in oral implantology: etiology, prevention, and management. Hanover Park: Quintessence;2011. p. 153–160.2. Lee WJ, Lee SJ, Kim HS. Analysis of location and prevalence of maxillary sinus septa. J Periodontal Implant Sci. 2010; 40:56–60.
Article3. Nkenke E, Stelzle F. Clinical outcomes of sinus floor augmentation for implant placement using autogenous bone or bone substitutes: a systematic review. Clin Oral Implants Res. 2009; 20:Suppl 4. 124–133.
Article4. van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000; 11:256–265.
Article5. Krennmair G, Ulm CW, Lugmayr H, Solar P. The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg. 1999; 57:667–672.
Article6. Underwood AS. An inquiry into the anatomy and pathology of the maxillary sinus. J Anat Physiol. 1910; 44:354–369.7. Maestre-Ferrín L, Galán-Gil S, Rubio-Serrano M, Peñarrocha-Diago M, Peñarrocha-Oltra D. Maxillary sinus septa: a systematic review. Med Oral Patol Oral Cir Bucal. 2010; 15:e383–e386.8. Wen SC, Chan HL, Wang HL. Classification and management of antral septa for maxillary sinus augmentation. Int J Periodontics Restorative Dent. 2013; 33:509–517.
Article9. Rancitelli D, Borgonovo AE, Cicciù M, Re D, Rizza F, Frigo AC, et al. Maxillary sinus septa and anatomic correlation with the Schneiderian membrane. J Craniofac Surg. 2015; 26:1394–1398.
Article10. van Zyl AW, van Heerden WF. A retrospective analysis of maxillary sinus septa on reformatted computerised tomography scans. Clin Oral Implants Res. 2009; 20:1398–1401.
Article11. Malec M, Smektala T, Tutak M, Trybek G, Sporniak-Tutak K. Maxillary sinus septa prevalence and morphology-computed tomography based analysis. Int J Morphol. 2015; 33:144–148.12. Park YB, Jeon HS, Shim JS, Lee KW, Moon HS. Analysis of the anatomy of the maxillary sinus septum using 3-dimensional computed tomography. J Oral Maxillofac Surg. 2011; 69:1070–1078.
Article13. Kim MJ, Jung UW, Kim CS, Kim KD, Choi SH, Kim CK, et al. Maxillary sinus septa: prevalence, height, location, and morphology. A reformatted computed tomography scan analysis. J Periodontol. 2006; 77:903–908.
Article14. Malkinson S, Irinakis T. The influence of interfering septa on the incidence of Schneiderian membrane perforations during maxillary sinus elevation surgery: a retrospective study of 52 consecutive lateral window procedures. Oral Surg. 2009; 2:19–25.
Article15. Velásquez-Plata D, Hovey LR, Peach CC, Alder ME. Maxillary sinus septa: a 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants. 2002; 17:854–860.16. Gosau M, Rink D, Driemel O, Draenert FG. Maxillary sinus anatomy: a cadaveric study with clinical implications. Anat Rec (Hoboken). 2009; 292:352–354.
Article17. Ella B, Noble Rda C, Lauverjat Y, Sédarat C, Zwetyenga N, Siberchicot F, et al. Septa within the sinus: effect on elevation of the sinus floor. Br J Oral Maxillofac Surg. 2008; 46:464–467.
Article18. Rosano G, Taschieri S, Gaudy JF, Lesmes D, Del Fabbro M. Maxillary sinus septa: a cadaveric study. J Oral Maxillofac Surg. 2010; 68:1360–1364.
Article19. Naitoh M, Suenaga Y, Kondo S, Gotoh K, Ariji E. Assessment of maxillary sinus septa using cone-beam computed tomography: etiological consideration. Clin Implant Dent Relat Res. 2009; 11:Suppl 1. e52–e58.
Article20. Shen EC, Fu E, Chiu TJ, Chang V, Chiang CY, Tu HP. Prevalence and location of maxillary sinus septa in the Taiwanese population and relationship to the absence of molars. Clin Oral Implants Res. 2012; 23:741–745.
Article21. Neugebauer J, Ritter L, Mischkowski RA, Dreiseidler T, Scherer P, Ketterle M, et al. Evaluation of maxillary sinus anatomy by cone-beam CT prior to sinus floor elevation. Int J Oral Maxillofac Implants. 2010; 25:258–265.22. Koymen R, Gocmen-Mas N, Karacayli U, Ortakoglu K, Ozen T, Yazici AC. Anatomic evaluation of maxillary sinus septa: surgery and radiology. Clin Anat. 2009; 22:563–570.
Article23. Pommer B, Ulm C, Lorenzoni M, Palmer R, Watzek G, Zechner W. Prevalence, location and morphology of maxillary sinus septa: systematic review and meta-analysis. J Clin Periodontol. 2012; 39:769–773.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of panoramic radiography and cone beam computed tomography for assessing the relationship between the maxillary sinus floor and maxillary molars
- Maxillary sinus pneumatization after maxillary molar extraction assessed with cone beam computed tomography
- Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography
- Positional relationship between the maxillary sinus floor and the apex of the maxillary first molar using cone beam computed tomograph
- Comparison of panoramic radiography and cone-beam computed tomography for assessing radiographic signs indicating root protrusion into the maxillary sinus