Korean J Sports Med.
2017 Dec;35(3):198-201. 10.5763/kjsm.2017.35.3.198.
Sequential Proximal Adjacent Spondylolysis by Pars Interarticularis Fracture in Elite Soccer Player
- Affiliations
-
- 1Spine Center, Himchan Hospital, Incheon, Korea. deux8888@kangwon.ac.kr
- 2Department of Neurosurgery, Kangwon National University College of Medicine, Chuncheon, Korea.
- 3Joint and Arthritis Research, Department of Orthopedic Surgery, Himchan Hospital, Seoul, Korea.
- KMID: 2397815
- DOI: http://doi.org/10.5763/kjsm.2017.35.3.198
Abstract
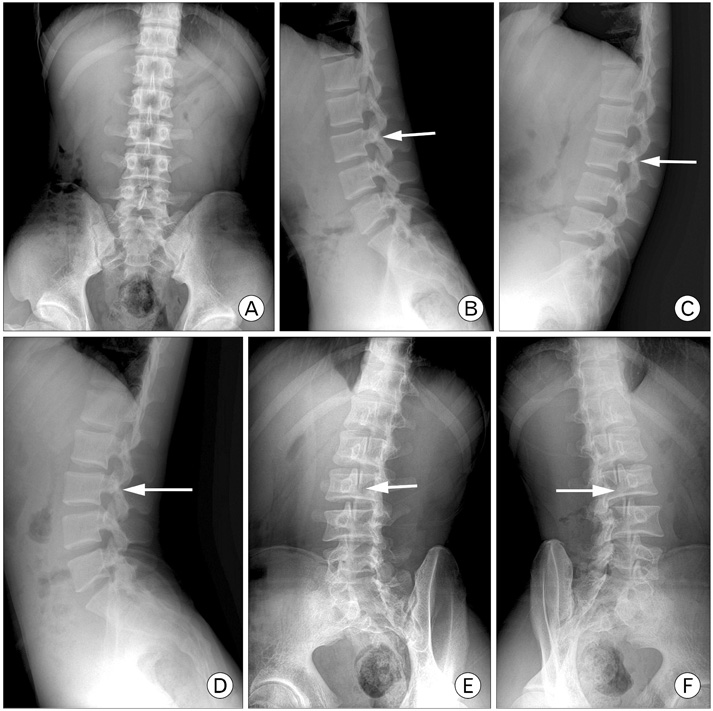
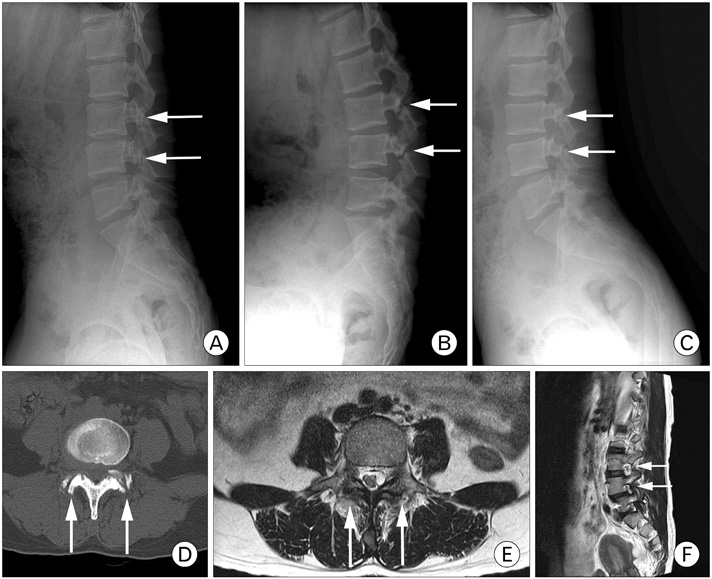
- Pars interarticularis fracture is a common finding in young soccer players with low back pain. Spondylolysis in young adults involves a defect of the pars interarticularis, occurring as a result of repeated hyperextension and rotation. Here, we describe the case of a 26-year-old male elite soccer player who was diagnosed with L3 spondylolysis 2 years previously. He visited Incheon Himchan Hospital again because of low back pain. Radiographs showed consecutive spondylolysis at the L3 and L4 levels. Physicians should be aware that repeated performance of athletic movements, such as those during soccer, might lead to consecutive levels of spondylolysis.
Keyword
MeSH Terms
Figure
Reference
-
1. Alton TB, Patel AM, Lee MJ, Chapman JR. Pediatric cervical spondylolysis and American football. Spine J. 2014; 14:e1–e5.2. Sairyo K, Katoh S, Takata Y, et al. MRI signal changes of the pedicle as an indicator for early diagnosis of spondylolysis in children and adolescents: a clinical and biomechanical study. Spine (Phila Pa 1976). 2006; 31:206–211.3. Standaert CJ. Spondylolysis in the adolescent athlete. Clin J Sport Med. 2002; 12:119–122.4. Logroscino G, Mazza O, Aulisa G, Pitta L, Pola E, Aulisa L. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst. 2001; 17:644–655.5. Masci L, Pike J, Malara F, Phillips B, Bennell K, Brukner P. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006; 40:940–946.6. Micheli LJ, Wood R. Back pain in young athletes: significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995; 149:15–18.7. Donaldson LD. Spondylolysis in elite junior-level ice hockey players. Sports Health. 2014; 6:356–359.8. McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Curr Sports Med Rep. 2007; 6:62–66.9. Sakai T, Sairyo K, Takao S, Nishitani H, Yasui N. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine (Phila Pa 1976). 2009; 34:2346–2350.10. Sairyo K, Katoh S, Sasa T, et al. Athletes with unilateral spondylolysis are at risk of stress fracture at the contralateral pedicle and pars interarticularis: a clinical and biomechanical study. Am J Sports Med. 2005; 33:583–590.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- MR Imaging of Lumbar Spondylolysis: Signal Intensity Change in the Pars Interarticularis and Adjacent Structures
- Pars Interarticularis Injections in a Patient with Spondylolysis: A case report
- Direct Repair of Pars Defects in Symptomatic Lumbar Spondylolysis Using Pedicle Screws and Universal Hooks : Preliminary Report
- Radiological Study of Spondylolysis in Korean Laborer
- The Clinical Outcomes of Exercise Therapy for a Soccer Player with Stress Fracture of Superior Pubic Ramus