A proposal: Atopic Dermatitis Organizer (ADO) guideline for children
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. childslee@skku.edu
- 2Environmental Health Center for Atopic Diseases, Samsung Medical Center, Seoul 135-710, Korea.
- KMID: 2397163
- DOI: http://doi.org/10.5415/apallergy.2011.1.2.53
Abstract
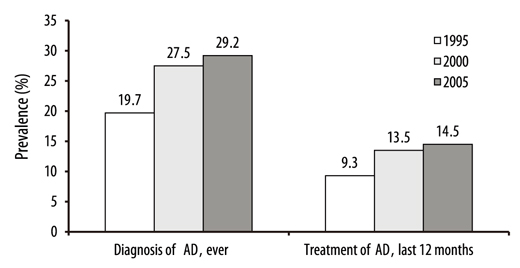
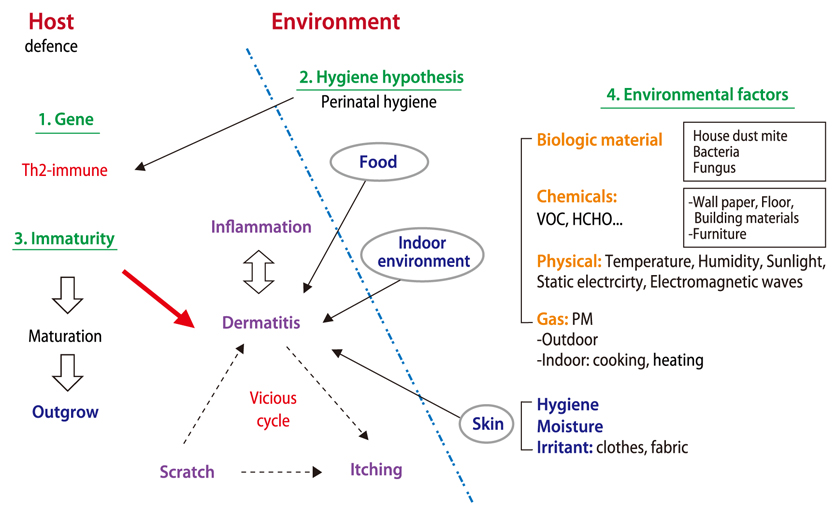
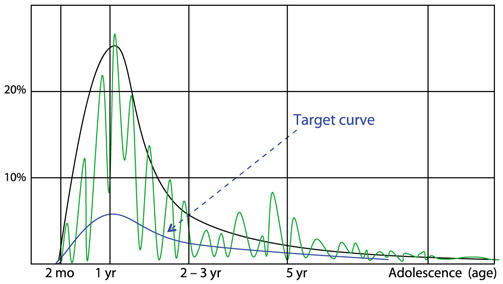
- Atopic dermatitis (AD) is the most common chronic inflammatory skin disorder in children, with a worldwide cumulative prevalence in children of 8-20%. The number of AD patients is beyond the level that can be dealt with at clinics and it is time to make an effort to reduce the number of AD patients in the community. Thus, caregivers and all persons involved with AD management, including health care providers, educators, technologists and medical policy makers, should understand the development and the management of AD. Although a number of guidelines such as Practical Allergy (PRACTALL) report have been developed and used, community understanding of these is low. This is probably because there are still remarkable differences in management practices between specialists and between countries and most of the reported guidelines have been prepared for physicians. From the viewpoint of providing a basis for a multidisciplinary team approach, easily comprehensible guidelines for organizing treatment of AD, i.e. an Atopic Dermatitis Organizer (ADO), are required. guidelines should be simple and well organized. We suggest an easy approach with a new classification of AD symptoms into early and/or progressive lesions in acute and/or chronic symptoms. The contents of this ADO guideline basically consist of 3 steps approaches: conservative management, topical anti-inflammatory therapy, and systemic anti-inflammatory therapy.
MeSH Terms
Figure
Cited by 7 articles
-
Association between parental history of allergic diseases and atopic dermatitis in school aged children
Young Man Kim, You Chan Kim, SooJin Lee, Joung Hwan Back, Kihong Chun
Allergy Asthma Respir Dis. 2014;2(5):377-382. doi: 10.4168/aard.2014.2.5.377.Sensitization in children with atopic dermatitis: a single center study
Ari Song, Ji Young Lee, Hea-kyoung Yang, Minji Kim, Kangmo Ahn, Sang-il Lee, Jihyun Kim
Allergy Asthma Respir Dis. 2016;4(4):290-295. doi: 10.4168/aard.2016.4.4.290.Early intervention in the management of atopic dermatitis
Donald Y.M. Leung
Asia Pac Allergy. 2011;1(2):51-52. doi: 10.5415/apallergy.2011.1.2.51.Effect of bathing on atopic dermatitis during the summer season
Hakyoung Kim, Jeongsuk Ban, Mi-Ran Park, Do-Soo Kim, Hye-Young Kim, Youngshin Han, Kangmo Ahn, Jihyun Kim
Asia Pac Allergy. 2012;2(4):269-274. doi: 10.5415/apallergy.2012.2.4.269.The Prevalence of Atopic Dermatitis in Korean Children
Kangmo Ahn
Allergy Asthma Immunol Res. 2016;8(1):1-2. doi: 10.4168/aair.2016.8.1.1.Clinical features of eczema herpeticum in atopic dermatitis in a single center
Hyun Ji Jang, Young Eun Rho, Kwanghoon Kim, Seong Heon Kim, Young Mi Kim, Hye-Young Kim
Allergy Asthma Respir Dis. 2018;6(3):174-178. doi: 10.4168/aard.2018.6.3.174.Beneficial Effect of Diet Intervention on School Children with Atopic Dermatitis
Jae Hyuck Lee, Seung Wan Hong, Sung-Ae Kim, Hee Joung Choi, Mi Kyung Kim, Young-Sung Suh
Korean J Health Promot. 2016;16(1):32-36. doi: 10.15384/kjhp.2016.16.1.32.
Reference
-
1. Johansson SG, Hourihane JO, Bousquet J, Bruijnzeel-Koomen C, Dreborg S, Haahtela T, Kowalski ML, Mygind N, Ring J, van Cauwenberge P, van Hage-Hamsten M, Wüthrich B. A revised nomenclature for allergy. An EAACI position statement from the EAACI nomenclature task force. Allergy. 2001. 56:813–824.
Article2. Purvis DJ, Thompson JM, Clark PM, Robinson E, Black PN, Wild CJ, Mitchell EA. Risk factors for atopic dermatitis in New Zealand children at 3.5 years of age. Br J Dermatol. 2005. 152:742–749.
Article3. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, Williams H. ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006. 368:733–743.
Article4. Williams H, Stewart A, von Mutius E, Cookson W, Anderson HR. International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008. 121:947–954.
Article5. Lee JH, Kim EH, Cho JB, Kim HY, Suh JM, Ahn KM, Cheong HK, Lee SI. Comparison of prevalence and risk factors of atopic dermatitis by physical examination and questionnaire survey in elementay school children. Pediatr Allergy Respir Dis. 2011. (Unpublished data).6. Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG. The prevalence of childhood atopic eczema in a general population. J Am Acad Dermatol. 1994. 30:35–39.
Article7. Rudolph AM. . Rudolph's pediatrics. 1991. 19th ed. Norwalk: Appleton & Lange.8. Illi S, von Mutius E, Lau S, Nickel R, Grüber C, Niggemann B, Wahn U. Multicenter Allergy Study Group. The natural course of atopic dermatitis from birth to age 7 years and the association with asthma. J Allergy Clin Immunol. 2004. 113:925–931.
Article9. Hong SJ. Korean ISAAC committee in Korean academy of pediatric allergy and respiratory disease. Report from Korean ISAAC committee. Pediatr Allergy Respir Dis. 2007. 17:S55–S66.10. Novak N, Kruse S, Potreck J, Maintz L, Jenneck C, Weidinger S, Fimmers R, Bieber T. Single nucleotide polymorphisms of the IL18 gene are associated with atopic eczema. J Allergy Clin Immunol. 2005. 115:828–833.
Article11. Weidinger S, Klopp N, Rummler L, Wagenpfeil S, Novak N, Baurecht HJ, Groer W, Darsow U, Heinrich J, Gauger A, Schafer T, Jakob T, Behrendt H, Wichmann HE, Ring J, Illig T. Association of NOD1 polymorphisms with atopic eczema and related phenotypes. J Allergy Clin Immunol. 2005. 116:177–184.
Article12. Weidinger S, Rümmler L, Klopp N, Wagenpfeil S, Baurecht HJ, Fischer G, Holle R, Gauger A, Schäfer T, Jakob T, Ollert M, Behrendt H, Wichmann HE, Ring J, Illig T. Association study of mast cell chymase polymorphisms with atopy. Allergy. 2005. 60:1256–1261.
Article13. Akdis CA, Akdis M, Bieber T, Bindslev-Jensen C, Boguniewicz M, Eigenmann P, Hamid Q, Kapp A, Leung DY, Lipozencic J, Luger TA, Muraro A, Novak N, Platts-Mills TA, Rosenwasser L, Scheynius A, Simons FE, Spergel J, Turjanmaa K, Wahn U, Weidinger S, Werfel T, Zuberbier T. European Academy of Allergology. Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Group. Diagnosis and treatment of atopic dermatitis in children and adults: European Academy of Allergology and Clinical Immunology/American Academy of Allergy, Asthma and Immunology/PRACTALL Consensus Report. Allergy. 2006. 61:969–987.
Article14. Kim HY, Jang EY, Sim JH, Kim JH, Chung Y, Park SH, Hwang EM, Han Y, Ahn K, Lee SI. Effects of family history on the occurrence of atopic dermatitis in infants. Pediatr Allergy Respir Dis. 2009. 19:106–114.15. Okada H, Kuhn C, Feillet H, Bach JF. The 'hygiene hypothesis' for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010. 160:1–9.
Article16. Williams H, Flohr C. How epidemiology has challenged 3 prevailing concepts about atopic dermatitis. J Allergy Clin Immunol. 2006. 118:209–213.
Article17. Zutavern A, Hirsch T, Leupold W, Weiland S, Keil U, von Mutius E. Atopic dermatitis, extrinsic atopic dermatitis and the hygiene hypothesis: results from a cross-sectional study. Clin Exp Allergy. 2005. 35:1301–1308.
Article18. Ibargoyen-Roteta N, Aguinaga-Ontoso I, Fernandez-Benitez M, Marin-Fernandez B, Guillen-Grima F, Serrano-Monzo I, Hermoso-demendoza J, Brun-Sandiumetge C, Ferrer-Nadal A, Irujo-Andueza A. Role of the home environment in rhinoconjunctivitis and eczema in schoolchildren in Pamplona, Spain. J Investig Allergol Clin Immunol. 2007. 17:137–144.19. Galeev KA, Khakimova RF. Relationship of the ambient air concentrations of chemical substances to the spread of allergic diseases in children. Gig Sanit. 2002. 23–24.20. Solé D, Camelo-Nunes IC, Wandalsen GF, Pastorino AC, Jacob CM, Gonzalez C, Wandalsen NF, Rosário Filho NA, Fischer GB, Naspitz CK. Prevalence of symptoms of asthma, rhinitis, and atopic eczema in Brazilian adolescents related to exposure to gaseous air pollutants and socioeconomic status. J Investig Allergol Clin Immunol. 2007. 17:6–13.21. Huss-Marp J, Eberlein-König B, Breuer K, Mair S, Ansel A, Darsow U, Krämer U, Mayer E, Ring J, Behrendt H. Influence of short-term exposure to airborne Der p 1 and volatile organic compounds on skin barrier function and dermal blood flow in patients with atopic eczema and healthy individuals. Clin Exp Allergy. 2006. 36:338–345.
Article22. Ring J, Eberlein-Koenig B, Behrendt H. Environmental pollution and allergy. Ann Allergy Asthma Immunol. 2001. 87:2–6.
Article23. Eberlein-König B, Przybilla B, Kühnl P, Pechak J, Gebefügi I, Kleinschmidt J, Ring J. Influence of airborne nitrogen dioxide or formaldehyde on parameters of skin function and cellular activation in patients with atopic eczema and control subjects. J Allergy Clin Immunol. 1998. 101:141–143.
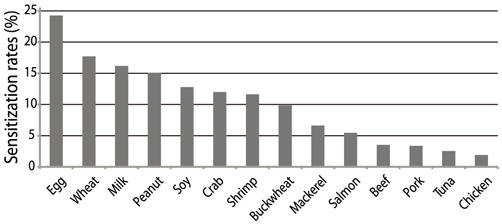
Article24. Sampson HA. The immunopathogenic role of food hypersensitivity in atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1992. 176:34–37.25. Leung DY. Infection in atopic dermatitis. Curr Opin Pediatr. 2003. 15:399–404.
Article26. Nomura I, Goleva E, Howell MD, Hamid QA, Ong PY, Hall CF, Darst MA, Gao B, Boguniewicz M, Travers JB, Leung DY. Cytokine milieu of atopic dermatitis, as compared to psoriasis, skin prevents induction of innate immune response genes. J Immunol. 2003. 171:3262–3269.
Article27. Suh L, Coffin S, Leckerman KH, Gelfand JM, Honig PJ, Yan AC. Methicillin-resistant Staphylococcus aureus colonization in children with atopic dermatitis. Pediatr Dermatol. 2008. 25:528–534.28. Palmer CN, Irvine AD, Terron-Kwiatkowski A, Zhao Y, Liao H, Lee SP, Goudie DR, Sandilands A, Campbell LE, Smith FJ, O'Regan GM, Watson RM, Cecil JE, Bale SJ, Compton JG, DiGiovanna JJ, Fleckman P, Lewis-Jones S, Arseculeratne G, Sergeant A, Munro CS, El Houate B, McElreavey K, Halkjaer LB, Bisgaard H, Mukhopadhyay S, McLean WH. Common loss-of-function variants of the epidermal barrier protein filaggrin are a major predisposing factor for atopic dermatitis. Nat Genet. 2006. 38:441–446.
Article29. Müller S, Marenholz I, Lee YA, Sengler C, Zitnik SE, Griffioen RW, Meglio P, Wahn U, Nickel R. Association of Filaggrin loss-of-function-mutations with atopic dermatitis and asthma in the Early Treatment of the Atopic Child (ETAC) population. Pediatr Allergy Immunol. 2009. 20:358–361.30. Hanifin JM, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol Suppl (Stockh). 1980. 92:44–47.31. Staldera JF, Taïebb A. Severity scoring of atopic dermatitis: the SCORAD index. Consensus report of the European task force on atopic dermatitis. Dermatology. 1993. 186:23–31.32. Hanifin JM, Cooper KD, Ho VC, Kang S, Krafchik BR, Margolis DJ, Schachner LA, Sidbury R, Whitmore SE, Sieck CK, Van Voorhees AS. Guidelines of care for atopic dermatitis, developed in accordance with the American Academy of Dermatology (AAD)/American Academy of Dermatology Association "Administrative Regulations for Evidence-Based Clinical Practice Guidelines". J Am Acad Dermatol. 2004. 50:391–404.33. Chamlin SL, Frieden IJ, Fowler A, Williams M, Kao J, Sheu M, Elias PM. Ceramide-dominant, barrier-repair lipids improve childhood atopic dermatitis. Arch Dermatol. 2001. 137:1110–1112.34. Grimalt R, Mengeaud V, Cambazard F. Study Investigator's Group. The steroid-sparing effect of an emollient therapy in infants with atopic dermatitis: a randomized controlled study. Dermatology. 2007. 214:61–67.
Article35. Anderson PC, Dinulos JG. Atopic dermatitis and alternative management strategies. Curr Opin Pediatr. 2009. 21:131–138.
Article36. Kim MB, Kim BJ, Seo YJ, Lee YW, Lee AY, Kim KH, Kim MN, Kim JW, Ro YS, Park YM, Park CW, Seo SJ, Lee KH, Cho SH, Choi JH. Skin care for atopic dermatitis. Korean J Dermatol. 2009. 47:531–538.37. Kim JY, Kwon JH, Ahn SH, Lee SI, Han YS, Choi YO, Lee SY, Ahn KM, Ji GE. Effect of probiotic mix (Bifidobacterium bifidum, Bifidobacterium lactis, Lactobacillus acidophilus) in the primary prevention of eczema: a double-blind, randomized, placebo-controlled trial. Pediatr Allergy Immunol. 2010. 21:e386–e393.38. Kim TH, Jung HH, Kim ES, Park JY, Kim KW, Sohn MH, Kim KE. A case of rice allergy caused by thin rice porridge during the weaning period. Pediatr Allergy Respir Dis. 2007. 17:149–154.39. Ahn YH, Yeo JS, Lee JY, Han YS, Ahn KM, Lee SI. Effects of cooking methods on peanut allergenicity. Pediatr Allergy Respir Dis. 2009. 19:233–240.40. Scalabrin DM, Bavbek S, Perzanowski MS, Wilson BB, Platts-Mills TA, Wheatley LM. Use of specific IgE in assessing the relevance of fungal and dust mite allergens to atopic dermatitis: a comparison with asthmatic and nonasthmatic control subjects. J Allergy Clin Immunol. 1999. 104:1273–1279.
Article41. Mitchell EB, Crow J, Chapman MD, Jouhal SS, Pope FM, Platts-Mills TA. Basophils in allergen-induced patch test sites in atopic dermatitis. Lancet. 1982. 1:127–130.
Article42. Tan BB, Weald D, Strickland I, Friedmann PS. Double-blind controlled trial of effect of housedust-mite allergen avoidance on atopic dermatitis. Lancet. 1996. 347:15–18.
Article43. Platts-Mills TA, Mitchell EB, Rowntree S, Chapman MD, Wilkins SR. The role of dust mite allergens in atopic dermatitis. Clin Exp Dermatol. 1983. 8:233–247.
Article44. Capristo C, Romei I, Boner AL. Environmental prevention in atopic eczema dermatitis syndrome (AEDS) and asthma: avoidance of indoor allergens. Allergy. 2004. 59:Suppl 78. 53–60.
Article45. Roberts DL. House dust mite avoidance and atopic dermatitis. Br J Dermatol. 1984. 110:735–736.
Article46. August PJ. The environmental causes and management of eczema. Practitioner. 1987. 231:495–500.47. Zingarelli G, editor. Atopic dermatitis. Australian doctor - How to treat. Available from: http://www.australiandoctor.com.au//htt/pdf/AD_029_036_APR16_10.pdf.48. Wahlgren CF, Hägermark O, Bergström R. The antipruritic effect of a sedative and a non-sedative antihistamine in atopic dermatitis. Br J Dermatol. 1990. 122:545–551.
Article49. Harper J, Oranje AP, Prose NS. Textbook of pediatric dermatology. 2000. 1st ed. Oxford: Blackwell Science.50. Seidenari S, Giusti G. Objective assessment of the skin of children affected by atopic dermatitis: a study of pH, capacitance and TEWL in eczematous and clinically uninvolved skin. Acta Derm Venereol. 1995. 75:429–433.51. Ong PY, Ohtake T, Brandt C, Strickland I, Boguniewicz M, Ganz T, Gallo RL, Leung DY. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002. 347:1151–1160.
Article52. Scheynius A, Johansson C, Buentke E, Zargari A, Linder MT. Atopic eczema/dermatitis syndrome and Malassezia. Int Arch Allergy Immunol. 2002. 127:161–169.53. Thomas KS, Armstrong S, Avery A, Po AL, O'Neill C, Young S, Williams HC. Randomised controlled trial of short bursts of a potent topical corticosteroid versus prolonged use of a mild preparation for children with mild or moderate atopic eczema. BMJ. 2002. 324:768.
Article54. Long CC, Finlay AY. The finger-tip unit--a new practical measure. Clin Exp Dermatol. 1991. 16:444–447.
Article55. Hultsch T, Kapp A, Spergel J. Immunomodulation and safety of topical calcineurin inhibitors for the treatment of atopic dermatitis. Dermatology. 2005. 211:174–187.
Article56. Wahn U, Bos JD, Goodfield M, Caputo R, Papp K, Manjra A, Dobozy A, Paul C, Molloy S, Hultsch T, Graeber M, Cherill R, de Prost Y. Flare Reduction in Eczema with Elidel (Children) Multicenter Investigator Study Group. Efficacy and safety of pimecrolimus cream in the long-term management of atopic dermatitis in children. Pediatrics. 2002. 110:e2.
Article57. Queille-Roussel C, Paul C, Duteil L, Lefebvre MC, Rapatz G, Zagula M, Ortonne JP. The new topical ascomycin derivative SDZ ASM 981 does not induce skin atrophy when applied to normal skin for 4 weeks: a randomized, double-blind controlled study. Br J Dermatol. 2001. 144:507–513.58. Boguniewicz M, Nicol N, Kelsay K, Leung DY. A multidisciplinary approach to evaluation and treatment of atopic dermatitis. Semin Cutan Med Surg. 2008. 27:115–127.
Article59. Zheng T, Yu J, Oh MH, Zhu Z. The atopic march: progression from atopic dermatitis to allergic rhinitis and asthma. Allergy Asthma Immunol Res. 2011. 3:67–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The KAPARD guidelines for atopic dermatitis in children and adolescents: Part II. Systemic treatment, novel therapeutics, and adjuvant therapy
- Measurement of Atopic Dermatitis Disability
- Serum IgE Level in Patients of Atopic Dermatitis and Atopic Dermatitis with Molluscum Contagiosum
- Update on management of pediatric atopic dermatitis
- Therapeutic approach to atopic dermatitis in children