Asia Pac Allergy.
2014 Oct;4(4):222-229. 10.5415/apallergy.2014.4.4.222.
The impact of sinusitis on the long-term clinical outcomes of asthma
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul 110-799, Korea. helenmed@snu.ac.kr
- 2Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul 110-799, Korea.
- 3Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul 158-710, Korea.
- 4Department of Internal Medicine, Chung-Ang University Hospital, Seoul 156-755, Korea.
- KMID: 2397103
- DOI: http://doi.org/10.5415/apallergy.2014.4.4.222
Abstract
- BACKGROUND
Upper respiratory diseases have been linked with lower respiratory diseases. However, the long-term effect of sinusitis on the clinical outcomes of asthma has not been fully evaluated.
OBJECTIVE
The aim of this study was to investigate the impact of sinusitis on the disease progression of asthma.
METHODS
Seventy-five asthmatic patients confirmed with the methacholine bronchial provocation test or bronchodilator response were included. The study patients underwent paranasal sinus x-ray upon their asthma evaluation and they visited the hospital at least 3 years or longer. We retrospectively reviewed their medical records and compared data according to the presence of comorbid sinusitis.
RESULTS
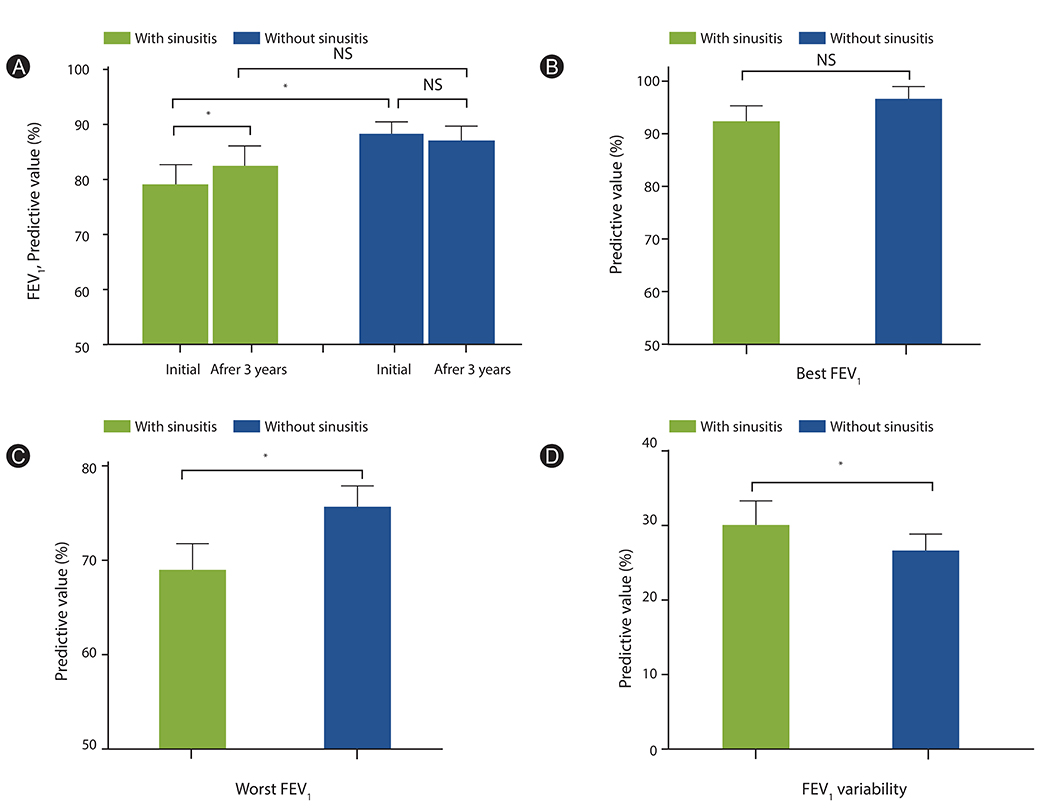
Among the 75 asthmatic subjects, 38 subjects (50.7%) had radiologic evidence of sinusitis. Asthmatics with sinusitis had significantly lower forced expiratory volume in 1 second (FEVâ‚; 79.2% vs. 88.2%) and PC20 values (5.2 mg/mL vs. 8.9 mg/mL) compared to asthmatics without sinusitis at the time of diagnosis. This difference in FEVâ‚ disappeared (82.6% vs. 87.2%) in the 3-year follow-up, although FEVâ‚ was more variable (31.7% vs. 23.5%) and worst FEVâ‚ was also significantly lower in patients with sinusitis compared to those without (70.9% vs. 79.0%). There were no significant differences in the number of hospital visits, acute exacerbations, and scores for the asthma control test.
CONCLUSION
Although sinusitis was associated with lower baseline lung function and higher hyperreactivity, sinusitis was not related with significant deterioration in lung function over 3 years of follow-up. Asthmatics with sinusitis showed more variability in lung function during the follow-up period. Healthcare utilization was not different except antibiotics use.
MeSH Terms
Figure
Cited by 1 articles
-
In the memory of Professor Felicidad Cua-Lim
Yoon-Seok Chang
Asia Pac Allergy. 2014;4(4):185-186. doi: 10.5415/apallergy.2014.4.4.185.
Reference
-
1. Hellings PW, Hens G. Rhinosinusitis and the lower airways. Immunol Allergy Clin North Am. 2009; 29:733–740.
Article2. Boulet LP, Boulay ME. Asthma-related comorbidities. Expert Rev Respir Med. 2011; 5:377–393.
Article3. Jani AL, Hamilos DL. Current thinking on the relationship between rhinosinusitis and asthma. J Asthma. 2005; 42:1–7.
Article4. Bresciani M, Paradis L, Des Roches A, Vernhet H, Vachier I, Godard P, Bousquet J, Chanez P. Rhinosinusitis in severe asthma. J Allergy Clin Immunol. 2001; 107:73–80.
Article5. ten Brinke A, Grootendorst DC, Schmidt JT, De Bruïne FT, van Buchem MA, Sterk PJ, Rabe KF, Bel EH. Chronic sinusitis in severe asthma is related to sputum eosinophilia. J Allergy Clin Immunol. 2002; 109:621–626.
Article6. Rachelefsky GS, Katz RM, Siegel SC. Chronic sinus disease with associated reactive airway disease in children. Pediatrics. 1984; 73:526–529.
Article7. Friedman R, Ackerman M, Wald E, Casselbrant M, Friday G, Fireman P. Asthma and bacterial sinusitis in children. J Allergy Clin Immunol. 1984; 74:185–189.
Article8. Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, Murray JJ, Pendergraft TB. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004; 113:59–65.9. Chai H. Antigen and methacholine challenge in children with asthma. J Allergy Clin Immunol. 1979; 64(6 pt 2):575–579.
Article10. Stelmach R, Junior SA, Figueiredo CM, Uezumi K, Genu AM, Carvalho-Pinto RM, Cukier A. Chronic rhinosinusitis in allergic asthmatic patients: radiography versus low-dose computed tomography evaluation. J Asthma. 2010; 47:599–603.
Article11. Laprise C, Boulet LP. Asymptomatic airway hyperresponsiveness: a three-year follow-up. Am J Respir Crit Care Med. 1997; 156(2 Pt 1):403–409.
Article12. Jarvis D, Newson R, Lotvall J, Hastan D, Tomassen P, Keil T, Gjomarkaj M, Forsberg B, Gunnbjornsdottir M, Minov J, Brozek G, Dahlen SE, Toskala E, Kowalski ML, Olze H, Howarth P, Kramer U, Baelum J, Loureiro C, Kasper L, Bousquet PJ, Bousquet J, Bachert C, Fokkens W, Burney P. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy. 2012; 67:91–98.
Article13. Dixon AE, Kaminsky DA, Holbrook JT, Wise RA, Shade DM, Irvin CG. Allergic rhinitis and sinusitis in asthma: differential effects on symptoms and pulmonary function. Chest. 2006; 130:429–435.14. Litvack JR, Fong K, Mace J, James KE, Smith TL. Predictors of olfactory dysfunction in patients with chronic rhinosinusitis. Laryngoscope. 2008; 118:2225–2230.
Article15. Bachert C, Zhang N, Holtappels G, De Lobel L, van Cauwenberge P, Liu S, Lin P, Bousquet J, Van Steen K. Presence of IL-5 protein and IgE antibodies to staphylococcal enterotoxins in nasal polyps is associated with comorbid asthma. J Allergy Clin Immunol. 2010; 126:962–968. 968.e1–968.e6.
Article16. ten Brinke A, Sterk PJ, Masclee AA, Spinhoven P, Schmidt JT, Zwinderman AH, Rabe KF, Bel EH. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J. 2005; 26:812–818.
Article17. Lotvall J, Ekerljung L, Lundback B. Multi-symptom asthma is closely related to nasal blockage, rhinorrhea and symptoms of chronic rhinosinusitis-evidence from the West Sweden Asthma Study. Respir Res. 2010; 11:163.
Article18. Braunstahl GJ, Fokkens W. Nasal involvement in allergic asthma. Allergy. 2003; 58:1235–1243.
Article19. Tomassen P, Van Zele T, Zhang N, Perez-Novo C, Van Bruaene N, Gevaert P, Bachert C. Pathophysiology of chronic rhinosinusitis. Proc Am Thorac Soc. 2011; 8:115–120.
Article20. Fuhlbrigge AL, Adams RJ. The effect of treatment of allergic rhinitis on asthma morbidity, including emergency department visits. Curr Opin Allergy Clin Immunol. 2003; 3:29–32.
Article21. Stelmach R, do Patrocinio T Nunes M, Ribeiro M, Cukier A. Effect of treating allergic rhinitis with corticosteroids in patients with mild-to-moderate persistent asthma. Chest. 2005; 128:3140–3147.
Article22. Choi SH, Kim do K, Yoo Y, Yu J, Koh YY. Comparison of deltaFVC between patients with allergic rhinitis with airway hypersensitivity and patients with mild asthma. Ann Allergy Asthma Immunol. 2007; 98:128–133.23. Ciprandi G, Cirillo I, Pistorio A. Impact of allergic rhinitis on asthma: effects on spirometric parameters. Allergy. 2008; 63:255–260.24. Guerra S, Sherrill DL, Martinez FD, Barbee RA. Rhinitis as an independent risk factor for adult-onset asthma. J Allergy Clin Immunol. 2002; 109:419–425.
Article25. Sherrill DL, Guerra S, Minervini MC, Wright AL, Martinez FD. The relation of rhinitis to recurrent cough and wheezing: a longitudinal study. Respir Med. 2005; 99:1377–1385.
Article26. Ponikau JU, Sherris DA, Kephart GM, Kern EB, Gaffey TA, Tarara JE, Kita H. Features of airway remodeling and eosinophilic inflammation in chronic rhinosinusitis: is the histopathology similar to asthma? J Allergy Clin Immunol. 2003; 112:877–882.27. Jaaskelainen IP, Ahveninen J, Andermann ML, Belliveau JW, Raij T, Sams M. Short-term plasticity as a neural mechanism supporting memory and attentional functions. Brain Res. 2011; 1422:66–81.28. Senior BA, Kennedy DW, Tanabodee J, Kroger H, Hassab M, Lanza DC. Long-term impact of functional endoscopic sinus surgery on asthma. Otolaryngol Head Neck Surg. 1999; 121:66–68.
Article29. Manning SC, Wasserman RL, Silver R, Phillips DL. Results of endoscopic sinus surgery in pediatric patients with chronic sinusitis and asthma. Arch Otolaryngol Head Neck Surg. 1994; 120:1142–1145.
Article30. Palmer JN, Conley DB, Dong RG, Ditto AM, Yarnold PR, Kern RC. Efficacy of endoscopic sinus surgery in the management of patients with asthma and chronic sinusitis. Am J Rhinol. 2001; 15:49–53.
Article31. Ikeda K, Tanno N, Tamura G, Suzuki H, Oshima T, Shimomura A, Nakabayashi S, Takasaka T. Endoscopic sinus surgery improves pulmonary function in patients with asthma associated with chronic sinusitis. Ann Otol Rhinol Laryngol. 1999; 108:355–359.
Article32. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011; 128:693–707.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Allergic rhinitis, sinusitis and asthma: evidence for respiratory system integration
- A significance of the sinusitis in asthma of children
- Allergy Fungal Sinusitis
- Clinical Characteristics of Chronic Sinusitis with Asthma
- Successful Role of Endoscopic Sinus Surgery in an Asthmatic Patient Associated with Kartagener's Syndrome