Asia Pac Allergy.
2017 Apr;7(2):92-96. 10.5415/apallergy.2017.7.2.92.
Medical certification reduces the number of children requiring allergen elimination diets for school lunches
- Affiliations
-
- 1Division of Educational Support for Regional Pediatrics, Oita University Faculty of Medicine, Oita 879-5593, Japan. kseigo@oita-u.ac.jp
- 2Department of Pediatrics, Oita University Faculty of Medicine, Oita 879-5593, Japan.
- 3Kunisaki City Hospital, Kunisaki 873-0231, Japan.
- KMID: 2396930
- DOI: http://doi.org/10.5415/apallergy.2017.7.2.92
Abstract
- BACKGROUND
Following the increase in the number of children with food allergies, support systems are now required for school lunches, but a large-scale factual investigation has not been carried out.
OBJECTIVE
We evaluated the features of elimination diet due to food allergy and the support system in kindergartens and schools.
METHODS
A prefecture-based questionnaire survey regarding measures for food allergies in school lunches of all kindergartens, public elementary schools, and public junior high schools (631 facilities) was conducted in Oita Prefecture, Japan.
RESULTS
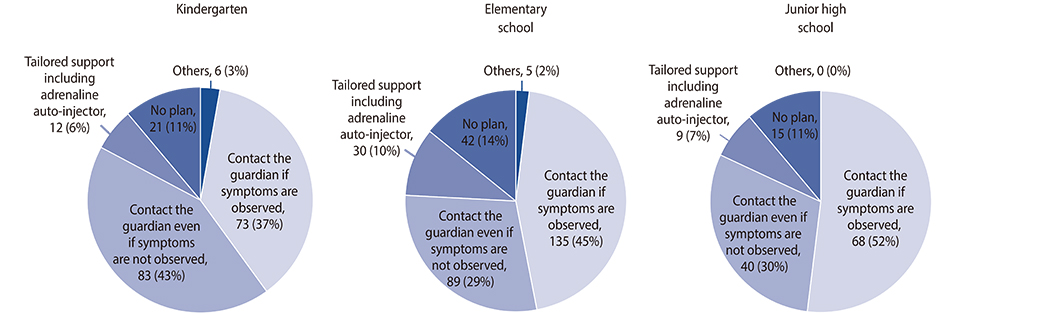
The recovery rate of the questionnaire was 99.5%, which included 106,008 students in total. A total of 1,562 children (1.5%) required elimination diets. The rate of children on elimination diets in kindergartens and elementary/junior high schools that required medical certification by a physician was 1.2% (324 among 27,761 children), which was significantly lower than the 1.8% of children (1,227 among 68,576 students) on elimination diets at the request of guardians without the need for medical certification (p < 0.0001). A total of 43.9% of the kindergartens and schools said that they would contact guardians if symptoms were observed after accidental ingestion, while a low 8.1% stated that they provided support to children themselves, including the administration of adrenaline auto-injectors.
CONCLUSION
Medical certification reduces the number of children requiring elimination diets, but it has not been adequately implemented. Furthermore, waiting to contact guardians after symptoms are observed may lead to the delayed treatment of anaphylaxis. Cooperation between physicians and teachers is desired to avoid the overdiagnosis and undertreatment of children with food allergies.
MeSH Terms
Figure
Reference
-
1. Simons FE, Ebisawa M, Sanchez-Borges M, Thong BY, Worm M, Tanno LK, Lockey RF, El-Gamal YM, Brown SG, Park HS, Sheikh A. 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organ J. 2015; 8:32.
Article2. Ward CE, Greenhawt MJ. Treatment of allergic reactions and quality of life among caregivers of food-allergic children. Ann Allergy Asthma Immunol. 2015; 114:312–318.e2.
Article3. Sandin A, Annus T, Björkstén B, Nilsson L, Riikjärv MA, van Hage-Hamsten M, Bråbäck L. Prevalence of self-reported food allergy and IgE antibodies to food allergens in Swedish and Estonian schoolchildren. Eur J Clin Nutr. 2005; 59:399–403.
Article4. Urisu A, Ebisawa M, Ito K, Aihara Y, Ito S, Mayumi M, Kohno Y, Kondo N. Committee for Japanese Pediatric Guideline for Food Allergy. Japanese Society of Pediatric Allergy and Clinical Immunology. Japanese Society of Allergology. Japanese Guideline for Food Allergy 2014. Allergol Int. 2014; 63:399–419.
Article5. Ohtani K, Sato S, Syukuya A, Asaumi T, Ogura K, Koike Y, Iikura K, Yanagida N, Imai T, Ebisawa M. Natural history of immediate-type hen's egg allergy in Japanese children. Allergol Int. 2016; 65:153–157.
Article6. Meyer R, De Koker C, Dziubak R, Venter C, Dominguez-Ortega G, Cutts R, Yerlett N, Skrapak AK, Fox AT, Shah N. Malnutrition in children with food allergies in the UK. J Hum Nutr Diet. 2014; 27:227–235.
Article7. Gandy LT, Yadrick MK, Boudreaux LJ, Smith ER. Serving children with special health care needs: nutrition services and employee training needs in the school lunch program. J Am Diet Assoc. 1991; 91:1585–1586.
Article8. Rhim GS, McMorris MS. School readiness for children with food allergies. Ann Allergy Asthma Immunol. 2001; 86:172–176.
Article9. Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001; 155:790–795.
Article10. Kim S, Yoon J, Kwon S, Kim J, Han Y. Current status of managing food allergies in schools in Seoul, Korea. J Child Health Care. 2012; 16:406–416.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of obesity on the Satisfaction with School Lunches and the Behavior of Leaving Lunch Food in Elementary School Children
- Dietary Quality Comparison of the School and Home Lunches Consumed by Chinese School-Age Children and Adolescents:Analysis of the 2011 China Health and Nutrition Survey
- Nutritional quality of lunches consumed by Korean workers: Comparison between institutional and commercial lunches
- Indoor Allergen Avoidance and Asthma
- Association of Descriptive Menu Names and Number of Correctly Vegetable Names with Factors Regarding Vegetable Intake in Elementary School Children