Korean Circ J.
2017 Nov;47(6):970-977. 10.4070/kcj.2016.0364.
Pericardial-esophageal Fistula Complicating Atrial Fibrillation Ablation Successfully Resolved after Pericardial Drainage with Conservative Management
- Affiliations
-
- 1Department of Cardiology, Cardio-Cerebrovascular Center, Dong-A University Hospital, Busan, Korea. thinkmed@dau.ac.kr
- 2Department of Thoracic Surgery, Cardio-Cerebrovascular Center, Dong-A University Hospital, Busan, Korea.
- KMID: 2396490
- DOI: http://doi.org/10.4070/kcj.2016.0364
Abstract
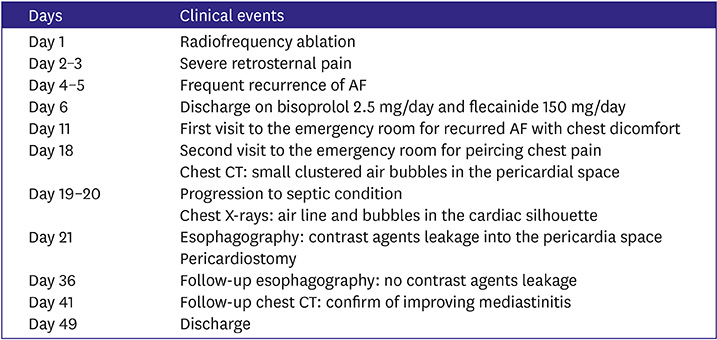
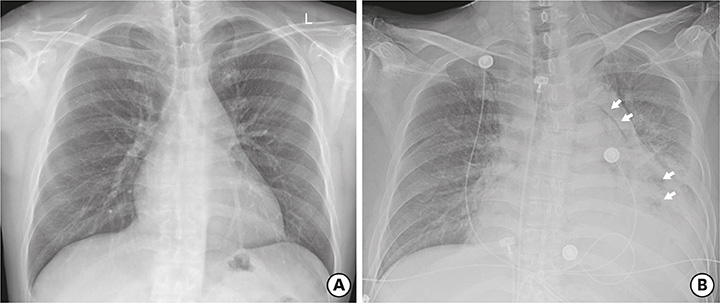
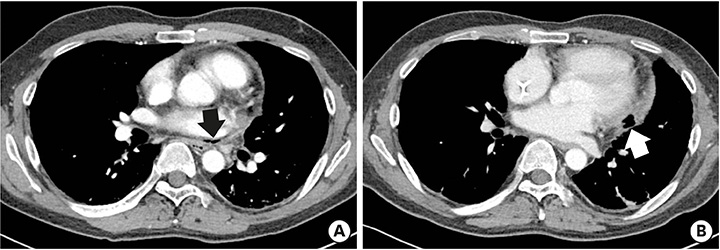
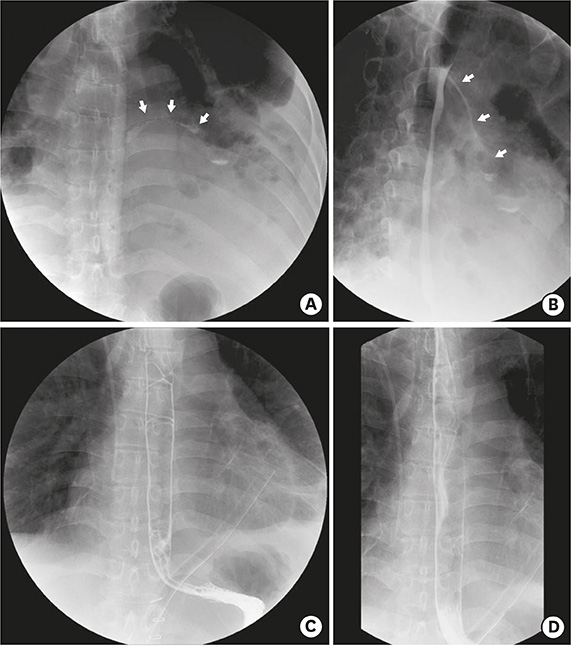
- A 40-year-old male patient underwent radiofrequency catheter ablation for symptomatic paroxysmal atrial fibrillation (AF). Although pulmonary vein (PV) isolation was successfully completed without acute complications, the patient began complaining of sustained retrosternal pain. Seventeen days after ablation, the patient visited the emergency room with fever and severe chest pain with pericarditis-like features. Chest computed tomography (CT) revealed clustered air bubbles in the pericardial space. Esophagography confirmed leakage of contrast agent into the pericardial space but not into the left atrium. While performing pericardiostomy, the operator confirmed the absence of active bleeding from the left atrium. Because there were no signs of left atrial-esophageal fistula, such as systemic embolization, conservative management based on strict fasting with fluids and antibiotic therapy was undertaken. Follow-up esophagography performed 2 weeks later showed no more contrast agent leakage, and the patient was discharged without further incident.
MeSH Terms
Figure
Reference
-
1. Ghia KK, Chugh A, Good E, et al. A nationwide survey on the prevalence of atrioesophageal fistula after left atrial radiofrequency catheter ablation. J Interv Card Electrophysiol. 2009; 24:33–36.2. Cappato R, Calkins H, Chen SA, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010; 3:32–38.3. Barbhaiya CR, Kumar S, John RM, et al. Global survey of esophageal and gastric injury in atrial fibrillation ablation: incidence, time to presentation, and outcomes. J Am Coll Cardiol. 2015; 65:1377–1378.4. Pappone C, Oral H, Santinelli V, et al. Atrio-esophageal fistula as a complication of percutaneous transcatheter ablation of atrial fibrillation. Circulation. 2004; 109:2724–2726.5. Dagres N, Kottkamp H, Piorkowski C, et al. Rapid detection and successful treatment of esophageal perforation after radiofrequency ablation of atrial fibrillation: lessons from five cases. J Cardiovasc Electrophysiol. 2006; 17:1213–1215.6. Eitel C, Rolf S, Zachäus M, et al. Successful nonsurgical treatment of esophagopericardial fistulas after atrial fibrillation catheter ablation: a case series. Circ Arrhythm Electrophysiol. 2013; 6:675–681.7. Shalaby A, Refaat M, Sebastien G, Zenati M. Conservative management of pericardial-esophageal fistula complicating robotic atrial fibrillation ablation. Heart Rhythm. 2011; 8:905–908.8. Quénéhervé L, Musquer N, Léauté F, Coron E. Endoscopic management of an esophagopericardial fistula after radiofrequency ablation for atrial fibrillation. World J Gastroenterol. 2013; 19:3352–3353.9. Bailey CW, Tallaksen RJ. Pericardioesophageal fistula following left atrial ablation procedure. J Radiol Case Rep. 2014; 8:23–31.10. Schmidt M, Nölker G, Marschang H, et al. Incidence of oesophageal wall injury post-pulmonary vein antrum isolation for treatment of patients with atrial fibrillation. Europace. 2008; 10:205–209.11. Zellerhoff S, Ullerich H, Lenze F, et al. Damage to the esophagus after atrial fibrillation ablation: Just the tip of the iceberg? High prevalence of mediastinal changes diagnosed by endosonography. Circ Arrhythm Electrophysiol. 2010; 3:155–159.12. Ripley KL, Gage AA, Olsen DB, Van Vleet JF, Lau CP, Tse HF. Time course of esophageal lesions after catheter ablation with cryothermal and radiofrequency ablation: implication for atrio-esophageal fistula formation after catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2007; 18:642–646.13. Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society. Heart Rhythm. 2012; 9:632–696.e21.14. Hornero F, Berjano EJ. Esophageal temperature during radiofrequency-catheter ablation of left atrium: a three-dimensional computer modeling study. J Cardiovasc Electrophysiol. 2006; 17:405–410.15. Di Biase L, Saenz LC, Burkhardt DJ, et al. Esophageal capsule endoscopy after radiofrequency catheter ablation for atrial fibrillation: documented higher risk of luminal esophageal damage with general anesthesia as compared with conscious sedation. Circ Arrhythm Electrophysiol. 2009; 2:108–112.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Management of Atrio-Esophageal Fistula after Cardiac Radiofrequency Catheter Ablation
- Persistent Atrial Fibrillation Related to a Congenital Pericardial Defect and Left Atrial Appendage Herniation
- Hemodynamic Change before and after Serial Fluid Drainage in Patients with Chronic Pericardial Effusion
- A Case of Pyogenic Liver Abscess Complicating Cardiac Tamponade Caused by Klebsiella pneumoniae
- Radiofrequency Catheter Ablation of Persistent Atrial Fibrillation with Myotonic Dystrophy and Achalasia-like Esophageal Dilatation