Intest Res.
2017 Oct;15(4):518-523. 10.5217/ir.2017.15.4.518.
Predictive factors for malignancy in undiagnosed isolated small bowel strictures
- Affiliations
-
- 1Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi, India.
- 2Department of GI Surgery, All India Institute of Medical Sciences, New Delhi, India. peush_sahni@hotmail.com
- 3Department of Pathology, All India Institute of Medical Sciences, New Delhi, India.
- KMID: 2396402
- DOI: http://doi.org/10.5217/ir.2017.15.4.518
Abstract
- BACKGROUND/AIMS
Patients with small bowel strictures have varied etiologies, including malignancy. Little data are available on the demographic profiles and etiologies of small bowel strictures in patients who undergo surgery because of intestinal obstruction but do not have a definitive pre-operative diagnosis.
METHODS
Retrospective data were analyzed for all patients operated between January 2000 and October 2014 for small bowel strictures without mass lesions and a definite diagnosis after imaging and endoscopic examinations. Demographic parameters, imaging, endoscopic, and histological data were extracted from the medical records. Univariate and multivariate analyses were conducted to identify factors that could differentiate between intestinal tuberculosis (ITB) and Crohn's disease (CD) and between malignant and benign strictures.
RESULTS
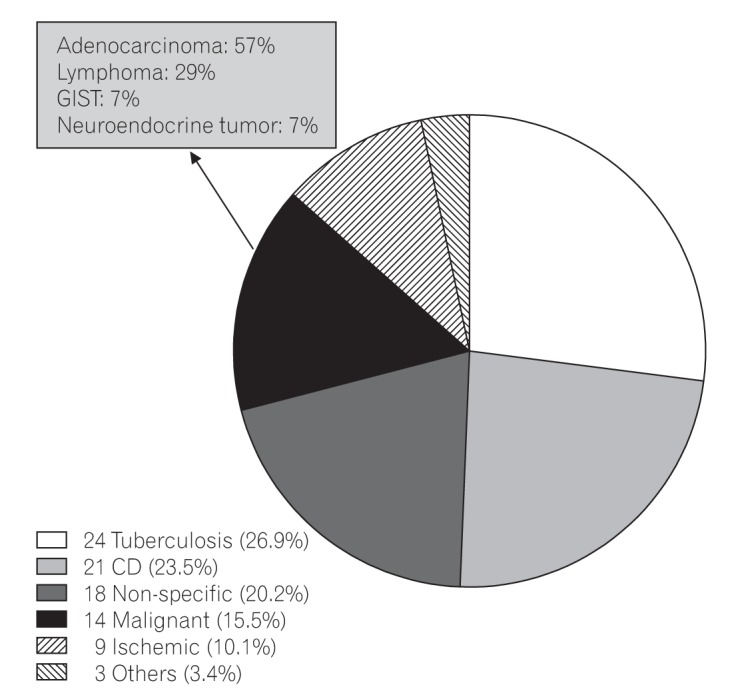
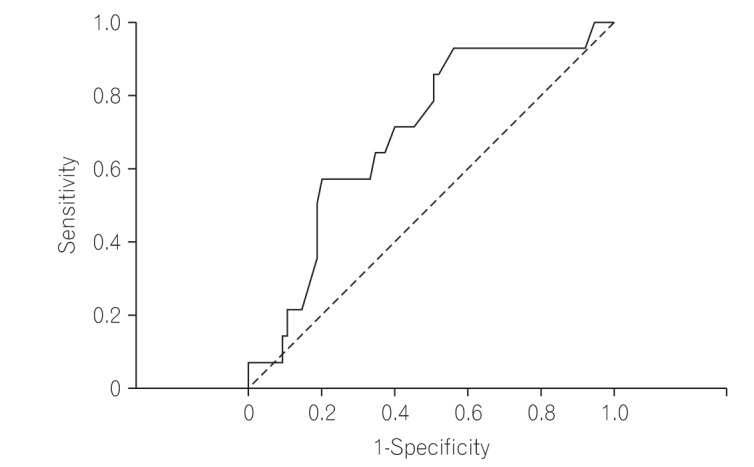
Of the 7,425 reviewed medical records, 89 met the inclusion criteria. The most common site of strictures was the proximal small intestine (41.5%). The most common histological diagnoses in patients with small bowel strictures were ITB (26.9%), CD (23.5%), non-specific strictures (20.2%), malignancy (15.5%), ischemia (10.1%), and other complications (3.4%). Patients with malignant strictures were older than patients with benign etiologies (47.6±15.9 years vs. 37.4±16.4 years, P=0.03) and age >50 years had a specificity for malignant etiology of 80%. Only 7.1% of the patients with malignant strictures had more than 1 stricture and 64% had proximally located strictures. Diarrhea was the only factor that predicted the diagnosis of CD 6.5 (95% confidence interval, 1.10-38.25; P=0.038) compared with the diagnosis of ITB.
CONCLUSIONS
Malignancy was the cause of small bowel strictures in approximately 16% patients, especially among older patients with a single stricture in the proximal location. Empirical therapy should be avoided and the threshold for surgical resection is low in these patients.
MeSH Terms
Figure
Reference
-
1. Kelly ME, McMahon LE, Jaroszewski DE, Yousfi MM, De Petris G, Swain JM. Small-bowel diaphragm disease: seven surgical cases. Arch Surg. 2005; 140:1162–1166. PMID: 16365236.2. Wang ML, Miao F, Tang YH, Zhao XS, Zhong J, Yuan F. Special diaphragm-like strictures of small bowel unrelated to non-steroidal anti-inflammatory drugs. World J Gastroenterol. 2011; 17:3596–3604. PMID: 21987606.
Article3. Patel S, Gurjar SV. Small intestinal strictures as a complication of mesenteric vessel thrombosis: two case reports. J Med Case Rep. 2009; 3:8623.
Article4. Honzawa Y, Kondo M, Hayakumo T, Matsuura M, Nakase H. Successful endoscopic dilation treatment of small intestinal stricture occurring during chemotherapy for malignant lymphoma. Case Rep Gastroenterol. 2010; 4:323–329. PMID: 21060694.
Article5. Ahuja V, Tandon RK. Inflammatory bowel disease in the Asia-Pacific area: a comparison with developed countries and regional differences. J Dig Dis. 2010; 11:134–147. PMID: 20579217.
Article6. Ahuja V, Tandon RK. Inflammatory bowel disease: the Indian augury. Indian J Gastroenterol. 2012; 31:294–296. PMID: 23150035.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Diagnosis and Treatment of Benign Small Bowel Stricture
- Current status of endoscopic balloon dilation for Crohn's disease
- Isolated Small Bowel Metastasis of Endometrial Carcinoma with Resultant Jejunojejunal Intussusception: A Case Report
- Small Bowel Obstruction and Capsule Retention by a Small Bowel Ulcer That Was Not Found on Capsule Endoscopy
- Radiologic Review of Small Bowel Malignancies and Their Mimicking Lesions