J Korean Med Sci.
2017 Dec;32(12):2058-2063. 10.3346/jkms.2017.32.12.2058.
Efficacy of Uncross-Matched Type O Packed Red Blood Cell Transfusion to Traumatic Shock Patients: a Propensity Score Match Study
- Affiliations
-
- 1Department of Trauma Surgery, Ajou University School of Medicine, Suwon, Korea. ajoutraumacenter@gmail.com
- 2Department of Trauma Surgery, National Medical Center, Seoul, Korea.
- KMID: 2396386
- DOI: http://doi.org/10.3346/jkms.2017.32.12.2058
Abstract
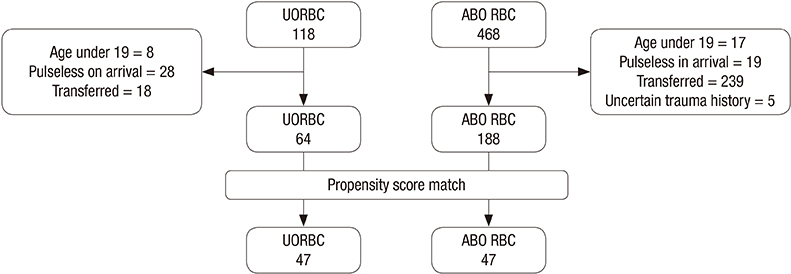
- A new blood bank system was established in our trauma bay, which allowed immediate utilization of uncross-matched type O packed red blood cells (UORBCs). We investigated the efficacy of UORBC compared to that of the ABO type-specific packed red blood cells (ABO RBCs) from before the bank was installed. From March 2016 to February 2017, data from trauma patients who received UORBCs in the trauma bay were compared with those of trauma patients who received ABO RBCs from January 2013 to December 2015. Propensity matching was used to overcome retrospective bias. The primary outcome was 24-hour mortality, while the secondary outcomes were in-hospital mortality and intensive care unit (ICU) length of stay (LOS). Data from 252 patients were reviewed and UORBCs were administered to 64 patients. The time to transfusion from emergency room admission was shorter in the UORBC group (11 [7-16] minutes vs. 44 [29-72] minutes, P < 0.001). After propensity matching, 47 patients were included in each group. The 24-hour mortality (4 [8.5%] vs. 9 [13.8%], P = 0.135), in-hospital mortality (14 [29.8%] vs. 18 [38.3%], P = 0.384), and ICU LOS (9 [4-19] days vs. 5 [0-19] days, P = 0.155) did not differ significantly between groups. The utilization of UORBCs resulted in a faster transfusion but did not significantly improve the clinical outcomes in traumatic shock patients in this study. However, the tendency for lower mortality in the UORBC group suggested the need for a large study.
MeSH Terms
Figure
Reference
-
1. Ahn E, Choi SH, Kim JY, Park JH, Cho YD. Analysis of trauma patients with massive transfusion in the emergency department. Korean J Blood Transfus. 2016; 27:130–136.2. Bjerkvig CK, Strandenes G, Eliassen HS, Spinella PC, Fosse TK, Cap AP, Ward KR. “Blood failure” time to view blood as an organ: how oxygen debt contributes to blood failure and its implications for remote damage control resuscitation. Transfusion. 2016; 56:Suppl 2. S182–S189.3. Alarhayem AQ, Myers JG, Dent D, Liao L, Muir M, Mueller D, Nicholson S, Cestero R, Johnson MC, Stewart R, et al. Time is the enemy: mortality in trauma patients with hemorrhage from torso injury occurs long before the “golden hour”. Am J Surg. 2016; 212:1101–1105.4. Brown JB, Sperry JL, Fombona A, Billiar TR, Peitzman AB, Guyette FX. Pre-trauma center red blood cell transfusion is associated with improved early outcomes in air medical trauma patients. J Am Coll Surg. 2015; 220:797–808.5. Schwab CW, Shayne JP, Turner J. Immediate trauma resuscitation with type O uncrossmatched blood: a two-year prospective experience. J Trauma. 1986; 26:897–902.6. Dutton RP, Shih D, Edelman BB, Hess J, Scalea TM. Safety of uncrossmatched type-O red cells for resuscitation from hemorrhagic shock. J Trauma. 2005; 59:1445–1449.7. Auten JD, Lunceford NL, Horton JL, Galarneau MR, Galindo RM, Shepps CD, Zieber TJ, Dewing CB. The safety of early fresh, whole blood transfusion among severely battle injured at US Marine Corps forward surgical care facilities in Afghanistan. J Trauma Acute Care Surg. 2015; 79:790–796.8. Kang BH, Jung KW, Heo YJ, Lee CJ. Safety and efficacy of type-O packed red blood cell transfusion in traumatic hemorrhagic shock patients: preliminary study. J Acute Care Surg. 2017; 7:50–55.9. Korea Centers for Disease Control and Prevention. Transfusion. 2nd rev. ed. [Internet]. accessed on 6 June 2017. Available at http://www.cdc.go.kr/CDC/contents/CdcKrContentLink.jsp?fid=51&cid=24064&ctype=1.10. ATLS Subcommittee. American College of Surgeons' Committee on Trauma. International ATLS working group. Advanced trauma life support (ATLS®): the ninth edition. J Trauma Acute Care Surg. 2013; 74:1363–1366.11. Powell EK, Hinckley WR, Gottula A, Hart KW, Lindsell CJ, McMullan JT. Shorter times to packed red blood cell transfusion are associated with decreased risk of death in traumatically injured patients. J Trauma Acute Care Surg. 2016; 81:458–462.12. Brown JB, Cohen MJ, Minei JP, Maier RV, West MA, Billiar TR, Peitzman AB, Moore EE, Cuschieri J, Sperry JL, et al. Pretrauma center red blood cell transfusion is associated with reduced mortality and coagulopathy in severely injured patients with blunt trauma. Ann Surg. 2015; 261:997–1005.13. Lee JH, Choa M, Cho J, Chung SP. Validity of transfusing group O+ unmatched packed red blood cells in hemorrhagic shock patients. J Korean Soc Traumatol. 2009; 22:167–171.14. Holcomb JB, Swartz MD, DeSantis SM, Greene TJ, Fox EE, Stein DM, Bulger EM, Kerby JD, Goodman M, Schreiber MA, et al. Multicenter observational prehospital resuscitation on helicopter study. J Trauma Acute Care Surg. 2017; 83:S83–S91.15. Smith IM, James RH, Dretzke J, Midwinter MJ. Prehospital blood product resuscitation for trauma: a systematic review. Shock. 2016; 46:3–16.16. Blumberg N. ABO mismatched platelet transfusions in trauma patients. CMAJ. 2014; 186:63.17. Hagiwara A, Kushimoto S, Kato H, Sasaki J, Ogura H, Matsuoka T, Uejima T, Hayakawa M, Takeda M, Kaneko N, et al. Can early aggressive administration of fresh frozen plasma improve outcomes in patients with severe blunt trauma?--a report by the Japanese Association for the Surgery of Trauma. Shock. 2016; 45:495–501.18. Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, del Junco DJ, Brasel KJ, Bulger EM, Callcut RA, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015; 313:471–482.19. Holcomb JB, Fox EE, Wade CE; PROMMTT Study Group. The PRospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study. J Trauma Acute Care Surg. 2013; 75:S1–S2.20. Kim Y, Lee K, Kim J, Kim J, Heo Y, Wang H, Lee K, Jung K. Application of damage control resuscitation strategies to patients with severe traumatic hemorrhage: review of plasma to packed red blood cell ratios at a single institution. J Korean Med Sci. 2014; 29:1007–1011.21. Yazer MH, Jackson B, Sperry JL, Alarcon L, Triulzi DJ, Murdock AD. Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. J Trauma Acute Care Surg. 2016; 81:21–26.22. Delaney M, Wendel S, Bercovitz RS, Cid J, Cohn C, Dunbar NM, Apelseth TO, Popovsky M, Stanworth SJ, Tinmouth A, et al. Transfusion reactions: prevention, diagnosis, and treatment. Lancet. 2016; 388:2825–2836.23. Branch DR. Anti-A and anti-B: what are they and where do they come from? Transfusion. 2015; 55:Suppl 2. S74–S79.24. Mulay SB, Jaben EA, Johnson P, Badjie K, Stubbs JR. Risks and adverse outcomes associated with emergency-release red blood cell transfusion. Transfusion. 2013; 53:1416–1420.25. Goodell PP, Uhl L, Mohammed M, Powers AA. Risk of hemolytic transfusion reactions following emergency-release RBC transfusion. Am J Clin Pathol. 2010; 134:202–206.26. Korean Red Cross. Title [Internet]. accessed on 6 June 2017. Available at http://www.bloodinfo.net/bloodknowledge_bloodtype.do.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and Efficacy of Type-O Packed Red Blood Cell Transfusion in Traumatic H emorrhagic Shock P atients: Preliminary Study
- Validity of Transfusing Group O+ Unmatched Packed Red Blood Cells in Hemorrhagic Shock Patients
- Transfusion-Related Acute Lung Injury after Stored Packed Red Blood Cell Transfusion: A Case Report
- Anesthetic Experience of Hemorrhagic Shock Patient with Rh-O Blood Type
- A Case of Packed red Cell Transfusion-Associated Anti-K Antibody