J Korean Med Sci.
2017 Dec;32(12):2042-2050. 10.3346/jkms.2017.32.12.2042.
Poisoning-induced Out-of-Hospital Cardiac Arrest and Outcomes according to Poison Agent
- Affiliations
-
- 1Department of Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea. sdshin@snu.ac.kr
- 3Department of Preventive Medicine, Seoul National University Graduate School of Public Health, Seoul, Korea.
- KMID: 2396384
- DOI: http://doi.org/10.3346/jkms.2017.32.12.2042
Abstract
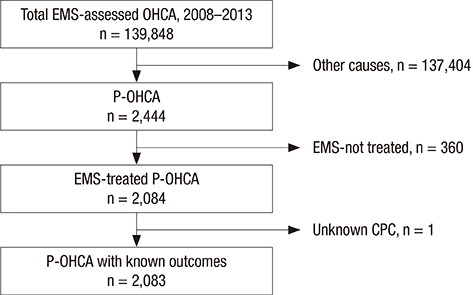
- It is unclear whether specific agent groups are associated with outcomes in cases of poisoning-induced out-of-hospital cardiac arrest (P-OHCA). The study population comprised cases of confirmed P-OHCA drawn from the national out-of-hospital cardiac arrest (OHCA) registry (2008-2013). Exposures were categorized into five groups according to the International Classification of Disease, 10th version: group 1, prescribed drugs; group 2, vapors and gases; group 3, pesticides; group 4, alcohol and organic solvents; and group 5, other poisons. The outcome was survival to discharge and good neurological recovery. Adjusted odds ratios (aORs) and 95% confidence intervals (CIs) were calculated to test the association between specific groups and outcomes. A total of 2,083 patients were analyzed; group 1 (10.3%), group 2 (23.6%), group 3 (52.9%), group 4 (1.4%), and group 5 (13.2%). The survival to discharge and good neurological recovery rates were 3.3%/1.3% for all patients, 10.3%/5.6% (group 1), 6.9%/3.4% (group 2), 2.4%/0.4% (group 3), 2.2%/1.0% (group 4), and 3.3%/2.4% (group 5) (all P < 0.001). The aORs (95% CIs) of groups 2-5 compared with group 1 for survival to discharge were 0.47 (0.09-2.51), 0.34 (0.17-0.68), 0.33 (0.14-0.77), and 0.31 (0.13-0.77), respectively. The odds ratios (95% CIs) for good neurological recovery were significant only in group 1, the pesticides group (0.07 [0.02-0.26]) and were not significant in the other groups. P-OHCA outcomes differed significantly among the poisoning agent groups. The pesticides group showed the worst outcomes, followed by the group of vapors or gases.
Keyword
MeSH Terms
Figure
Reference
-
1. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010; 81:1479–1487.2. Kitamura T, Kiyohara K, Sakai T, Iwami T, Nishiyama C, Kajino K, Nishiuchi T, Hayashi Y, Katayama Y, Yoshiya K, et al. Epidemiology and outcome of adult out-of-hospital cardiac arrest of non-cardiac origin in Osaka: a population-based study. BMJ Open. 2014; 4:e006462.3. Ro YS, Shin SD, Song KJ, Park CB, Lee EJ, Ahn KO, Cho SI. A comparison of outcomes of out-of-hospital cardiac arrest with non-cardiac etiology between emergency departments with low- and high-resuscitation case volume. Resuscitation. 2012; 83:855–861.4. Salcido DD, Torres C, Koller AC, Orkin AM, Schmicker RH, Morrison LJ, Nichol G, Stephens S, Menegazzi JJ. Resuscitation Outcomes Consortium Investigators. Regional incidence and outcome of out-of-hospital cardiac arrest associated with overdose. Resuscitation. 2016; 99:13–19.5. Ro YS, Shin SD, Song KJ, Lee EJ, Kim JY, Ahn KO, Chung SP, Kim YT, Hong SO, Choi JA, et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: a nationwide observational study from 2006 to 2010 in South Korea. Resuscitation. 2013; 84:547–557.6. Pell JP, Sirel JM, Marsden AK, Ford I, Walker NL, Cobbe SM. Presentation, management, and outcome of out of hospital cardiopulmonary arrest: comparison by underlying aetiology. Heart. 2003; 89:839–842.7. Hess EP, Campbell RL, White RD. Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2007; 72:200–206.8. Nielsen N, Hovdenes J, Nilsson F, Rubertsson S, Stammet P, Sunde K, Valsson F, Wanscher M, Friberg H. Hypothermia Network. Outcome, timing and adverse events in therapeutic hypothermia after out-of-hospital cardiac arrest. Acta Anaesthesiol Scand. 2009; 53:926–934.9. Bebarta VS, Pitotti RL, Borys DJ, Morgan DL. Seven years of cyanide ingestions in the USA: critically ill patients are common, but antidote use is not. Emerg Med J. 2011; 28:155–158.10. Park JH, Shin SD, Song KJ, Park CB, Ro YS, Kwak YH. Epidemiology and outcomes of poisoning-induced out-of-hospital cardiac arrest. Resuscitation. 2012; 83:51–57.11. Sohn CH, Ryoo SM, Lim KS, Kim W, Lim H, Oh BJ. Kind and estimated stocking amount of antidotes for initial treatment for acute poisoning at emergency medical centers in Korea. J Korean Med Sci. 2014; 29:1562–1571.12. Goel A, Aggarwal P. Pesticide poisoning. Natl Med J India. 2007; 20:182–191.13. Moulaert VR, Verbunt JA, van Heugten CM, Wade DT. Cognitive impairments in survivors of out-of-hospital cardiac arrest: a systematic review. Resuscitation. 2009; 80:297–305.14. Shin SD, Kitamura T, Hwang SS, Kajino K, Song KJ, Ro YS, Nishiuchi T, Iwami T. Seoul–Osaka Resuscitation Study (SORS) Group. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014; 85:203–210.15. Ahn KO, Shin SD, Suh GJ, Cha WC, Song KJ, Kim SJ, Lee EJ, Ong ME. Epidemiology and outcomes from non-traumatic out-of-hospital cardiac arrest in Korea: a nationwide observational study. Resuscitation. 2010; 81:974–981.16. Lin CH, Ng YY, Chiang WC, Karim SA, Shin SD, Tanaka H, Nishiuchi T, Kajino K, Khunkhlai N, Ma MH, et al. Variation of current protocols for managing out-of-hospital cardiac arrest in prehospital settings among Asian countries. J Formos Med Assoc. 2016; 115:628–638.17. Choi SW, Shin SD, Ro YS, Song KJ, Lee EJ, Ahn KO. Effect of therapeutic hypothermia on the outcomes after out-of-hospital cardiac arrest according to initial ECG rhythm and witnessed status: a nationwide observational interaction analysis. Resuscitation. 2016; 100:51–59.18. Kim JY, Shin SD, Ro YS, Song KJ, Lee EJ, Park CB, Hwang SS. CardioVascular Disease Surveillance (CAVAS) investigators. Post-resuscitation care and outcomes of out-of-hospital cardiac arrest: a nationwide propensity score-matching analysis. Resuscitation. 2013; 84:1068–1077.19. Shin SD, Suh GJ, Rhee JE, Sung J, Kim J. Epidemiologic characteristics of death by poisoning in 1991–2001 in Korea. J Korean Med Sci. 2004; 19:186–194.20. Lee WJ, Cha ES, Park ES, Kong KA, Yi JH, Son M. Deaths from pesticide poisoning in South Korea: trends over 10 years. Int Arch Occup Environ Health. 2009; 82:365–371.21. Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief. 2011; 1–8.22. Ossiander EM. Using textual cause-of-death data to study drug poisoning deaths. Am J Epidemiol. 2014; 179:884–894.23. Dines AM, Wood DM, Yates C, Heyerdahl F, Hovda KE, Giraudon I, Sedefov R, Dargan PI. Euro-DEN Research Group. Acute recreational drug and new psychoactive substance toxicity in Europe: 12 months data collection from the European Drug Emergencies Network (Euro-DEN). Clin Toxicol (Phila). 2015; 53:893–900.24. von Mach MA, Brinkmann X, Weilemann LS. Epidemiology of cardiac dysrhythmias in acute intoxication. Z Kardiol. 2004; 93:Suppl 4. IV9–IV15.25. Maskell KF, Ferguson NM, Bain J, Wills BK. Survival after cardiac arrest: ECMO rescue therapy after amlodipine and metoprolol overdose. Cardiovasc Toxicol. 2017; 17:223–225.26. Reynolds JC, Judge BS. Successful treatment of flecainide-induced cardiac arrest with extracorporeal membrane oxygenation in the ED. Am J Emerg Med. 2015; 33:1542.27. Thooft A, Goubella A, Fagnoul D, Taccone FS, Brimioulle S, Vincent JL, De Backer D. Combination of veno-arterial extracorporeal membrane oxygenation and hypothermia for out-of-hospital cardiac arrest due to Taxus intoxication. CJEM. 2014; 16:504–507.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic factors related with outcomes in out-of-hospital cardiac arrest due to pesticide poisoning in South Korea: a nationwide population-based study
- A Case Report of Cardiac Arrest Following Intentional Ingestion of Liquid Nicotine for Electronic Cigarette
- Case of cardiac arrest due to carbon dioxide poisoning following an explosion of a carbon dioxide tank
- Different Characteristics of Toxic Substance/poison Exposure Data that Collected from Pre-hospital Telephone Response and Emergency Department
- Acute Nicotine Poisoning due to Electronic Cigarette Liquid: Systematic Review of Case Reports