J Korean Med Sci.
2017 Dec;32(12):1938-1946. 10.3346/jkms.2017.32.12.1938.
Adapter-based Safety Injection System for Prevention of Wrong Route and Wrong Patient Medication Errors
- Affiliations
-
- 1Interdisciplinary Program in Bioengineering, Seoul National University College of Engineering, Seoul, Korea. ybchoy@snu.ac.kr
- 2Institute of Medical & Biological Engineering, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Biomedical Engineering, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2396369
- DOI: http://doi.org/10.3346/jkms.2017.32.12.1938
Abstract
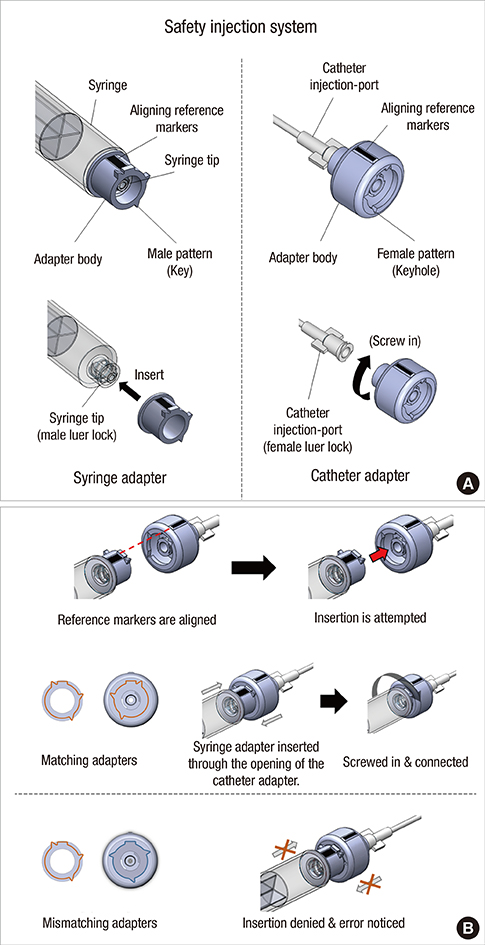
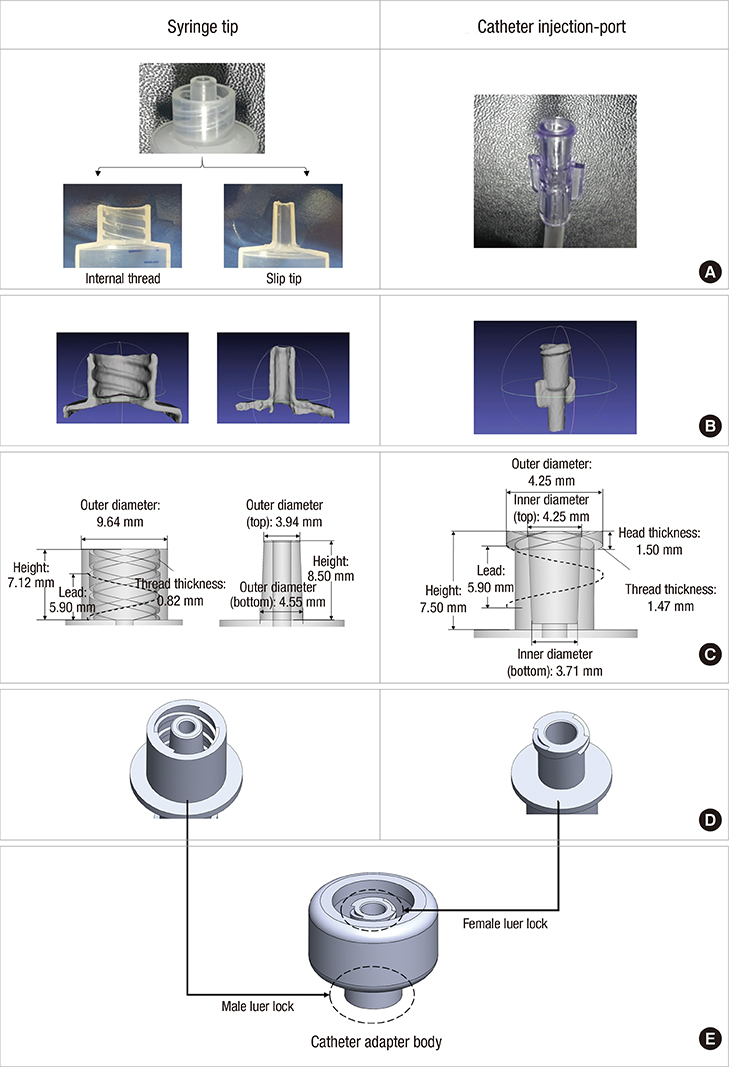
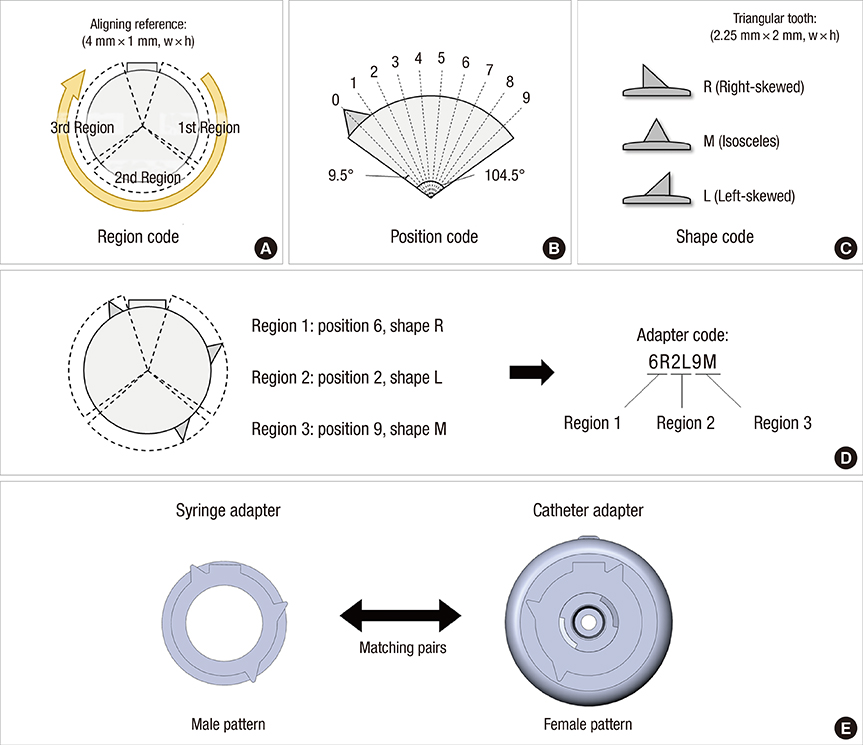
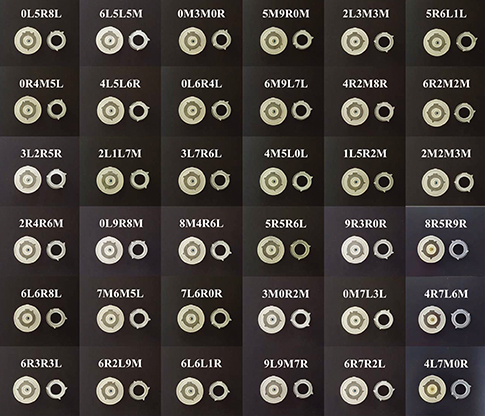
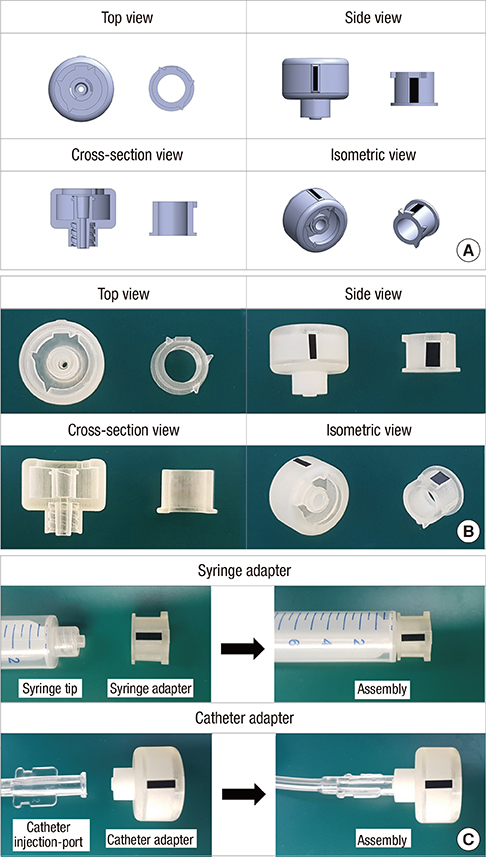
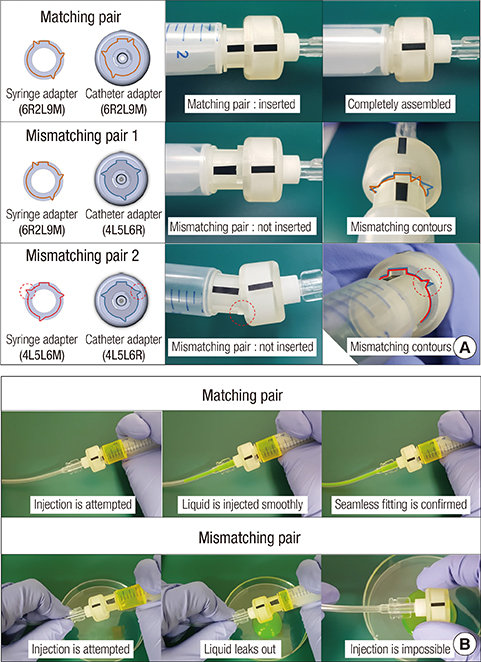
- Wrong-route or -patient medication errors due to human mistakes have been considered difficult to resolve in clinical settings. In this study, we suggest a safety injection system that can help to prevent an injection when a mismatch exists between the drug and route or patient. For this, we prepared two distinct adapters with key and keyhole patterns specifically assigned to a pair of drug and route or patient. When connected to a syringe tip and its counterpart, a catheter injection-port, respectively, the adapters allowed for a seamless connection only with their matching patterns. In this study, each of the adapters possessed a specific key and keyhole pattern at one end and the other end was shaped to be a universal fit for syringe tips or catheter injection-ports in clinical use. With the scheme proposed herein, we could generate 27,000 patterns, depending on the location and shape of the key tooth in the adapters. With a rapid prototyping technique, multiple distinct pairs of adapters could be prepared in a relatively short period of time and thus, we envision that a specific adapter pair can be produced on-site after patient hospitalization, much like patient identification barcodes.
Keyword
Figure
Reference
-
1. Westbrook JI, Rob MI, Woods A, Parry D. Errors in the administration of intravenous medications in hospital and the role of correct procedures and nurse experience. BMJ Qual Saf. 2011; 20:1027–1034.2. Elliott M, Liu Y. The nine rights of medication administration: an overview. Br J Nurs. 2010; 19:300–305.3. Pham JC, Story JL, Hicks RW, Shore AD, Morlock LL, Cheung DS, Kelen GD, Pronovost PJ. National study on the frequency, types, causes, and consequences of voluntarily reported emergency department medication errors. J Emerg Med. 2011; 40:485–492.4. Teixeira TC, de Cassiani SH. Root cause analysis: evaluation of medication errors at a university hospital. Rev Esc Enferm USP. 2010; 44:139–146.5. Cho WS. A study on the types and causes of medication errors and related drugs-by analyzing AJNs medication error 73 cases. J Korea Community Health Nurs Acad Soc. 2002; 16:176–189.6. Fathi A, Hajizadeh M, Moradi K, Zandian H, Dezhkameh M, Kazemzadeh S, Rezaei S. Medication errors among nurses in teaching hospitals in the west of Iran: what we need to know about prevalence, types, and barriers to reporting. Epidemiol Health. 2017; 39:e2017022.7. Phillips J, Beam S, Brinker A, Holquist C, Honig P, Lee LY, Pamer C. Retrospective analysis of mortalities associated with medication errors. Am J Health Syst Pharm. 2001; 58:1835–1841.8. Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, Goldmann DA. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001; 285:2114–2120.9. Prot S, Fontan JE, Alberti C, Bourdon O, Farnoux C, Macher MA, Foureau A, Faye A, Beaufils F, Gottot S, et al. Drug administration errors and their determinants in pediatric in-patients. Int J Qual Health Care. 2005; 17:381–389.10. Grissinger M. Reducing the risk of deadly mixups with epidural and intravenous drugs. P T. 2012; 37:432.11. Linden JV, Wagner K, Voytovich AE, Sheehan J. Transfusion errors in New York State: an analysis of 10 years' experience. Transfusion. 2000; 40:1207–1213.12. National Health Service (GB). Never Events List 2015/16. London: NHS England;2015.13. Pongudom S, Chinthammitr Y. Inadvertent intrathecal vincristine administration: report of a fatal case despite cerebrospinal fluid lavage and a review of the literature. J Med Assoc Thai. 2011; 94:Suppl 1. S258–S263.14. Reddy GK, Brown B, Nanda A. Fatal consequences of a simple mistake: how can a patient be saved from inadvertent intrathecal vincristine? Clin Neurol Neurosurg. 2011; 113:68–71.15. Garrouste-Orgeas M, Philippart F, Bruel C, Max A, Lau N, Misset B. Overview of medical errors and adverse events. Ann Intensive Care. 2012; 2:2.16. Kim M, Jeong S, Choi E, Ha H, Lee HY. Death after accidental injection of tranexamic acid during spinal anesthesia. Korean J Leg Med. 2009; 33:139–142.17. Glavin RJ. Drug errors: consequences, mechanisms, and avoidance. Br J Anaesth. 2010; 105:76–82.18. Yang A, Grissinger M. Wrong-patient medication errors: an analysis of event reports in Pennsylvania and strategies for prevention. Pa Patient Saf Advis. 2013; 10:41–49.19. Bauters T, De Porre J, Janssens N, Van de Velde V, Verlooy J, Dhooge C, Robays H. Prevention of wrong route errors in a pediatric hemato-oncology ward. Pharm World Sci. 2009; 31:522–524.20. Koppel R, Wetterneck T, Telles JL, Karsh BT. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc. 2008; 15:408–423.21. Henneman PL, Marquard JL, Fisher DL, Bleil J, Walsh B, Henneman JP, Blank FS, Higgins AM, Nathanson BH, Henneman EA. Bar-code verification: reducing but not eliminating medication errors. J Nurs Adm. 2012; 42:562–566.22. Choi JS, Kim D. Technical considerations for successful implementation of a barcode-based medication system in hospital. J Korean Soc Med Inform. 2009; 15:303–312.23. Choonara YE, du Toit LC, Kumar P, Kondiah PP, Pillay V. 3D-printing and the effect on medical costs: a new era? Expert Rev Pharmacoecon Outcomes Res. 2016; 16:23–32.24. Ihl C, Piller F. 3D printing as driver of localized manufacturing: expected benefits from producer and consumer perspectives. In : Ferdinand JP, Petschow U, Dickel S, editors. The Decentralized and Networked Future of Value Creation. Cham: Springer;2016. p. 179–204.25. Wong KV, Hernandez A. A review of additive manufacturing. ISRN Mech Eng. 2012; 2012:208760.26. Sastri VR. Plastics in Medical Devices: Properties, Requirements, and Applications. Amsterdam: Elsevier/William Andrew;2014.27. United States Pharmacopeial Convention. United States Pharmacopeia. 23 - National Formulary 18. Rockville, MD: United States Pharmacopeial Convention;1994.28. Macdonald NP, Zhu F, Hall CJ, Reboud J, Crosier PS, Patton EE, Wlodkowic D, Cooper JM. Assessment of biocompatibility of 3D printed photopolymers using zebrafish embryo toxicity assays. Lab Chip. 2016; 16:291–297.29. Onia R, Wu Y, Parvu V, Eshun-Wilson I, Kassler-Taub K. Simulated evaluation of a non-Luer safety connector system for use in neuraxial procedures. Br J Anaesth. 2012; 108:134–139.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention of wrong site, wrong procedure, wrong patient surgery and time-out
- Perception and Experience of Medication Errors in Nurses with Less than One Year Job Experience
- Patient Safety in Spine Surgery: Regarding the Wrong-Site Surgery
- Patient safety management in the medication use process: prevention and management of medication error
- Analysis of Medication Errors of Nurses by Patient Safety Accident Reports