An Acute Medical Unit in a Korean Tertiary Care Hospital Reduces the Length of Stay and Waiting Time in the Emergency Department
- Affiliations
-
- 1Division of General Internal Medicine, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Hospital Medicine Center, Seoul National University Bundang Hospital, Seongnam, Korea. janghak@snu.ac.kr
- 3Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2396366
- DOI: http://doi.org/10.3346/jkms.2017.32.12.1917
Abstract
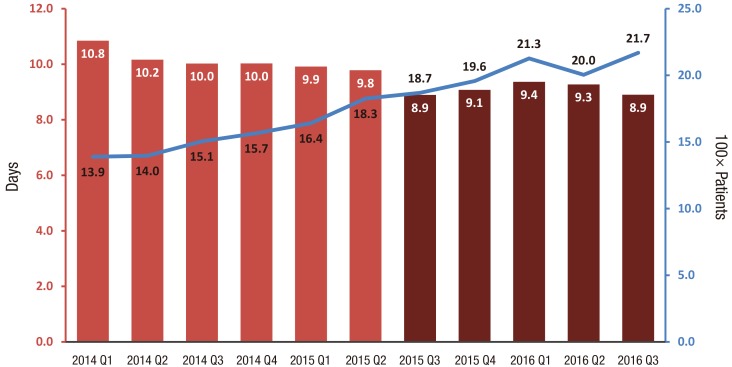
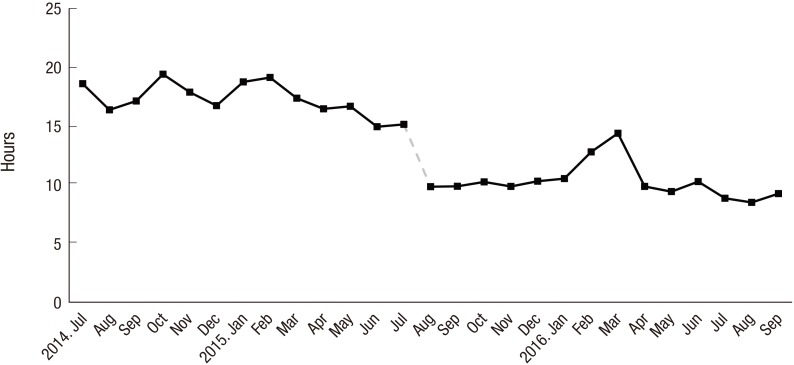
- A hospitalist-run acute medical unit (AMU) opened at a tertiary care hospital on August 2015 for the first time in Korea. Patients visiting the emergency department (ED) with acute medical problems are admitted to the AMU. They stay in that unit for less than 72 hours and are discharged or transferred to specialty wards if longer treatment is necessary. We reviewed 19,450 medical admissions through the ED from January 2014 to September 2016. The median length of stay (LOS) significantly decreased from 10.0 days (interquartile range [IQR], 5.5-16.7) to 9.1 days (IQR, 5.1-15.0) (P < 0.001) after the establishment of the AMU. The median waiting time in the ED significantly shortened by 40% (P < 0.001). Future studies on the impact of AMU on in-patient morbidity, mortality, re-admission rate, and patient or staff satisfaction are necessary.
MeSH Terms
Figure
Cited by 4 articles
-
Comparisons of Clinical Outcomes between Weekday-Only and Full-Time, 24-Hour/7-Day Coverage Hospitalist Systems
Seung Jun Han, Hee-Won Jung, Do-Youn Oh, Jae Hyun Lee, Sung do Moon, Sunhye Lee, Jung-Hwan Yoon
J Korean Med Sci. 2020;35(18):e117. doi: 10.3346/jkms.2020.35.e117.Evaluating the Outcome of Multi-Morbid Patients Cared for by Hospitalists: a Report of Integrated Medical Model in Korea
Jung Hwan Lee, Ah Jin Kim, Tae Young Kyong, Ji-Hun Jang, Jeongmi Park, Jeong Hoon Lee, Man-Jong Lee, Jung-Soo Kim, Young Ju Suh, Seong-Ryul Kwon, Cheol-Woo Kim
J Korean Med Sci. 2019;34(25):. doi: 10.3346/jkms.2019.34.e179.The Impact of Hospitalist Care in Korea
Junhwan Kim
J Korean Med Sci. 2019;34(25):. doi: 10.3346/jkms.2019.34.e177.Current status and future of internal medicine hospitalist in Korea
Junhwan Kim
J Korean Med Assoc. 2019;62(11):564-568. doi: 10.5124/jkma.2019.62.11.564.
Reference
-
1. Eom JS. Operating the hospitalist system. J Korean Med Assoc. 2016; 59:342–344.2. Jang SI, Jang SY, Park EC. Trends of US hospitalist and suggestions for introduction of Korean hospitalist. Korean J Med. 2015; 89:1–5.3. Lee DK. Launching the hospitalist in Korea. Korean J Med. 2016; 91:241–244.4. Wachter RM, Goldman L. Zero to 50,000 - the 20th anniversary of the hospitalist. N Engl J Med. 2016; 375:1009–1011. PMID: 27508924.5. Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996; 335:514–517. PMID: 8672160.6. Wachter RM, Katz P, Showstack J, Bindman AB, Goldman L. Reorganizing an academic medical service: impact on cost, quality, patient satisfaction, and education. JAMA. 1998; 279:1560–1565. PMID: 9605901.7. Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002; 137:859–865. PMID: 12458985.8. Bell D, Skene H, Jones M, Vaughan L. A guide to the acute medical unit. Br J Hosp Med (Lond). 2008; 69:M107–M109. PMID: 18833973.9. Jones MC, Bell D. What is acute medicine and do we need it? Br J Hosp Med (Lond). 2009; 70:S8–S10. PMID: 19522113.10. Ward D, Potter J, Ingham J, Percival F, Bell D. Acute medical care. The right person, in the right setting--first time: how does practice match the report recommendations? Clin Med (Lond). 2009; 9:553–556. PMID: 20095297.11. Wachter RM, Bell D. Renaissance of hospital generalists. BMJ. 2012; 344:e652. PMID: 22331278.12. Moloney ED, Smith D, Bennett K, O’Riordan D, Silke B. Impact of an acute medical admission unit on length of hospital stay, and emergency department ‘wait times’. QJM. 2005; 98:283–289. PMID: 15760924.13. Moloney ED, Bennett K, Silke B. Effect of an acute medical admission unit on key quality indicators assessed by funnel plots. Postgrad Med J. 2007; 83:659–663. PMID: 17916876.14. Rooney T, Moloney ED, Bennett K, O'Riordan D, Silke B. Impact of an acute medical admission unit on hospital mortality: a 5-year prospective study. QJM. 2008; 101:457–465. PMID: 18319292.15. Byrne D, Silke B. Acute medical units: review of evidence. Eur J Intern Med. 2011; 22:344–347. PMID: 21767750.16. Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care. 2009; 21:397–407. PMID: 19903756.17. St Noble VJ, Davies G, Bell D. Improving continuity of care in an acute medical unit: initial outcomes. QJM. 2008; 101:529–533. PMID: 18417499.18. McLaren EH, Summerhill LE, Miller WJ, McMurdo ML, Robb CM. Re-organising emergency medical admitting: the Stobhill experience, 1992–1997. Health Bull (Edinb). 1999; 57:108–117. PMID: 12811902.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Admission Time to the Medical Intensive Care Unit on Acute Critical Patient Outcomes
- Effect of Issuing of Hospitalization Sheets by Emergency Department on Shortening Length of Stay
- The Effectiveness of Fast Track for Minor Patients in the Emergency Department
- Effect of trauma center operation on emergency care and clinical outcomes in patients with traumatic brain injury
- The effect of COVID-19 pandemic on the length of stay and outcomes in the emergency department