J Korean Ophthalmol Soc.
2017 Nov;58(11):1289-1294. 10.3341/jkos.2017.58.11.1289.
Delayed Onset Purtscher's Retinopathy with Serous Retinal Detachment after Trauma in a Retinitis Pigmentosa
- Affiliations
-
- 1Department of Ophthalmology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea. kimdk89@empas.com
- KMID: 2395872
- DOI: http://doi.org/10.3341/jkos.2017.58.11.1289
Abstract
- PURPOSE
To report a case of Purtscher's retinopathy accompanied by serous retinal detachment in a patient with retinitis pigmentosa (RP) who was referred to us for treatment of post-traumatic visual discomfort.
CASE SUMMARY
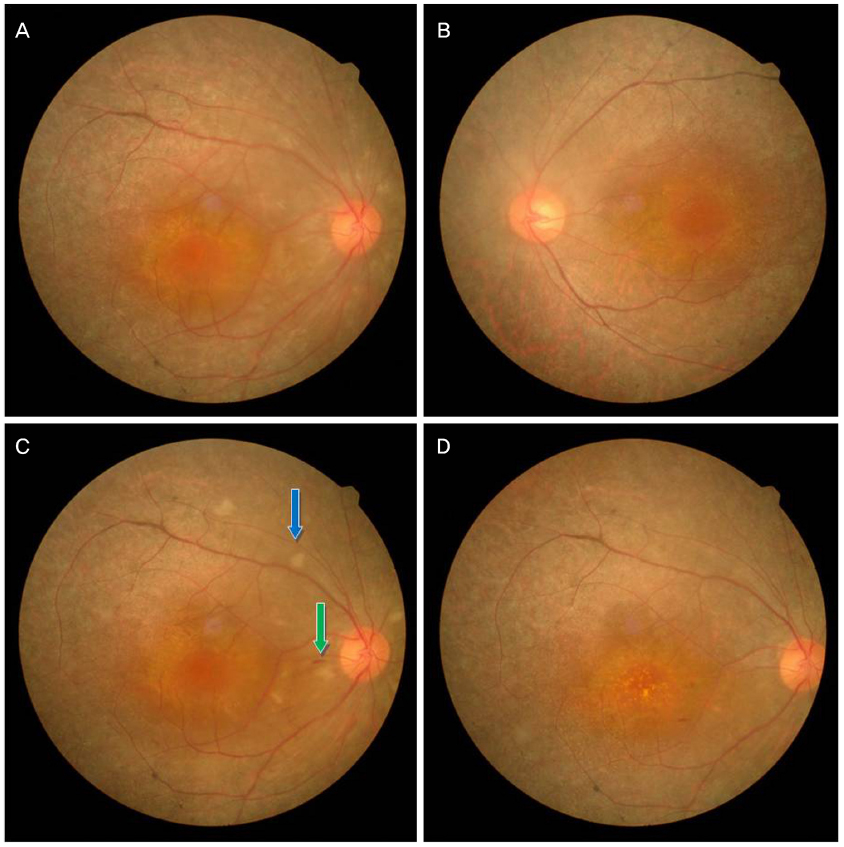
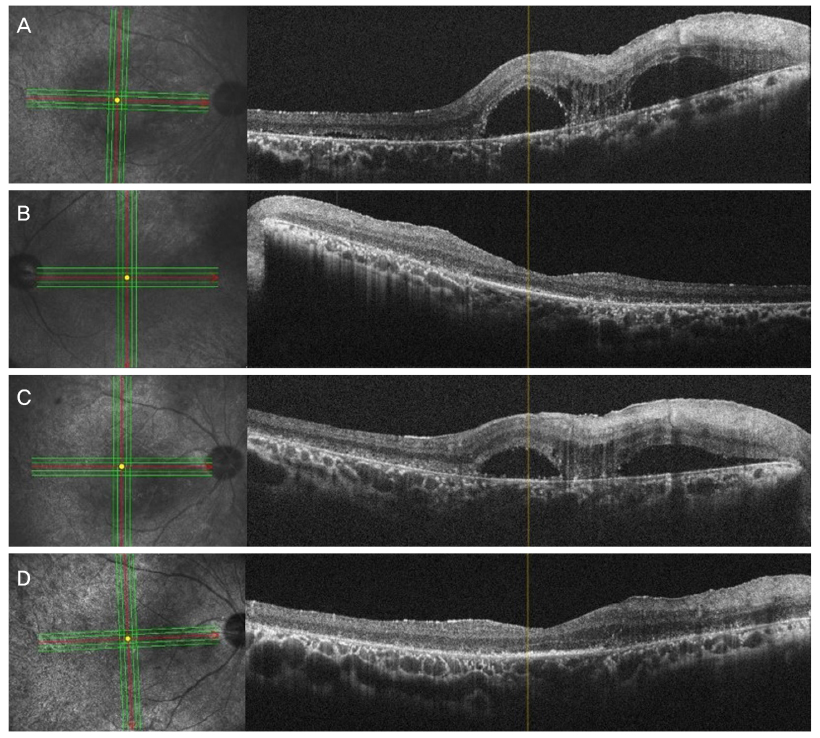
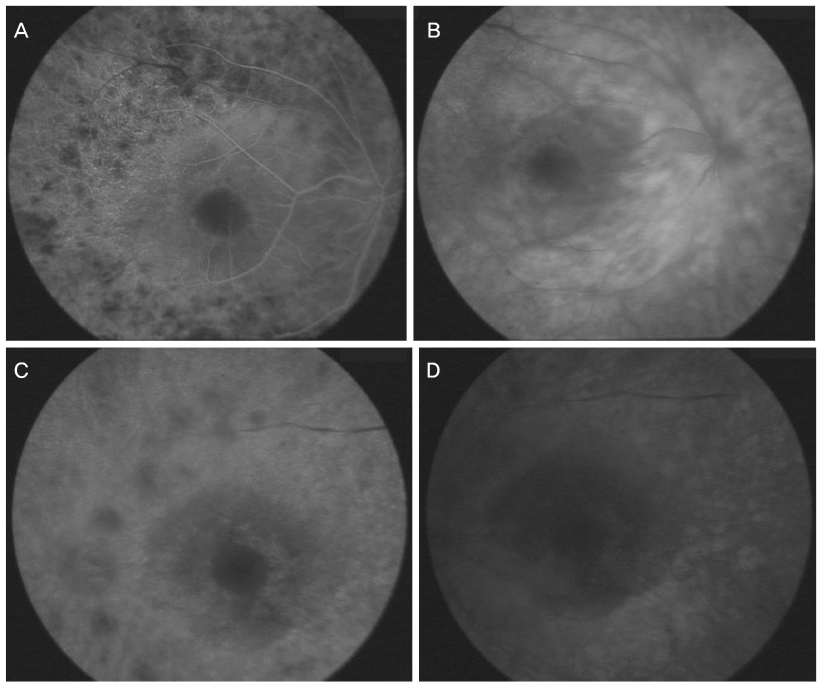
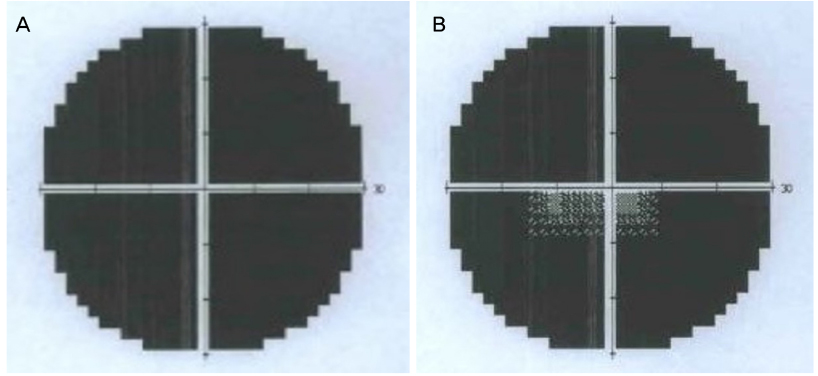
A 36-year-old man with history of RP was referred to us with the chief complaint of bilateral visual discomfort after chest injury from a traffic accident. His corrected visual acuity was 0.3 and 0.6 in the right and left eyes, respectively. Fundus examination revealed findings characteristic of RP in both eyes, along with a lesion in the right eye, which was suspected to be a serous elevation of the macula, as well as suspected exudates near the optic nerves. Optical coherence tomography indicated serous retinal detachment in the right eye, and fluorescein angiography findings were characteristic of RP. Seven days later, the amount of cotton-wool exudate in the right eye had increased and was more distinct than at the initial examination, and retinal hemorrhage was observed. Based on the medical history and specific fundus findings, the patient was diagnosed with Purtscher's retinopathy. One month later, the serous retinal detachment in the right eye had improved, but the vision loss and total anopsia in the right eye persisted.
CONCLUSIONS
The concomitant occurrence of RP and Purtscher's retinopathy is very rare. Moreover, the presence of accompanying serous retinal detachment and delayed onset of typical clinical symptoms are not present in typical Purtscher's retinopathy.
MeSH Terms
Figure
Reference
-
1. Wong P, Borst DE, Farber D, et al. Increased TRPM-2/clusterin mRNA levels during the time of retinal degeneration in mouse models of retinitis pigmentosa. Biochem Cell Biol. 1994; 72:439–446.2. Cotran PR, Bruns GA, Berson EL, Dryja TP. Genetic analysis of patients with retinitis pigmentosa using a cloned cDNA probe for the human gamma subunit of cyclic GMP phosphodiesterase. Exp Eye Res. 1991; 53:557–564.3. Rootman DB, Mandelcorn E, Dracopoulos A, et al. Concurrence of retinitis pigmentosa and central serous retinopathy. Digit J Ophthalmol. 2011; 17:55–57.4. Agrawal A, McKibbin MA. Purtscher's and Purtscher-like retinopathies: a review. Surv Ophthalmol. 2006; 51:129–136.5. Yamaguchi K, Kin-para Y, Tamai M. Idiopathic central serous choroidopathy in a patient with pericentral pigmentary retinal degeneration. Ann Ophthalmol. 1991; 23:251–253.6. Meunier I, Ben Salah S, Arndt C, Hamel C. Retinitis pigmentosa and central serous choroiditis. Retinal imaging and optical coherence tomography views. J Fr Ophtalmol. 2008; 31:735.7. Lewis ML. Coexisting central serous choroidopathy and retinitis pigmentosa. South Med J. 1980; 73:77–80.8. Dorenboim Y, Rehany U, Rumelt S. Central serous chorioretinopathy associated with retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2004; 242:346–349.9. Behrens-Baumann W, Scheurer G, Schroer H. Pathogenesis of Purtscher's retinopathy. An experimental study. Graefes Arch Clin Exp Ophthalmol. 1992; 230:286–291.10. Burton TC. Unilateral Purtscher's retinopathy. Ophthalmology. 1980; 87:1096–1105.11. Jacob HS, Craddock PR, Hammerschmidt DE, Moldow CF. Complement-induced granulocyte aggregation: an unsuspected mechanism of disease. N Engl J Med. 1980; 302:789–794.12. Lai JC, Johnson MW, Martonyi CL, Till GO. Complement-induced retinal arteriolar occlusions in the cat. Retina. 1997; 17:239–246.13. Li ZY, Possin DE, Milam AH. Histopathology of bone spicule pigmentation in retinitis pigmentosa. Ophthalmology. 1995; 102:805–816.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Purtscher's Retinopathy with Diffuse Serous Macular Detachment
- Spontaneously Resolved Purtscher's Retinopathy within 24 Hours: Case Report and OCT Review
- Electrophysiologic Finding of Retinitis Pigmentosa Inversus and Differential Diagnosis from Peripapillary Choroidal Dystrophy
- Clinical Applications of Multifocal Electroretinography (mfERG)
- Strategies for Mutation Discovery in Retinitis Pigmentosa: Transition to the Next Generation