J Dent Rehabil Appl Sci.
2017 Sep;33(3):189-198. 10.14368/jdras.2017.33.3.189.
Stress distribution of implants with external and internal connection design: a 3-D finite element analysis
- Affiliations
-
- 1Department of Periodontology, School of Dentistry, Chonnam National University, Gwangju, Republic of Korea.
- 2Department of Bio and Brain Engineering, KAIST, Daejon, Republic of Korea.
- 3Department of Prosthodontics, School of Dentistry, Chonnam National University, Gwangju, Republic of Korea. yhsdent@jnu.ac.kr
- KMID: 2394642
- DOI: http://doi.org/10.14368/jdras.2017.33.3.189
Abstract
- PURPOSE
This study aims to analyze the stress distribution of mandibular molar restoration supported by the implants with external hex and internal taper abutment connection design.
MATERIALS AND METHODS
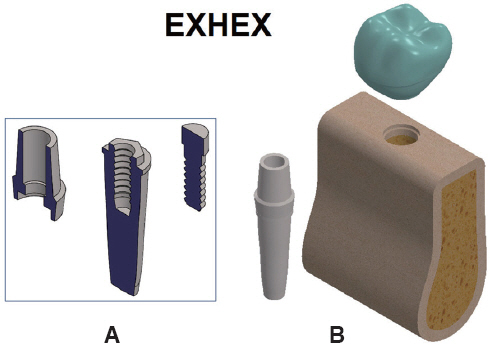
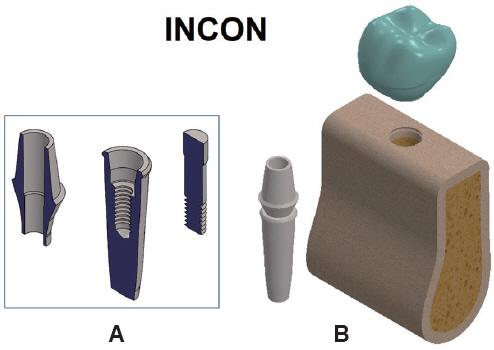
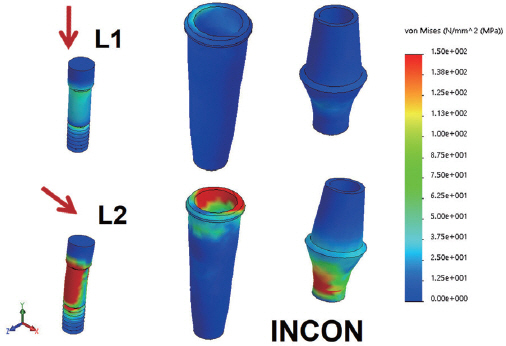
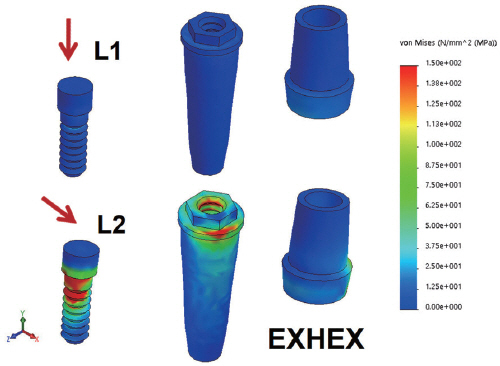
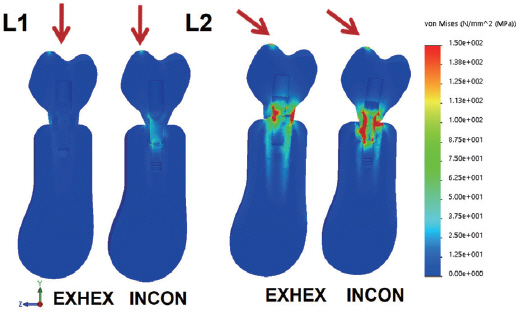
Models of external connection (EXHEX) and internal connection (INCON) implants, corresponding abutment/crowns, and screws were developed. Supporting edentulous mandibular bony structures were designed. All the components were assembled and a finite element analysis was performed to predict the magnitude and pattern of stresses generated by occlusal loading. A total of 120 N static force was applied both by axial (L1) and oblique (L2) direction.
RESULTS
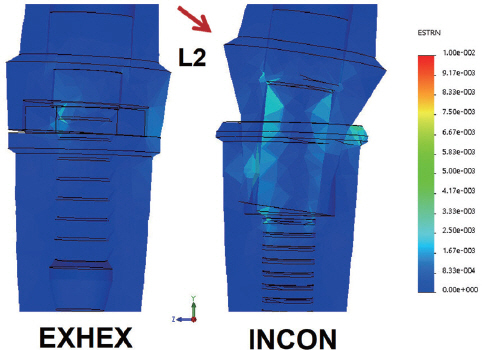
Peak von Mises stresses produced in the implants by L2 load produced 6 - 15 times greater than those by L1 load. The INCON model showed 2.2 times greater total amount of crown cusp deflection than the EXHEX model. Fastening screw in EXHEX model and upside margin of implant fixture in INCON model generated the peak von Mises stresses by oblique occlusal force. EXHEX model and INCON model showed the similar opening gap between abutment and fixture, but intimate sealing inside the contact interface was maintained in INCON model.
CONCLUSION
Oblique force produced grater magnitudes of deflection and stress than those by axial force. The maximum stress area at the implant was different between the INCON and EXHEX models.
Keyword
Figure
Reference
-
References
1. Eckert SE, Meraw SJ, Cal E, Ow RK. Analysis of incidence and associated factors with fractured implants: a retrospective study. Int J Oral Maxillofac Implants. 2000; 15:662–7. PMID: 11055133.2. Sánchez-Pérez A, Moya-Villaescusa MJ, Jornet-García A, Gomez S. Etiology, risk factors and management of implant fractures. Med Oral Patol Oral Cir Bucal. 2010; 15:e504–8. DOI: 10.4317/medoral.15.e504. PMID: 20038899.3. Eckert SE, Choi YG, Sánchez AR, Koka S. Complication of dental implant systems: quality of clinical evidence and prediction of 5-year survival. Int J Oral Maxillofac Implants. 2005; 20:406–15. PMID: 15973952.4. Norton MR. An in vitro evaluation of the strength of a 1-piece and 2- piece conical abutment joint in implant design. Clin Oral Implants Res. 2000; 11:458–64. DOI: 10.1034/j.1600-0501.2000.011005458.x. PMID: 11168238.5. Binon PP. Implants and components: entering the new millennium. Int J Oral Maxillofac Implants. 2000; 15:76–95. PMID: 10697942.6. Khraisat A, Stegaroiu R, Nomura S, Miyakawa O. Fatigue resistance of two implant/abutment joint designs. J Prosthet Dent. 2002; 88:604–10. DOI: 10.1067/mpr.2002.129384. PMID: 12488853.7. Çehreli MC, Akça K, Íplikçio lu H, Sahin S. Dynamic fatigue resistance of implant-abutment junction in an internally notched morse-taper oral implant: influence of abutment design. Clin Oral Implants Res. 2004; 15:459–65. DOI: 10.1111/j.1600-0501.2004.01023.x. PMID: 15248881.8. Dittmer S, Dittmer MP, Kohorst P, Jendras M, Borchers L, Stiesch M. Effect of implant-abutment connection design on load bearing capacity and failure mode of implants. J Prosthodont. 2011; 20:510–6. DOI: 10.1111/j.1532-849X.2011.00758.x. PMID: 21910778.9. Boggan RS, Strong JT, Misch CE, Bidez MW. Influence of hex geometry and prosthetic table width on static and fatigue strength of dental implants. J Prosthet Dent. 1999; 82:436–40. DOI: 10.1016/S0022-3913(99)70030-2.10. Steinebrunner L, Wolfart S, Ludwig K, Kern M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Implants Res. 2008; 19:1276–84. DOI: 10.1111/j.1600-0501.2008.01581.x. PMID: 19040443.11. Conrad HJ, Schulte JK, Vallee MC. Fractures related to occlusal overload with single posterior implants: a clinical report. J Prosthet Dent. 2008; 99:251–6. DOI: 10.1016/S0022-3913(08)00041-3.12. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003; 90:121–32. DOI: 10.1016/S0022-3913(03)00212-9.13. McDermott NE, Chuang SK, Woo VV, Dodson TB. Complications of dental implants: identification, frequency, and associated risk factors. Int J Oral Maxillofac Implants. 2003; 18:848–55. PMID: 14696660.14. Möllersten L, Lockowandt P, Lindén L. Comparison of strength and failure mode of seven implant systems: an in vitro test. J Prosthet Dent. 1997; 78:582–91. DOI: 10.1016/S0022-3913(97)70009-X.15. Djebbar N, Serier B, Bouiadjra BB, Benbarek S, Drai A. Analysis of the effect of load direction on the stress distribution in dental implant. Mater Des. 2010; 31:2097–101. DOI: 10.1016/j.matdes.2009.10.042.16. Sevimay M, Turhan F, Kiliçarslan MA, Eskitascioglu G. Three-dimensional finite element analysis of the effect of different bone quality on stress distribution in an implant-supported crown. J Prosthet Dent. 2005; 93:227–34. DOI: 10.1016/j.prosdent.2004.12.019. PMID: 15775923.17. Íplikçio lu H, Akça K. Comparative evaluation of the effect of diameter, length and number of implant supporting three-unit fixed partial prosthesis on stress distribution in the bone. J Dent. 2002; 30:41–6. DOI: 10.1016/S0300-5712(01)00057-4.18. Jörn D, Kohorst P, Besdo S, Rücker M, Stiesch M, Borchers L. Influence of lubricant on screw preload and stresses in a finite model for a dental implant. J Prosthet Dent. 2014; 112:340–8. DOI: 10.1016/j.prosdent.2013.10.016. PMID: 24529658.19. Eskitascioglu G, Usumez A, Sevimay M, Soykan E, Unsal E. The influence of occlusal loading location on stresses transferred to implant-supported prostheses and supporting bone: a three-dimensional finite element study. J Prosthet Dent. 2004; 91:144–50. DOI: 10.1016/j.prosdent.2003.10.018. PMID: 14970760.20. Freitas-Júnior AC, Rochac EP, Bonfante EA, Almeida EO, Anchieta RB, Martini AP, Assunção WG, Silva NR, Coelho PG. Biomechanical evaluation of internal and external hexagon platform switched implant-abutment connections: an in vitro laboratory and three-dimensional finite element analysis. Dent Mater. 2012; 28:e218–28. DOI: 10.1016/j.dental.2012.05.004. PMID: 22682782.21. Choi AH, Matinlinna JP, Ben-Nissan B. Finite element stress analysis of Ti-6Al-4V and partially stabilized zirconia dental implant during clenching. Acta Odontol Scand. 2012; 70:353–61. DOI: 10.3109/00016357.2011.600723. PMID: 21815837.22. Ma L, Guess PC, Zhang Y. Load-bearing properties of minimal-invasive monolithic lithium disilicate and zirconia occlusal onlays: finite element and theoretical analyses. Dent Mater. 2013; 29:742–51. DOI: 10.1016/j.dental.2013.04.004. PMID: 23683531. PMCID: PMC3698988.23. Pessoa RS, Muraru L, Marcantonio Júnior E, Vaz LG, Sloten JV, Duyck J, Jaecques SV. Influence of implant connection type on the biomechanical environment of immediately placed implants –CT-based nonlinear, three-dimensional finite element analysis. Clin Implant Dent Relat Res. 2010; 12:219–34. PMID: 19438946.24. Tang CB, Liu SY, Zhou GX, Yu JH, Zhang GD, Bao YD, Wang QJ. Nonlinear finite element analysis of three implant-abutment interface designs. Int J Oral Sci. 2012; 4:101–8. DOI: 10.1038/ijos.2012.35. PMID: 22699263. PMCID: PMC3412669.25. Yamanishi Y, Yamaguchi S, Imazato S, Nakano T, Yatani H. Influences of implant neck design and implant-abutment joint type on peri-implant bone stress and abutment micromovement: three-dimensional finite element analysis. Dent Mater. 2012; 28:1126–33. DOI: 10.1016/j.dental.2012.07.160. PMID: 22920538.26. Tsouknidas A, Lympoudi E, Michalakis K, Giannopoulos D, Michailidis N, Pissiotis A, Fytanidas D, Kugiumtzis D. Influence of alveolar bone loss and different alloys on the biomechanical behavior of internal- and external-connection implants: a three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2015; 30:e30–42. DOI: 10.11607/jomi.3814. PMID: 26009924.27. Ausiello P, Franciosa P, Martorelli M, Watts DC. Numerical fatigue 3D-FE modeling of indirect composite-restored posterior teeth. Dent Mater. 2011; 27:423–30. DOI: 10.1016/j.dental.2010.12.001. PMID: 21227484.28. Farah JW, Craig RG, Meroueh KA. Finite element analysis of three and four unit bridges. J Oral Rehabil. 1989; 16:603–11. DOI: 10.1111/j.1365-2842.1989.tb01384.x. PMID: 2689617.29. Schindler HJ, Stengel E, Spiess WE. Feedback control during mastication of solid food textures-a clinical-experimental study. J Prosthet Dent. 1998; 80:330–6. DOI: 10.1016/S0022-3913(98)70134-9.30. Richter EJ. In vivo vertical forces on implants. Int J Oral Maxillofac Implants. 1995; 10:99–108. PMID: 7615323.31. Rangert B, Jemt T, Jörneus L. Forces and moments on Brånemark implants. Int J Oral Maxillofac Implants. 1989; 4:241–7. PMID: 2700747.32. Steinebrunner L, Wolfart S, Bössmann K, Kern M. In vitro evaluation of bacterial leakage along the implant-abutment interface of different implant systems. Int J Oral Maxillofac Implants. 2005; 20:875–81. PMID: 16392344.33. Nascimento C, Barbosa RE, Issa JP, Watanabe E, Ito IY, Albuquerque RF Jr. Bacterial leakage along the implant-abutment interface of premachined or cast components. Int J Oral Maxillofac Surg. 2008; 37:177–80. DOI: 10.1016/j.ijom.2007.07.026. PMID: 17931833.34. Hermann JS, Schoolfield JD, Schenk RK, Buser D, Cochran DL. Influence of the size of the microgap on crestal bone change around titanium implants. A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Periodontol. 2001; 72:1372–83. DOI: 10.1902/jop.2001.72.10.1372. PMID: 11699479.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Finite element analysis on the connection types of abutment and fixture
- A three-dimensional finite-element analysis of influence of splinting in mandibular posterior implants
- Stress analysis of supporting tissues and implants according to implant fixture shapes and implant-abutment connections
- Finite element stress analysis of implant prosthesis according to connection types of implant-abutment
- THREE DIMENSIONAL FINITE ELEMENT ANALYSIS ON THE MANDIBULAR CANTILEVERED PROSTHESIS SUPPORTED BY IMPLANTS