J Korean Soc Radiol.
2017 Nov;77(5):263-285. 10.3348/jksr.2017.77.5.263.
Easy Way Out-Quick Interpretation of Musculoskeletal Radiographs: The Lower Extremity
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Medical Convergence Research Institute, and Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea. radiologie@gmail.com
- 2Department of Radiology, Inje University College of Medicine, Haeundae Paik Hospital, Busan, Korea.
- KMID: 2394041
- DOI: http://doi.org/10.3348/jksr.2017.77.5.263
Abstract
- Radiograph remains an important diagnostic tool for detection of musculoskeletal diseases despite recent advances in computed tomography (CT) or magnetic resonance imaging (MRI). Many musculoskeletal disorders are primarily diagnosed by identifying characteristic features on radiographs, which are known to have diagnostic value. In addition, radiographs provide basic information for determining the necessity of cross-sectional imaging such as CT or MRI. Therefore, radiologists should be aware of the radiographic findings of musculoskeletal diseases and they should apply them to establish the diagnosis. This article presents a review of the important radiographic findings that enable the diagnosis of musculoskeletal diseases of the lower extremity.
MeSH Terms
Figure
Reference
-
1.Renner JB. Conventional radiography in musculoskeletal imaging. Radiol Clin North Am. 2009. 47:357–372.
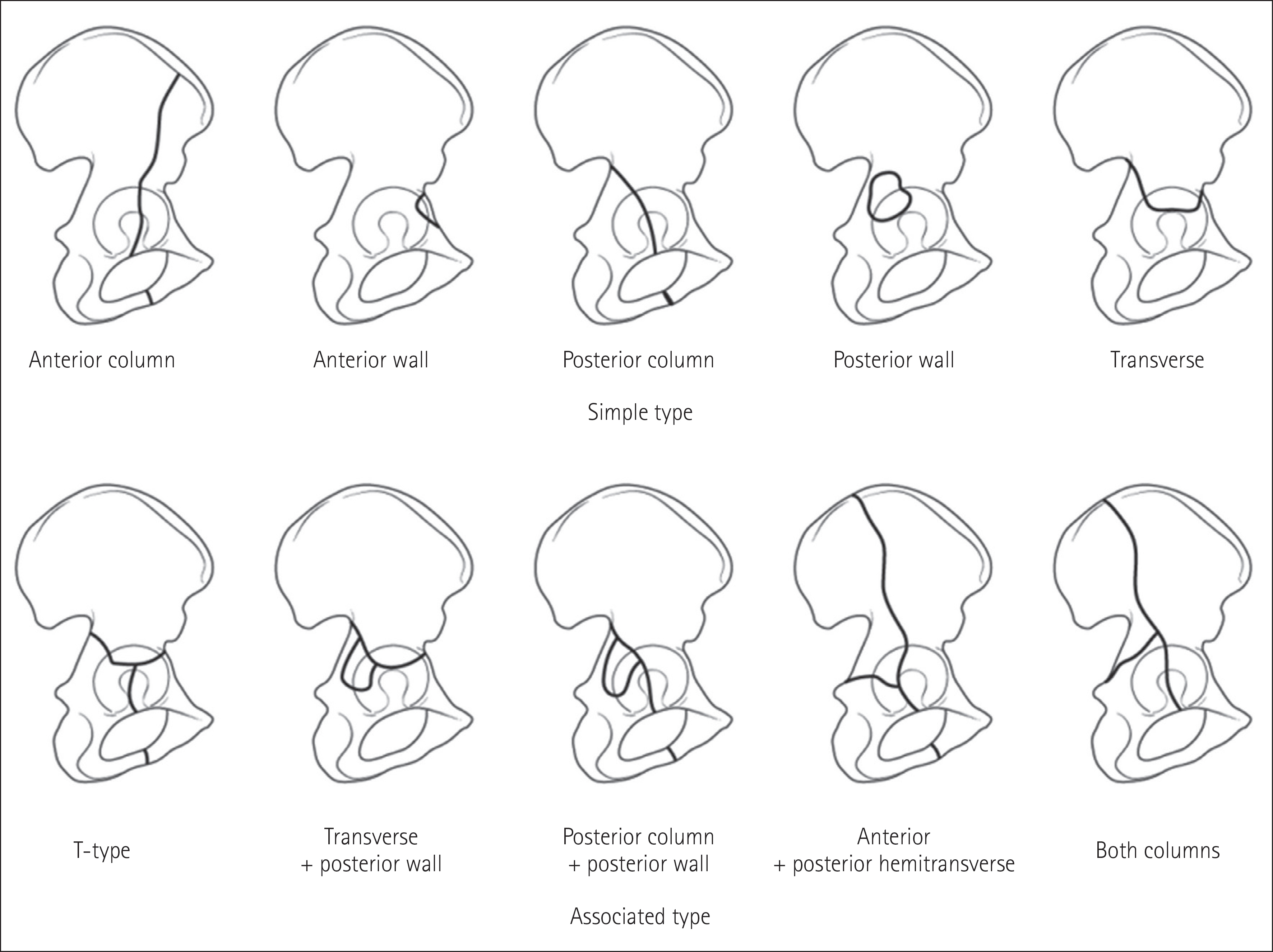
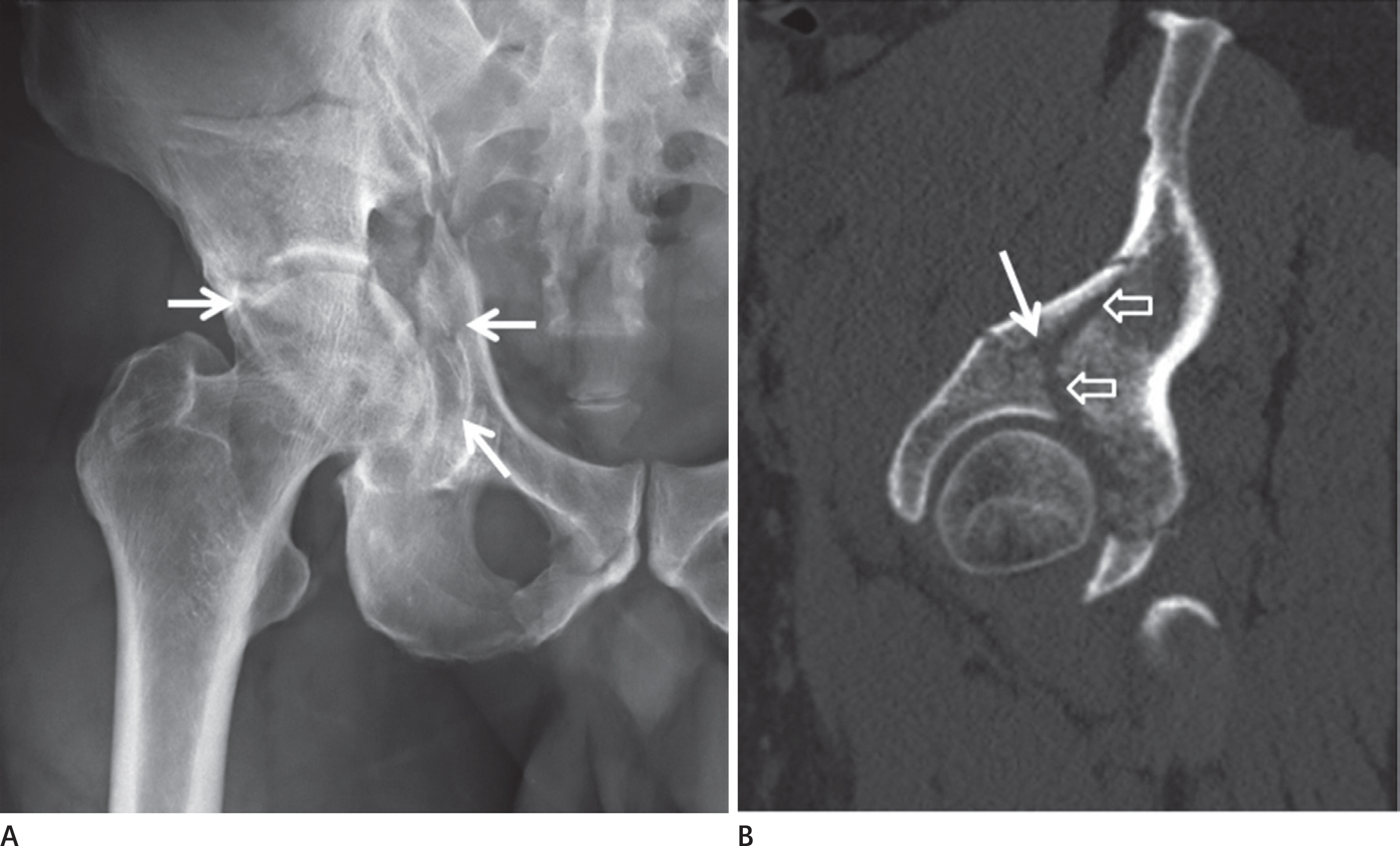
Article2.Potok PS., Hopper KD., Umlauf MJ. Fractures of the acetabu-lum: imaging, classification, and understanding. Radio-graphics. 1995. 15:7–23. discussion 23-24.
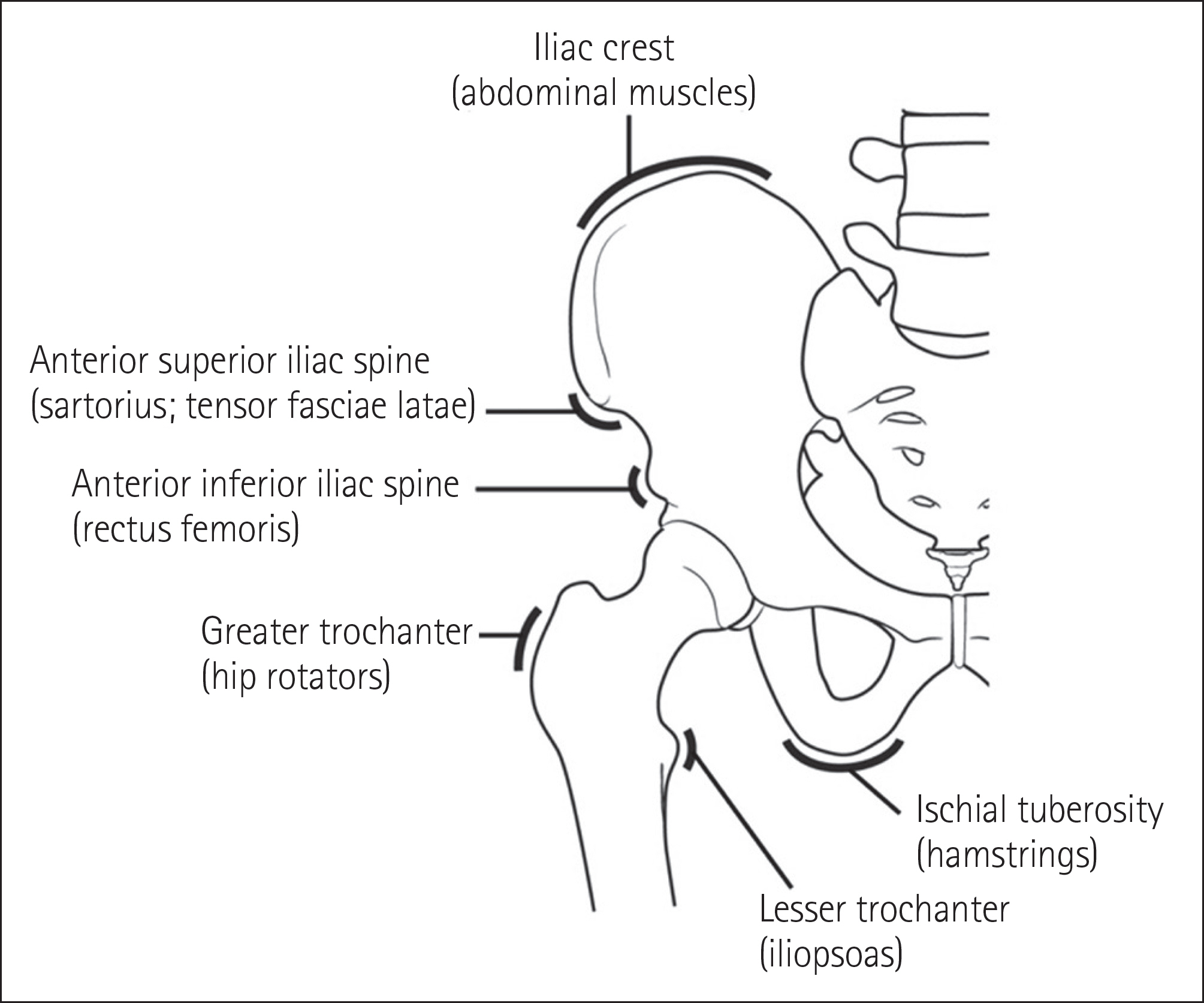
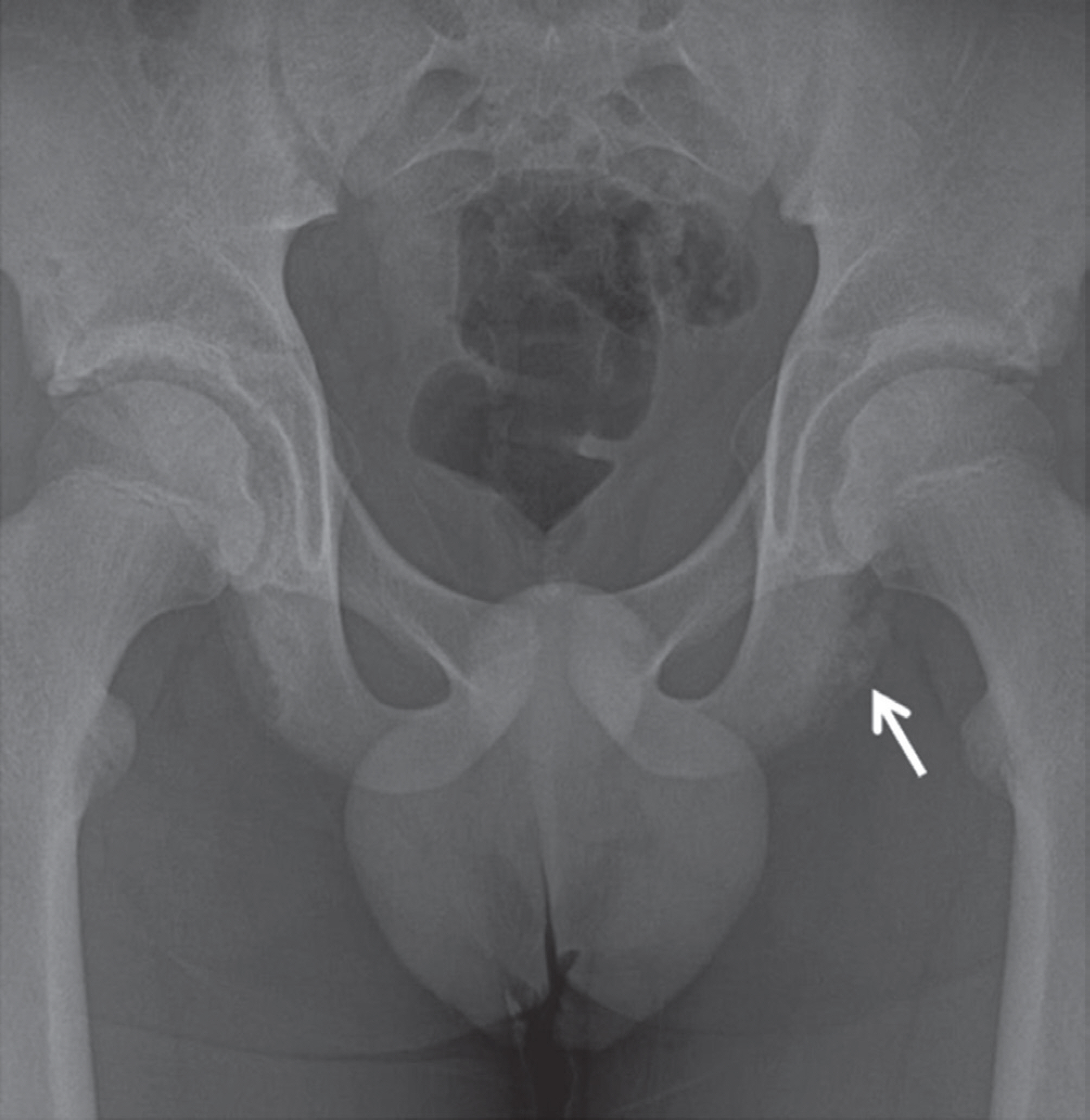
Article3.Lee SM., Lee YH. Trauma. Kang HS, Hong SH, Kang CH, editors. Musculoskeletal radiology. Reston: Bummun Education;2013. 267–339.4.Murphy D., Kaliszer M., Rice J., McElwain JP. Outcome after acetabular fracture. Prognostic factors and their inter-relationships. Injury. 2003. 34:512–517.5.Metzmaker JN., Pappas AM. Avulsion fractures of the pelvis. Am J Sports Med. 1985. 13:349–358.
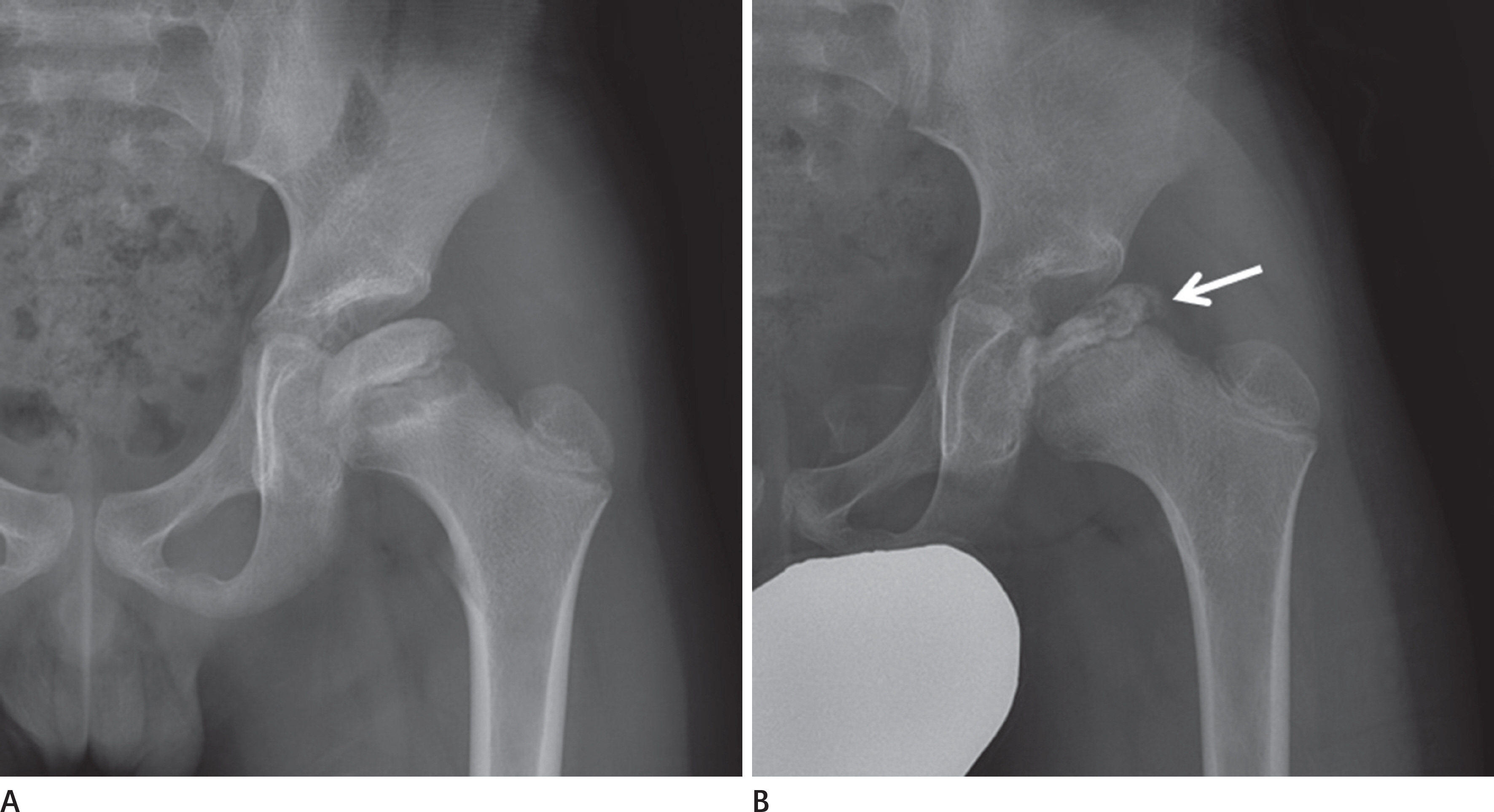
Article6.Frandsen PA., Andersen E., Madsen F., Skjødt T. Garden's clas-sification of femoral neck fractures. An assessment of inter-observer variation. J Bone Joint Surg Br. 1988. 70:588–590.
Article7.Bachiller FG., Caballer AP., Portal LF. Avascular necrosis of the femoral head after femoral neck fracture. Clin Orthop Relat Res. 2002. 399:87–109.
Article8.Rosenberg ZS., La Rocca Vieira R., Chan SS., Babb J., Akyol Y., Rybak LD, et al. Bisphosphonate-related complete atypical subtrochanteric femoral fractures: diagnostic utility of ra-diography. AJR Am J Roentgenol. 2011. 197:954–960.
Article9.Schilcher J., Michaëlsson K., Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med. 2011. 364:1728–1737.
Article10.Fisher RL. An epidemiological study of Legg-Perthes disease. J Bone Joint Surg Am. 1972. 54:769–778.
Article11.Dillon JE., Connolly SA., Connolly LP., Kim YJ., Jaramillo D. MR imaging of congenital/developmental and acquired disor-ders of the pediatric hip and pelvis. Magn Reson Imaging Clin N Am. 2005. 13:783–797.
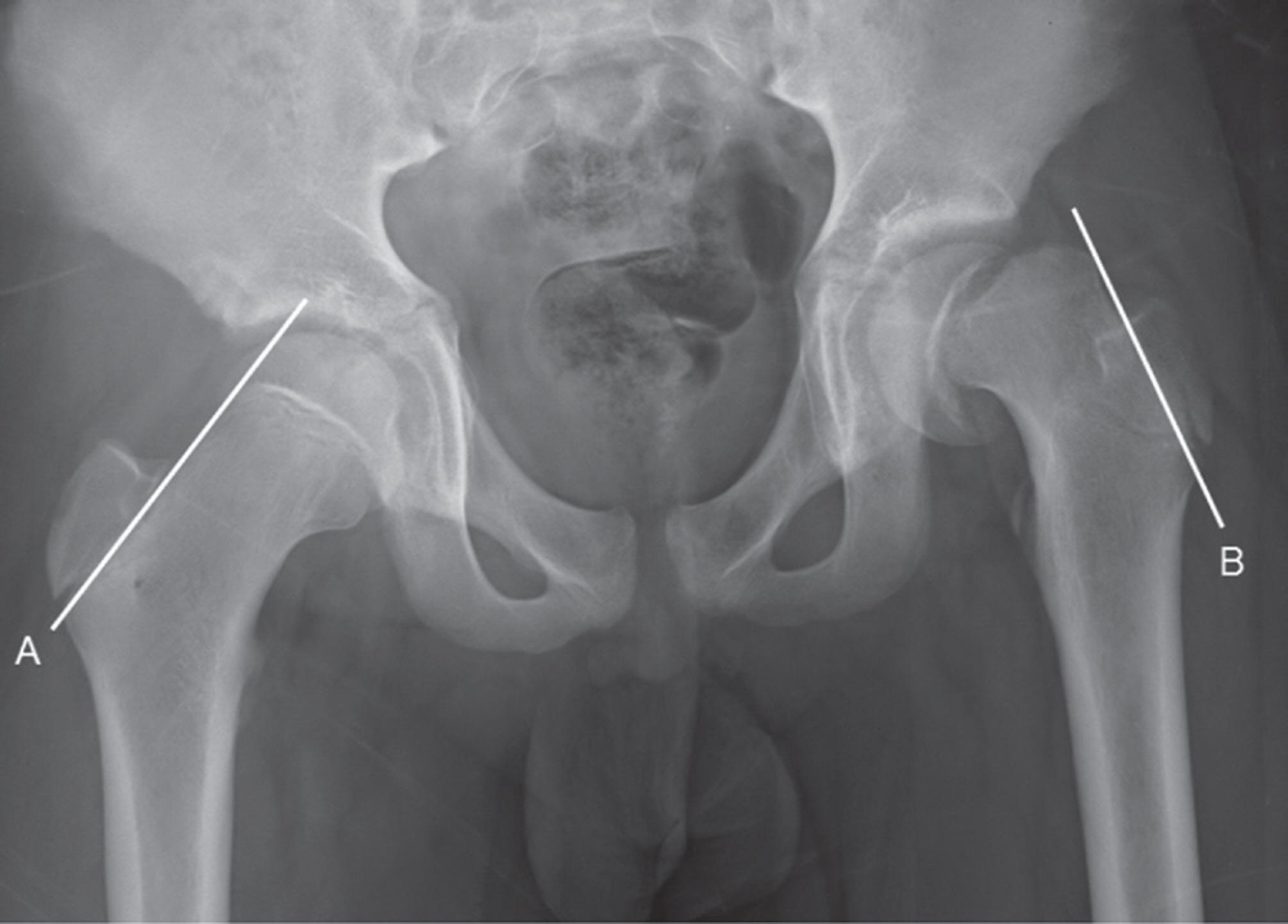
Article12.Wilcox PG., Weiner DS., Leighley B. Maturation factors in slipped capital femoral epiphysis. J Pediatr Orthop. 1988. 8:196–200.
Article13.Boles CA., el-Khoury GY. Slipped capital femoral epiphysis. Radiographics. 1997. 17:809–823.
Article14.Boyer DW., Mickelson MR., Ponseti IV. Slipped capital femo-ral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am. 1981. 63:85–95.
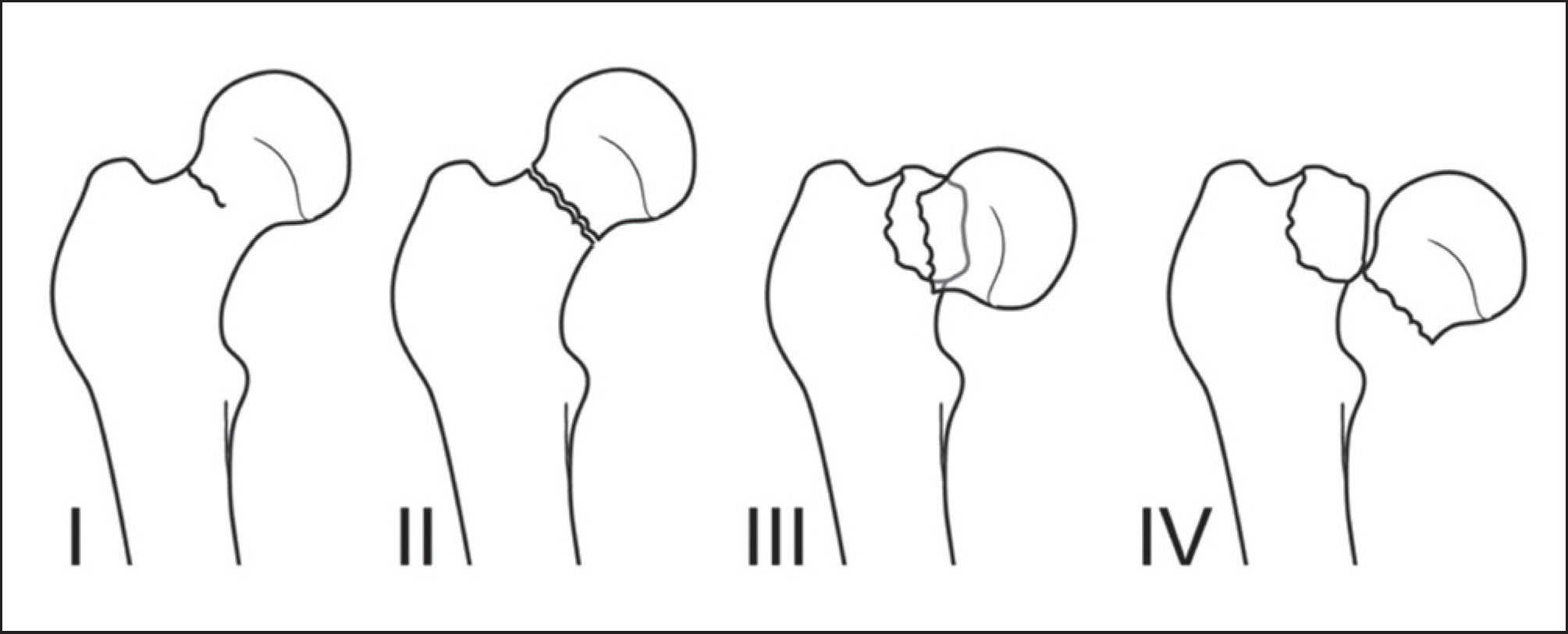
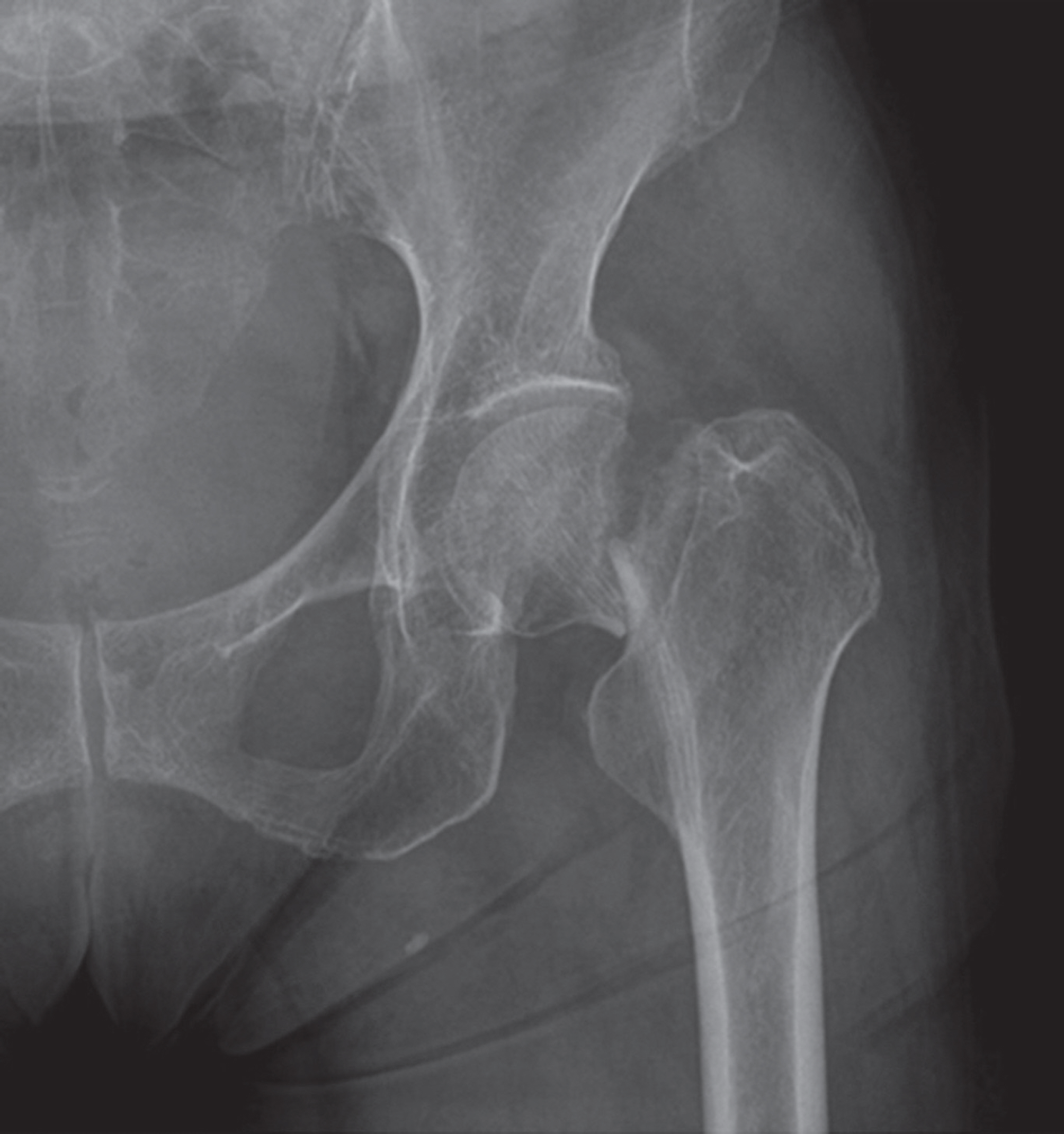
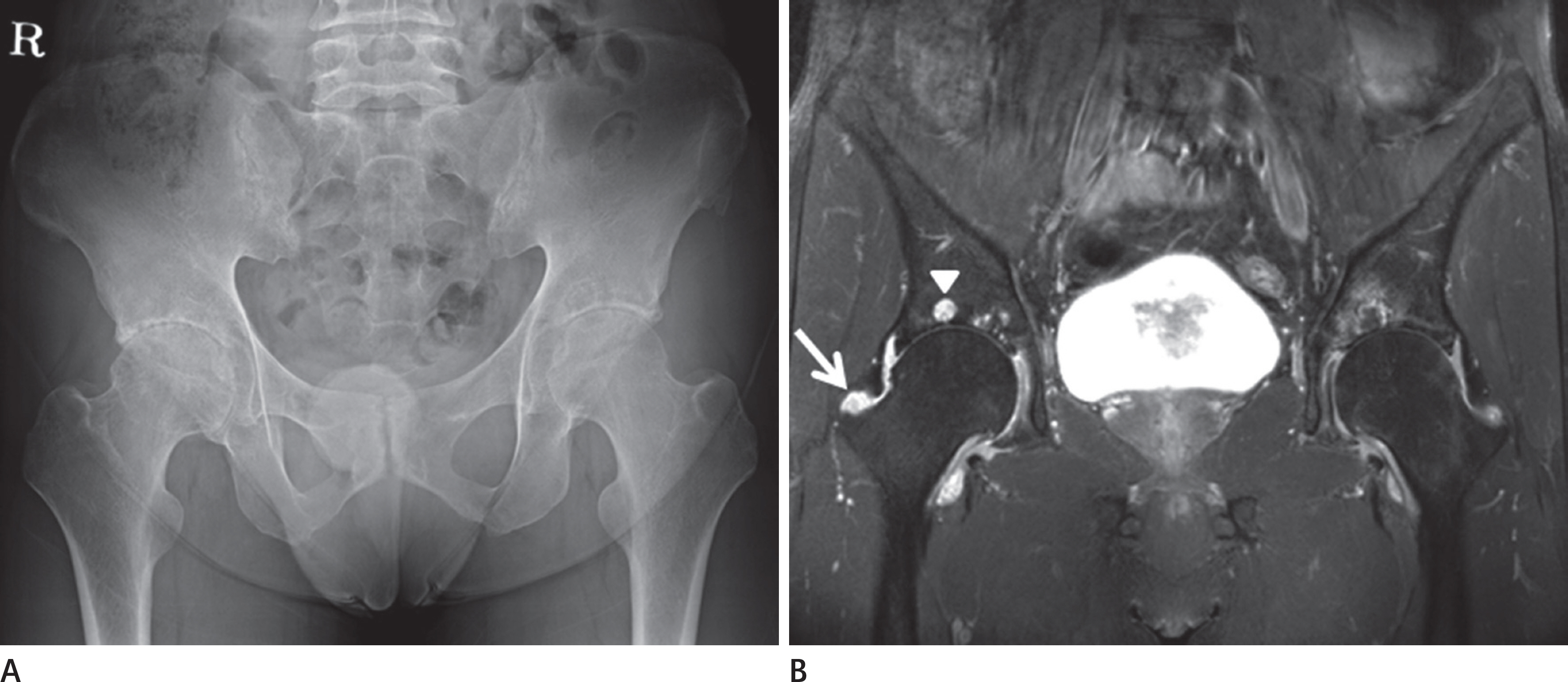
Article15.Kamal D., Traistaru R., Alexandru DO., Grecu DC., Mogoanta L. Epidemiologic study of avascular necrosis of the femoral head. Curr Health Sci J. 2013. 39:169–174.16.Jawad MU., Haleem AA., Scully SP. In brief: ficat classification: avascular necrosis of the femoral head. Clin Orthop Relat Res. 2012. 470:2636–2639.
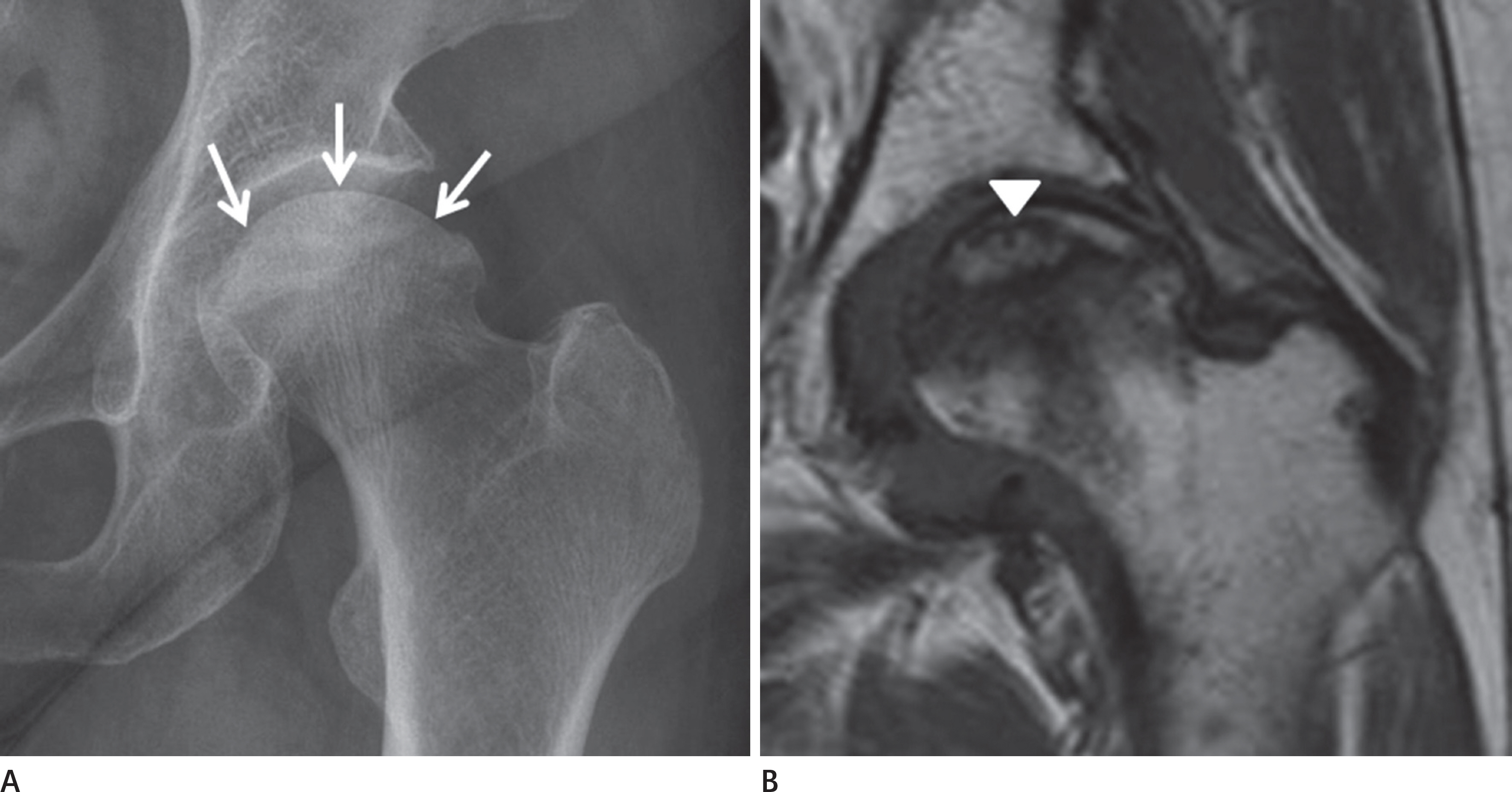
Article17.Ha DH., Na JB. Pelvis and hip joint. Kang HS, Hong SH, Kang CH, editors. Musculoskeletal radiology. Reston: Bummun Education;2013. 627–669.18.Tannast M., Siebenrock KA., Anderson SE. Femoroacetabular impingement: radiographic diagnosis--what the radiolo-gist should know. Am J Roentgenol. 2007. 188:1540–1552.
Article19.Dixon T., Benjamin J., Lund P., Graham A., Krupinski E. Femoral neck buttressing: a radiographic and histologic analysis. Skeletal Radiol. 2000. 29:587–592.
Article20.Brower A. Arthritis in black and white. Philadelphia, PA: Saunders;2012. 170–199.21.Kolmert L., Wulff K. Epidemiology and treatment of distal femoral fractures in adults. Acta Orthop Scand. 1982. 53:957–962.
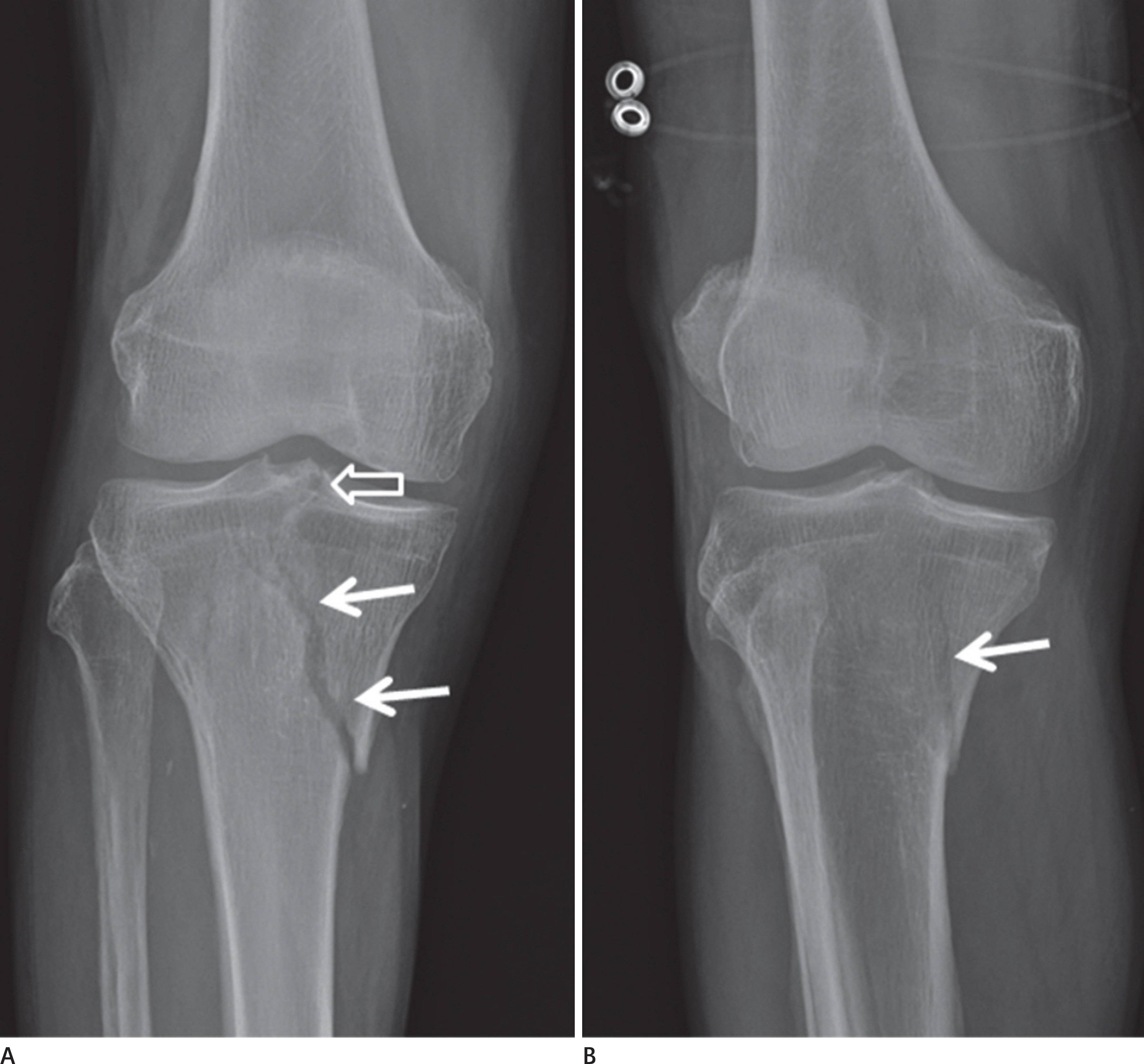
Article22.Sanders TG., Medynski MA., Feller JF., Lawhorn KW. Bone con-tusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000. 20:Spec No:. S135–S151.
Article23.Arneson TJ., Melton LJ 3rd., Lewallen DG., O'Fallon WM. Epi-demiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res. 1988. 234:188–194.
Article24.Marsh JL., Slongo TF., Agel J., Broderick JS., Creevey W., De-Coster TA, et al. Fracture and dislocation classification com-pendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007. 21(10 Suppl):S1–S133.25.Markhardt BK., Gross JM., Monu JU. Schatzker classification of tibial plateau fractures: use of CT and MR imaging im-proves assessment. Radiographics. 2009. 29:585–597.
Article26.O WH., Craig C., Banks HH. Epiphyseal injuries. Pediatr Clin North Am. 1974. 21:407–422.27.Lipp EJ. Athletic physeal injury in children and adolescents. Orthop Nurs. 1998. 17:17–22.28.Greenspan A. Lower limb, part II. Greenspan A, editor. Or-thopedic imaging: a practical approach. 5th ed.Philadel-phia: Lippincott Williams & Wilkins;2011. 258–307.29.Dupuis CS., Westra SJ., Makris J., Wallace EC. Injuries and conditions of the extensor mechanism of the pediatric knee. Radiographics. 2009. 29:877–886.
Article30.Gottsegen CJ., Eyer BA., White EA., Learch TJ., Forrester D. Avulsion fractures of the knee: imaging findings and clini-cal significance. Radiographics. 2008. 28:1755–1770.
Article31.Escobedo EM., Mills WJ., Hunter JC. The “reverse Segond" fracture: association with a tear of the posterior cruciate lig-ament and medial meniscus. AJR Am J Roentgenol. 2002. 178:979–983.32.White EA., Patel DB., Matcuk GR., Forrester DM., Lundquist RB., Hatch GF 3rd, et al. Cruciate ligament avulsion fractures: anatomy, biomechanics, injury patterns, and approach to management. Emerg Radiol. 2013. 20:429–440.
Article33.Griffith JF., Antonio GE., Tong CW., Ming CK. Cruciate liga-ment avulsion fractures. Arthroscopy. 2004. 20:803–812.
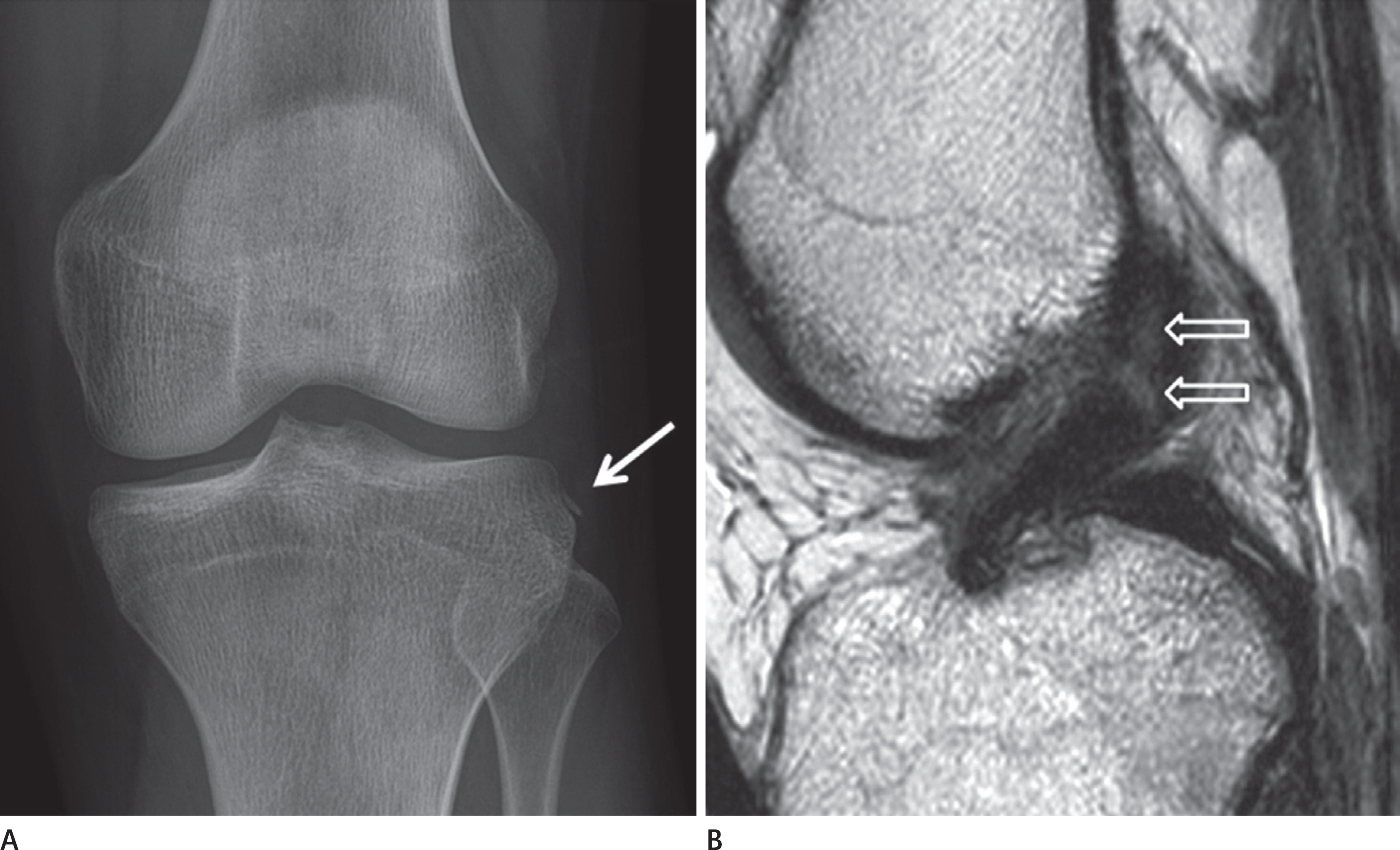
Article34.Hunter TB., Peltier LF., Lund PJ. Radiologic history exhibit. Musculoskeletal eponyms: who are those guys? Radiograph-ics. 2000. 20:819–836.35.McAnally JL., Southam SL., Mlady GW. New thoughts on the origin of Pellegrini-Stieda: the association of PCL injury and medial femoral epicondylar periosteal stripping. Skeletal Radiol. 2009. 38:193–198.
Article36.Sundararajan SR., Rajasekaran S., Bernard SL. Displaced ante-rior cruciate ligament avulsion fractures: arthroscopic sta-ple fixation. Indian J Orthop. 2011. 45:324–329.
Article37.Juhng SK., Park JG. Knee, part II. Kang HS, Hong SH, Kang CH, editors. Musculoskeletal radiology. Reston: Bummun Edu-cation;2013. 715–744.38.De Smet AA., Fisher DR., Burnstein MI., Graf BK., Lange RH. Val-ue of MR imaging in staging osteochondral lesions of the talus (osteochondritis dissecans): results in 14 patients. AJR Am J Roentgenol. 1990. 154:555–558.
Article39.Stevens MA., El-Khoury GY., Kathol MH., Brandser EA., Chow S. Imaging features of avulsion injuries. Radiographics. 1999. 19:655–672.
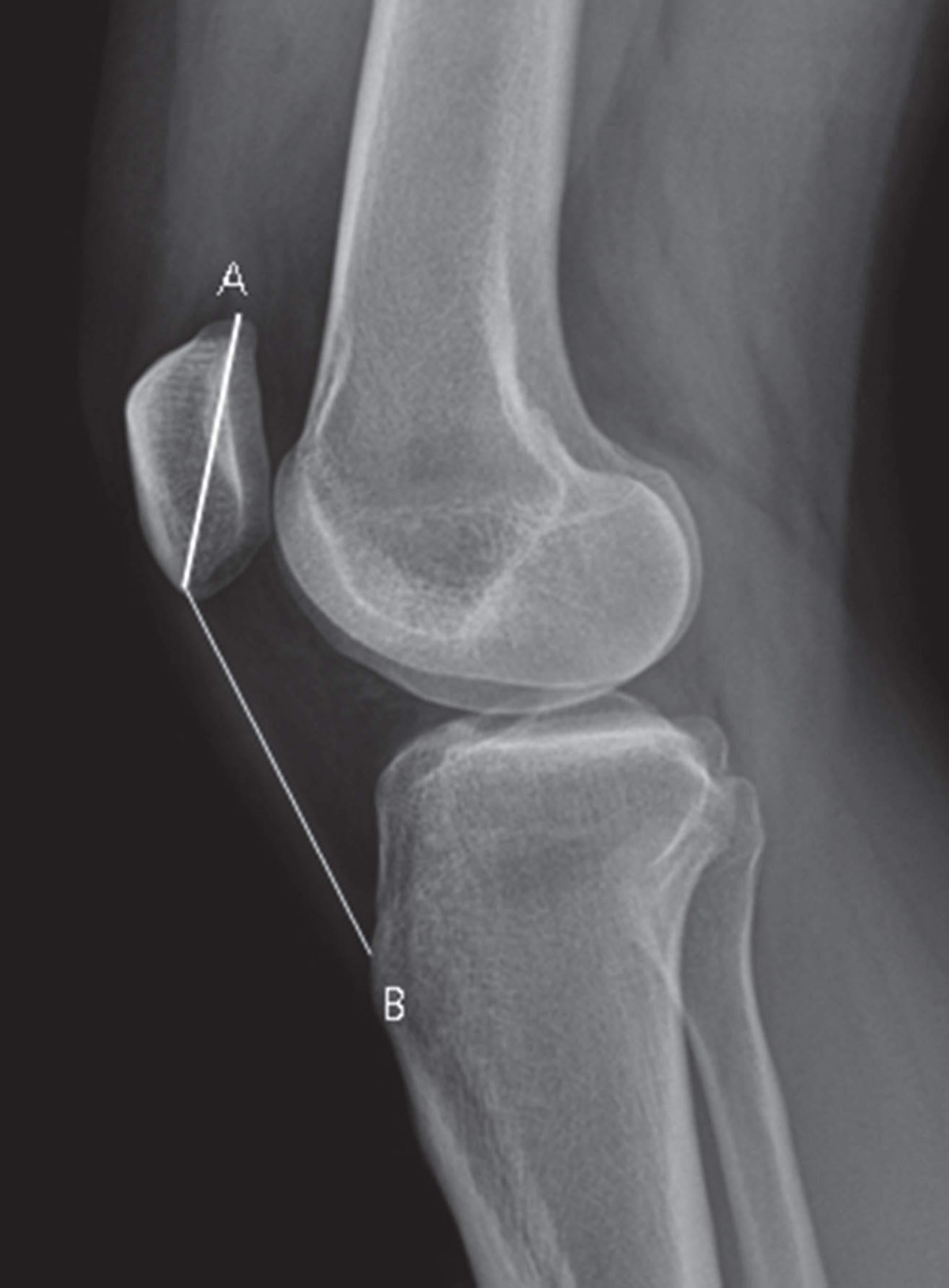
Article40.Insall J., Salvati E. Patella position in the normal knee joint. Radiology. 1971. 101:101–104.
Article41.Caton J., Deschamps G., Chambat P., Lerat JL., Dejour H. [Patella infera. Apropos of 128 cases]. Rev Chir Orthop Reparatrice Appar Mot. 1982. 68:317–325.42.Blackburne JS., Peel TE. A new method of measuring patel-lar height. J Bone Joint Surg Br. 1977. 59:241–242.
Article43.Dath R., Chakravarthy J., Porter KM. Patella dislocations. Trauma. 2006. 8:5–11.
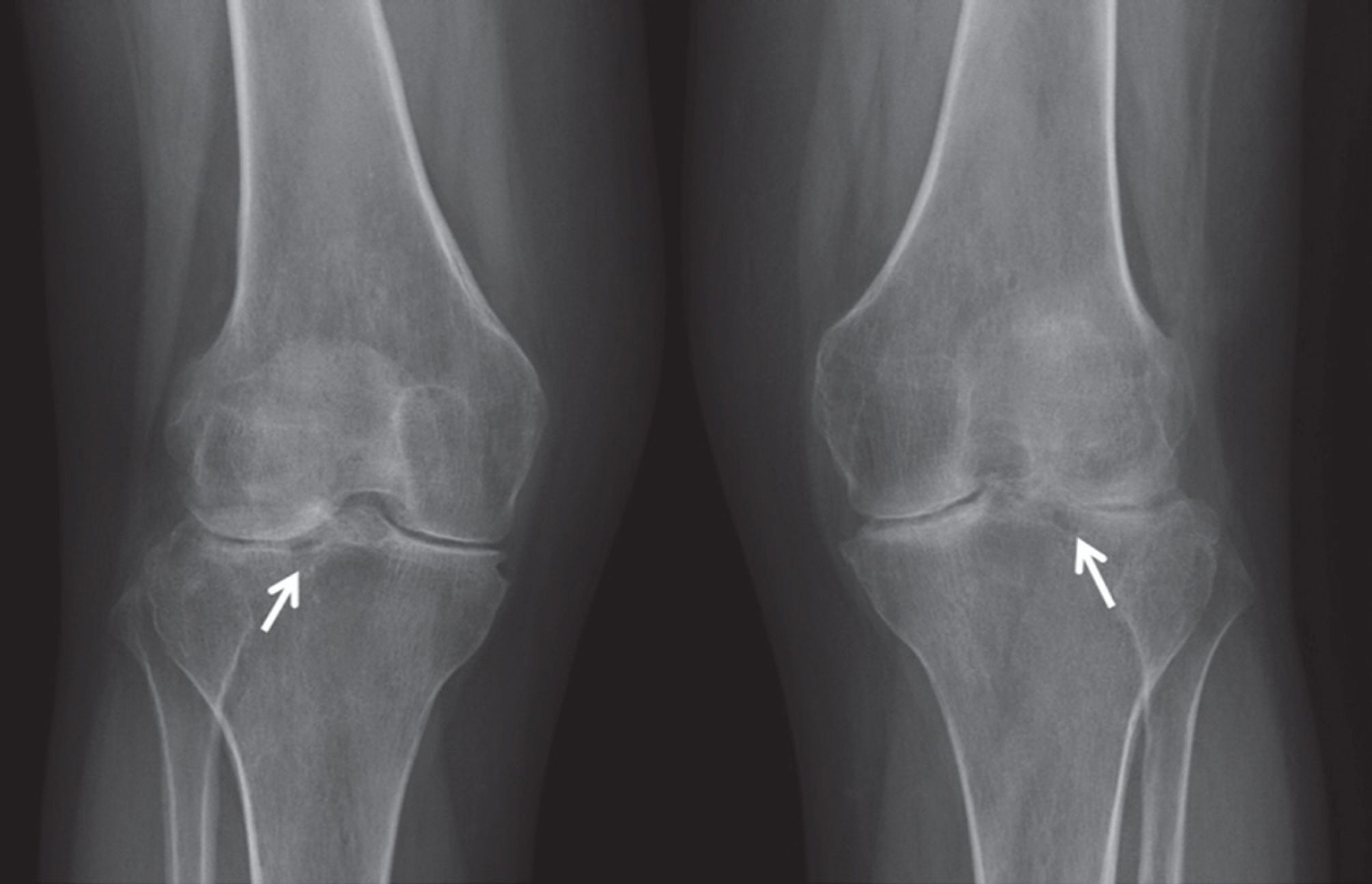
Article44.Sung MS., Chun KA. Degenerative joint disease. Kang HS, Hong SH, Kang CH, editors. Musculoskeletal radiology. Reston: Bummun Education;2013. 147–163.45.Kellgren JH., Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957. 16:494–502.
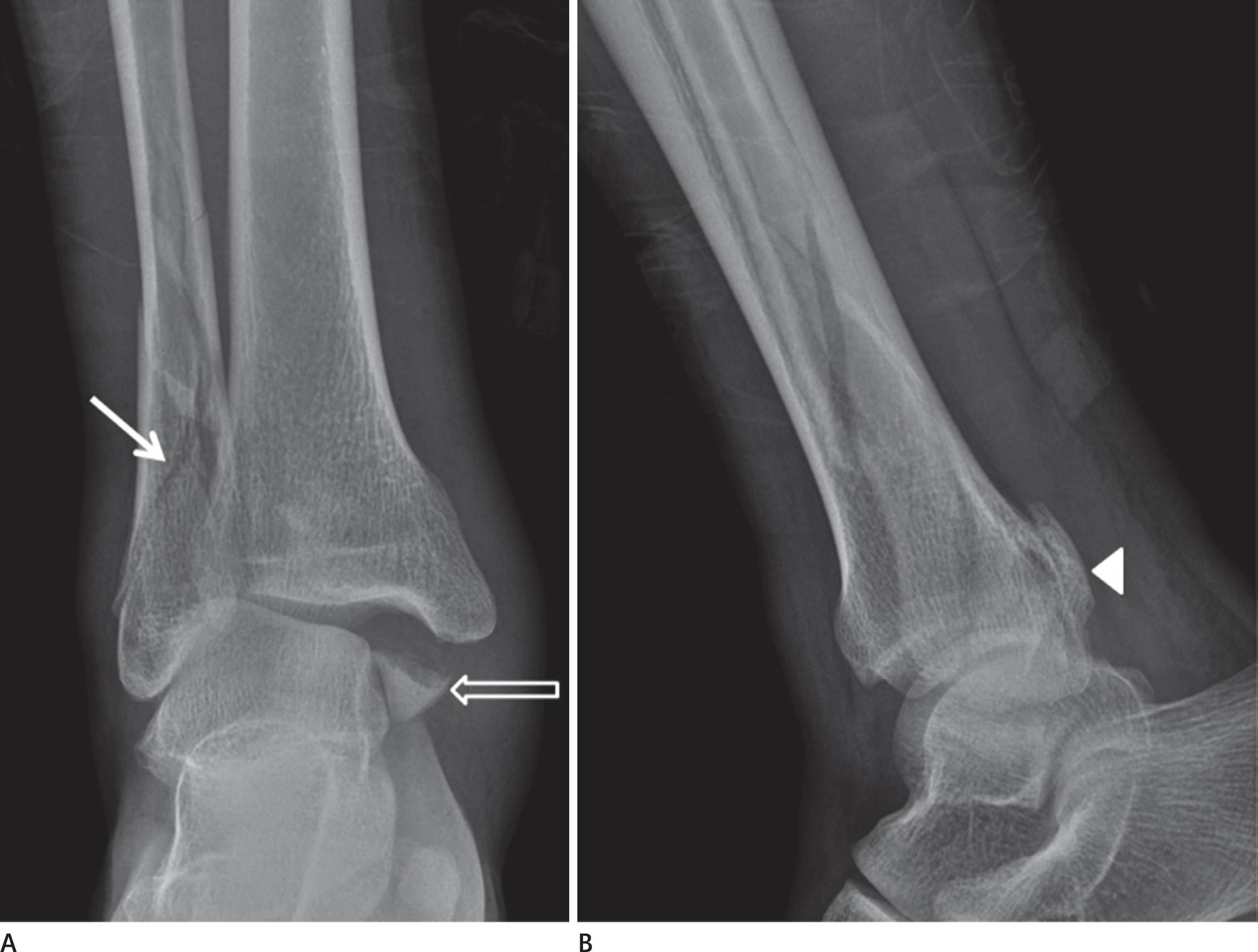
Article46.Arimoto HK., Forrester DM. Classification of ankle fractures: an algorithm. AJR Am J Roentgenol. 1980. 135:1057–1063.
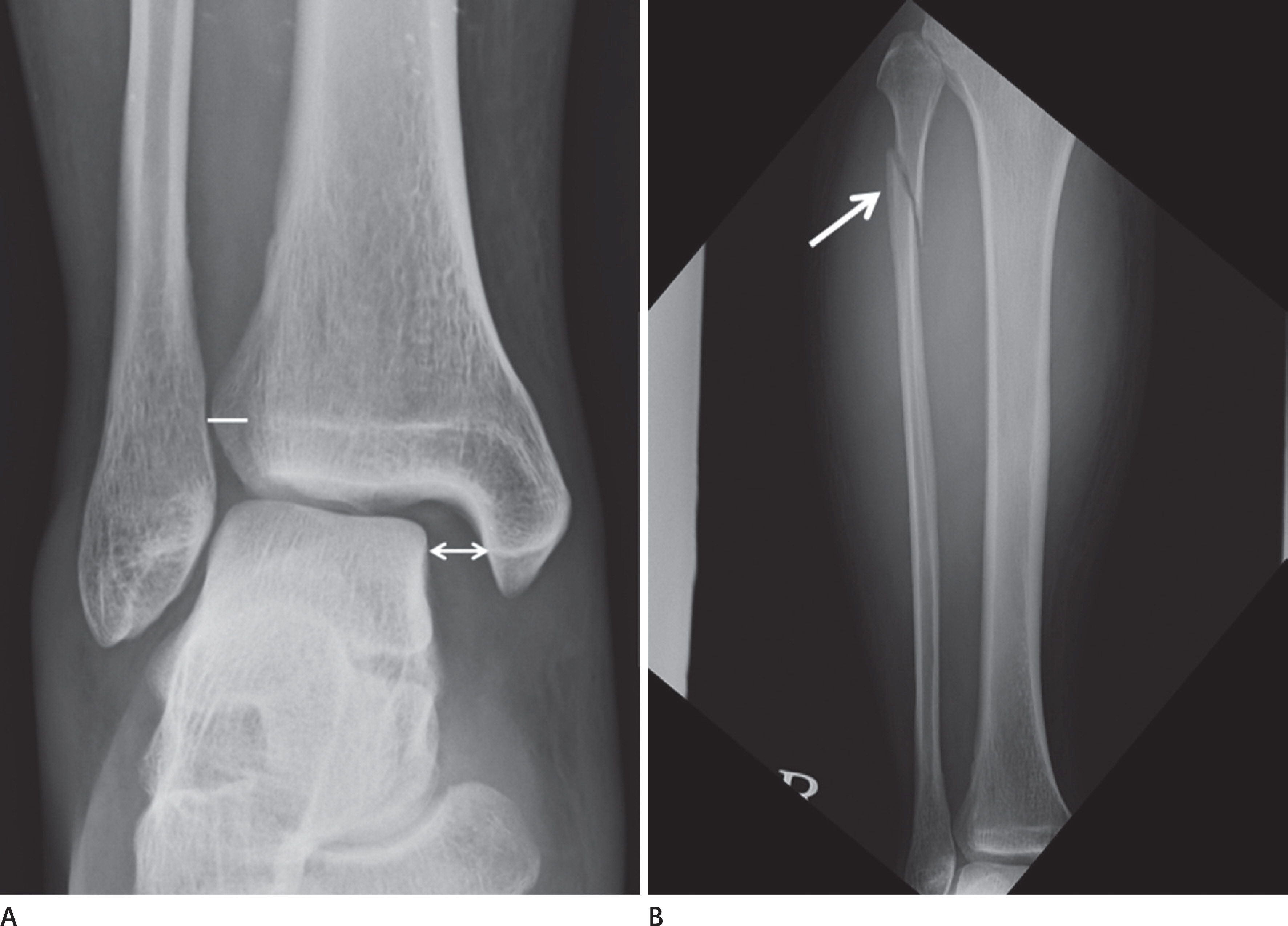
Article47.Arastu MH., Demcoe R., Buckley RE. Current concepts review: ankle fractures. Acta Chir Orthop Traumatol Cech. 2012. 79:473–483.48.Sclafani SJ. Ligamentous injury of the lower tibiofibular syndesmosis: radiographic evidence. Radiology. 1985. 156:21–27.
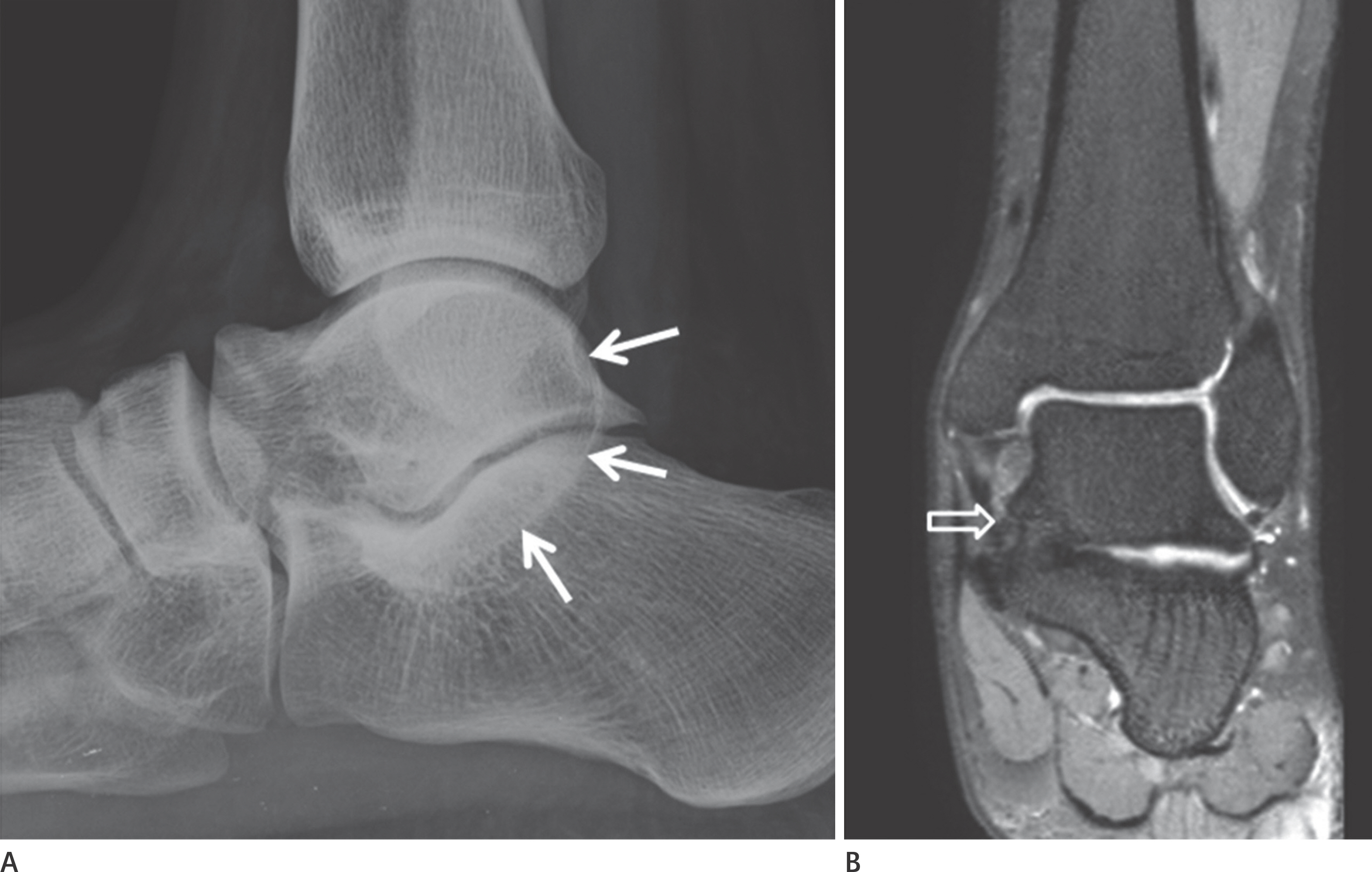
Article49.Greenspan A. Lower limb, part III. Greenspan A, editor. Or-thopedic imaging: a practical approach. 5th ed.Philadel-phia: Lippincott Williams & Wilkins;2011. 294–345.50.Badillo K., Pacheco JA., Padua SO., Gomez AA., Colon E., Vidal JA. Multidetector CT evaluation of calcaneal fractures. Ra-diographics. 2011. 31:81–92.
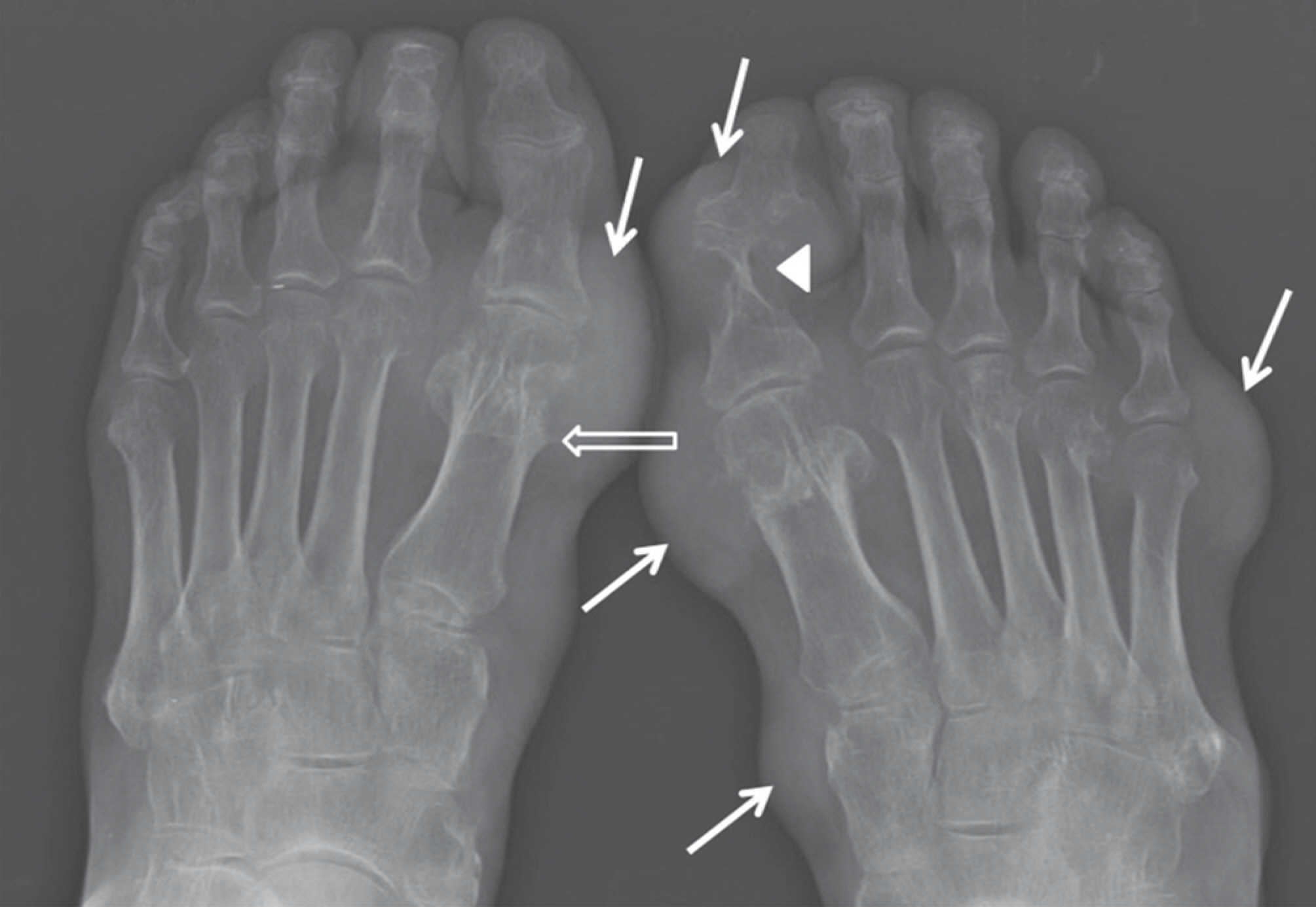
Article51.Hardcastle PH., Reschauer R., Kutscha-Lissberg E., Schoffmann W. Injuries to the tarsometatarsal joint. Incidence, classification and treatment. J Bone Joint Surg Br. 1982. 64:349–356.
Article52.Burroughs KE., Reimer CD., Fields KB. Lisfranc injury of the foot: a commonly missed diagnosis. Am Fam Physician. 1998. 58:118–124.53.Goiney RC., Connell DG., Nichols DM. CT evaluation of tarso-metatarsal fracture-dislocation injuries. AJR Am J Roentgen-ol. 1985. 144:985–990.
Article54.Alexander AH., Lichtman DM. Surgical treatment of tran-schondral talar-dome fractures (osteochondritis dissecans). Long-term follow-up. J Bone Joint Surg Am. 1980. 62:646–652.
Article55.Choi YS., Chun TJ. Foot and ankle. Kang HS, Hong SH, Kang CH, editors. Musculoskeletal radiology. Reston: Bummun Education;2013. 745–798.56.Naran KN., Zoga AC. Osteochondral lesions about the an-kle. Radiol Clin North Am. 2008. 46:995–1002.
Article57.Pearce DH., Mongiardi CN., Fornasier VL., Daniels TR. Avascu-lar necrosis of the talus: a pictorial essay. Radiographics. 2005. 25:399–410.
Article58.Park JS., Ryu KN. Osteonecrosis and osteochondrosis. Kang HS, Hong SH, Kang CH, editors. Musculoskeletal radiolo-gy. Reston: Bummun Education;2013. 229–265.59.Torriani M., Thomas BJ., Bredella MA., Ouellette H. MRI of meta-tarsal head subchondral fractures in patients with forefoot pain. AJR Am J Roentgenol. 2008. 190:570–575.
Article60.Ashman CJ., Klecker RJ., Yu JS. Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. Radiographics. 2001. 21:1425–1440.
Article61.Staheli LT., Chew DE., Corbett M. The longitudinal arch. A sur-vey of eight hundred and eighty-two feet in normal chil-dren and adults. J Bone Joint Surg Am. 1987. 69:426–428.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dynamic Ultrasonography in Musculoskeletal System-Lower Extremity and Miscellaneous disorders
- Musculoskeletal ultrasound: athletic injuries of the lower extremity
- Dynamic Ultrasonography in Musculoskeletal System: Upper Extremity
- Commuting time and musculoskeletal pain in the relationship with working time: a cross-sectional study
- The Role of Fat Tissues in the Diagnosis of Musculoskeletal Imaging