Ewha Med J.
2017 Oct;40(4):164-167. 10.12771/emj.2017.40.4.164.
Brugada Syndrome Patient Undertaken Brachial Plexus Block
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, International St. Mary's Hospital, Catholic Kwandong University, Incheon, Korea.
- 2Department of Anesthesiology and Pain Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea. anesthpark@hanmail.net
- KMID: 2393721
- DOI: http://doi.org/10.12771/emj.2017.40.4.164
Abstract
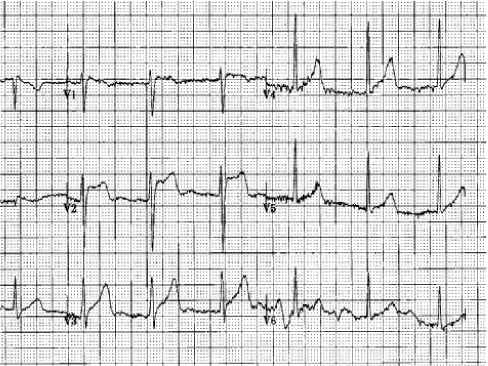
- Brugada syndrome is an arrhythmic syndrome characterized by right bundle branch block, ST segment elevation in the precordial lead (V1-V3), and sudden death caused by ventricular fibrillation, which is not effectively prevented by anti-arrhythmic drug therapy. We are reporting a 30-year-old male patient with Brugada syndrome who got an exploratory laparotomy and a tenorrhaphy due to stab wound which was managed with general anesthesia and brachial plexus block without any complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992; 20:1391–1396.2. Hedley PL, Jorgensen P, Schlamowitz S, Moolman-Smook J, Kanters JK, Corfield VA, et al. The genetic basis of Brugada syndrome: a mutation update. Hum Mutat. 2009; 30:1256–1266.3. Benito B, Brugada J, Brugada R, Brugada P. Brugada syndrome. Rev Esp Cardiol. 2009; 62:1297–1315.4. Carey SM, Hocking G. Brugada syndrome: a review of the implications for the anaesthetist. Anaesth Intensive Care. 2011; 39:571–577.5. Dulu A, Pastores SM, McAleer E, Voigt L, Halpern NA. Brugada electrocardiographic pattern in a postoperative patient. Crit Care Med. 2005; 33:1634–1637.6. Kloesel B, Ackerman MJ, Sprung J, Narr BJ, Weingarten TN. Anesthetic management of patients with Brugada syndrome: a case series and literature review. Can J Anaesth. 2011; 58:824–836.7. Miyazaki T, Mitamura H, Miyoshi S, Soejima K, Aizawa Y, Ogawa S. Autonomic and antiarrhythmic drug modulation of ST segment elevation in patients with Brugada syndrome. J Am Coll Cardiol. 1996; 27:1061–1070.8. Probst V, Mabo P, Sacher F, Babuty D, Mansourati J, Le Marec H. Effect of baroreflex stimulation using phenylephrine injection on ST segment elevation and ventricular arrhythmia-inducibility in Brugada syndrome patients. Europace. 2009; 11:382–384.9. Postema PG, Wolpert C, Amin AS, Probst V, Borggrefe M, Roden DM, et al. Drugs and Brugada syndrome patients: review of literature, recommendation, and an up-to-date website (www.brugadadrugs.org). Heart Rhythm. 2009; 6:1335–1341.10. Edge CJ, Blackman DJ, Gupta K, Sainsbury M. General anaesthesia in a patient with Brugada syndrome. Br J Anaesth. 2002; 89:788–791.11. Kim JS, Park SY, Min SK, Kim JH, Lee SY, Moon BK, et al. Anaesthesia in patients with Brugada syndrome. Acta Anaesthesiol Scand. 2004; 48:1058–1061.12. Theodotou N, Cillo JE Jr. Brugada syndrome (sudden unexpected death syndrome): perioperative and anesthetic management in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2009; 67:2021–2025.13. Duque M, Santos L, Ribeiro S, Catre D. Anesthesia and Brugada syndrome: a 12-year case series. J Clin Anesth. 2017; 36:168–173.14. Knudsen K, Beckman Suurkula M, Blomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of iv infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth. 1997; 78:507–514.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Horner's Syndrome following supraclavicular brachial plexus block
- Prolonged Horner's Syndrome Following Interscalene Brachial Plexus Block: A case report
- The Efficacy of Ultrasound-Guided Brachial Plexus Block in Trauma Patients
- Phrenic nerve palsy following coracoid infraclavicular brachial plexus block
- Clinical Evaluation of Parascalene Technique on Brachial Plexus Block