Korean Circ J.
2017 Jul;47(4):446-454. 10.4070/kcj.2017.0008.
Blood Pressure Targets and Clinical Outcomes in Patients with Acute Myocardial Infarction
- Affiliations
-
- 1Division of Cardiology, Chonnam National University Hospital, Cardiovascular Convergence Research Center Nominated by Korea Ministry of Health and Welfare, Gwangju, Korea. hyj200@hanmail.net
- KMID: 2392881
- DOI: http://doi.org/10.4070/kcj.2017.0008
Abstract
- BACKGROUND AND OBJECTIVES
The optimal blood pressure (BP) target in patients with a history of acute myocardial infarction (MI) remains as a subject of debate. The "˜J curve phenomenon' has been suggested as a target for BP control, however, it is unclear whether this phenomenon can be applied to MI patients. We analyzed patients with acute MI and investigated whether the "˜J curve phenomenon' exists in this population.
SUBJECTS AND METHODS
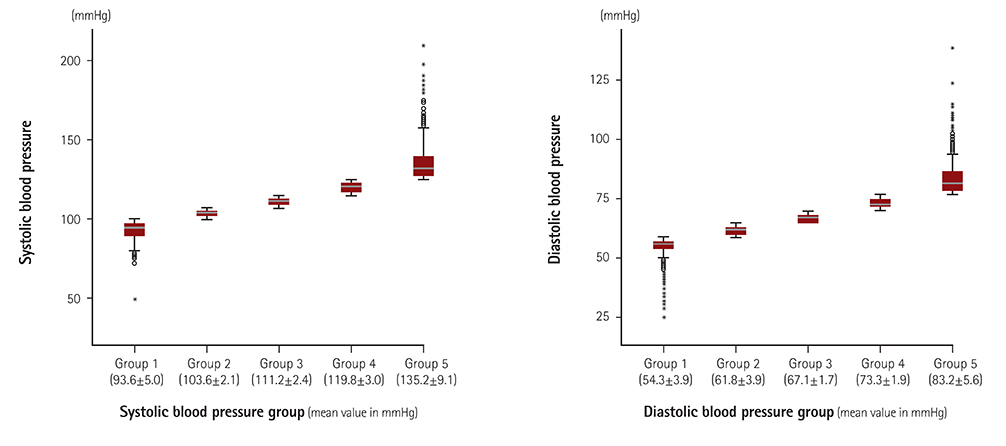
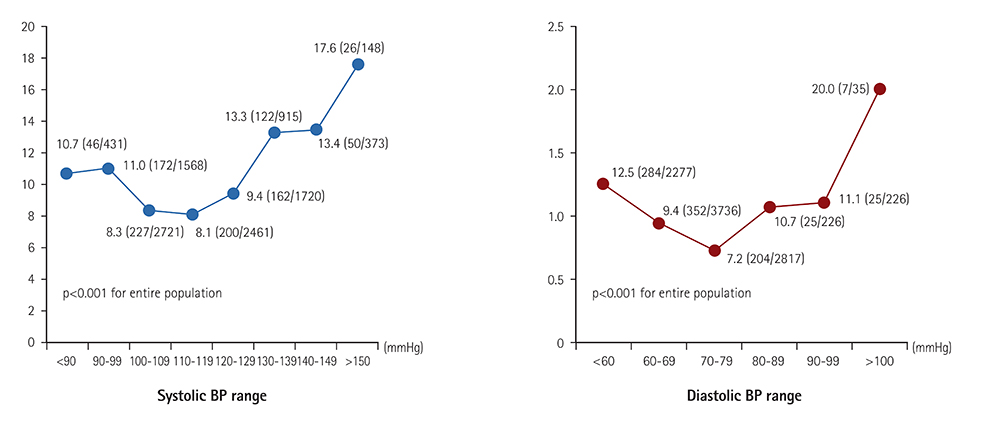
Data were obtained from a nationwide prospective Korea Acute Myocardial Infarction Registry, which included 10337 patients with acute MI who underwent percutaneous coronary intervention (PCI) between 2011 and 2014. The patients were divided into quintiles according to systolic blood pressure (SBP) and diastolic blood pressure (DBP), which were measured during a two-year clinical follow up. Two-year cumulative incidence of major adverse cardiac events (MACE) was analyzed among the groups.
RESULTS
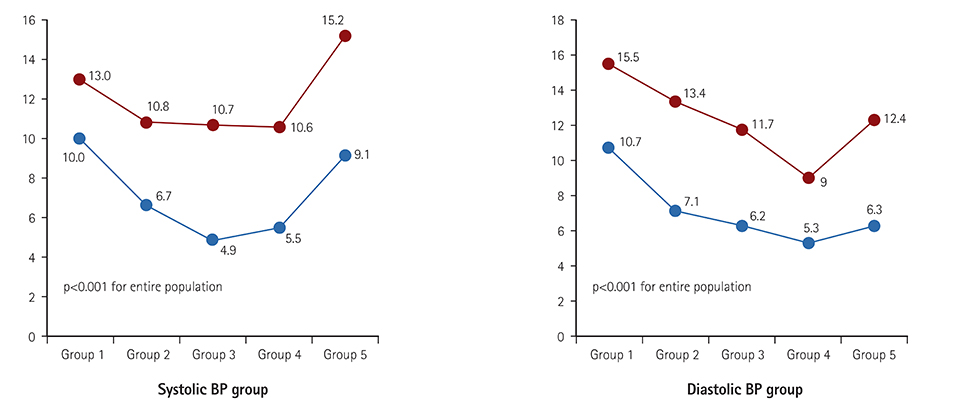
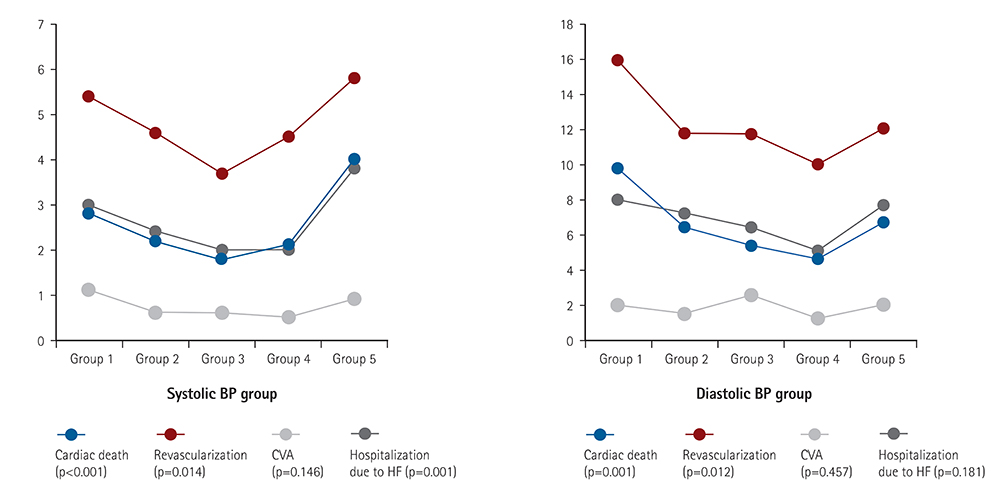
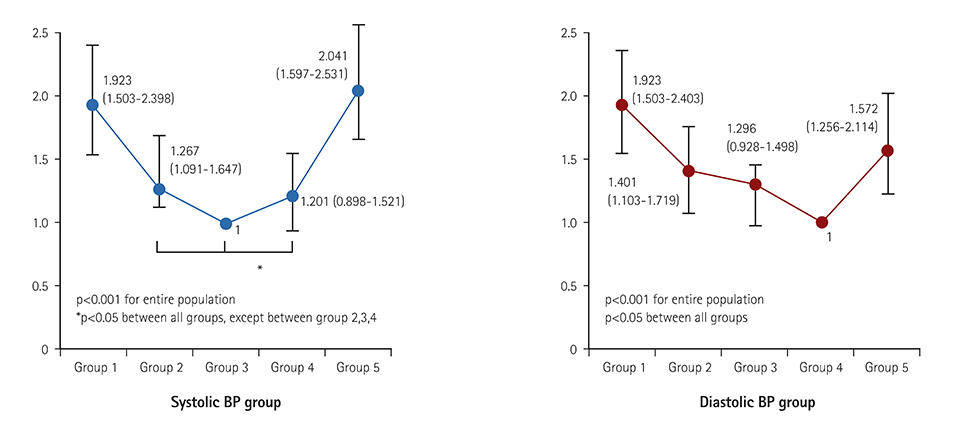
MACE was defined as a composite of cardiac death, need for recurrent revascularization (repeated PCI or coronary arterial bypass graft due to recurrent anginal symptoms or reoccurrence of MI), ischemic cerebrovascular accident, and need for hospitalization due to heart failure. During the two-year follow up, the total cumulative incidence of MACE was 9.7% (n=1005). BP-MACE analysis showed a U-shaped curve for both SBP and DBP, with the lowest MACE rate in quintiles with an average SBP of 112.2 mmHg and DBP of 73.3 mmHg. On Cox regression analysis, the U-shaped relation was statistically significant.
CONCLUSION
In patients with acute MI, a "˜U curve phenomenon' was observed when assessing patient BP control versus MACE rate.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The J-curve between Diastolic Blood Pressure and Risk of All-cause and Cardiovascular Death
Heejin Kimm, Yejin Mok, Sun Ju Lee, Sunmi Lee, Joung Hwan Back, Sun Ha Jee
Korean Circ J. 2018;48(1):36-47. doi: 10.4070/kcj.2017.0036.
Reference
-
1. Rosendorff C, Lackland DT, Allison M, et al. Treatment of hypertension in patients with coronary artery disease: a scientific statement from the American heart association, american college of cardiology, and American society of hypertension. J Am Coll Cardiol. 2015; 65:1998–2038.2. Kim JH, Chae SC, Oh DJ, et al. Multicenter cohort study of acute myocardial infarction in Korea - interim analysis of the Korea acute myocardial infarction registry-national institutes of health registry. Circ J. 2016; 80:1427–1436.3. Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002; 360:1903–1913.4. Neal B, MacMahon S, Chapman N, et al. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood pressure lowering treatment trialists' collaboration. Lancet. 2000; 356:1955–1964.5. Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001; 345:1291–1297.6. Psaty BM, Furberg CD, Kuller LH, et al. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001; 161:1183–1192.7. Denardo SJ, Gong Y, Nichols WW, et al. Blood pressure and outcomes in very old hypertensive coronary artery disease patients: an INVEST substudy. Am J Med. 2010; 123:719–726.8. Chin CT, Chen AY, Wang TY, et al. Risk adjustment for in-hospital mortality of contemporary patients with acute myocardial infarction: the Acute Coronary Treatment and Intervention Outcomes Network (ACTION) Registry-Get With The Guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J. 2011; 161:113–122.e2.9. Chang WC, Boersma E, Granger CB, et al. Dynamic prognostication in non-ST-elevation acute coronary syndromes: insights from GUSTO-IIB and PURSUIT. Am Heart J. 2004; 148:62–71.10. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Circulation. 2012; 126:2020–2035.11. Frazier CG, Shah SH, Armstrong PW, et al. Prevalence and management of hypertension in acute coronary syndrome patients varies by sex: observations from the Sibrafiban versus aspirin to Yield Maximum Protection from ischemic Heart events postacute cOroNary sYndromes (SYMPHONY) randomized clinical trials. Am Heart J. 2005; 150:1260–1267.12. Kang DG, Jeong MH, Ahn Y, et al. Clinical effects of hypertension on the mortality of patients with acute myocardial infarction. J Korean Med Sci. 2009; 24:800–806.13. Strauer BE. The concept of coronary flow revserve. J Cardiovasc Pharmacol. 1992; 19:suppl 5. S67–S80.14. Denardo SJ, Messerli FH, Gaxiola E, et al. Coronary revascularization strategy and outcomes according to blood pressure (from the International Verapamil SR-Trandolapril Study [INVEST]). Am J Cardiol. 2010; 106:498–503.15. Dorresteijn JA, van der Graaf Y, Spiering W, et al. Relation between blood pressure and vascular events and mortality in patients with manifest vascular disease: J-curve revisited. Hypertension. 2012; 59:14–21.16. Nissen SE, Tuzcu EM, Libby P, et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT Study: a randomized controlled trial. JAMA. 2004; 292:2217.17. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–2116.18. Witteman JC, Grobbee DE, Valkenburg HA, et al. J-shaped relation between change in diastolic blood pressure and progression of aortic atherosclerosis. Lancet. 1994; 343:504–507.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invasive Treatment of Acute Myocardial Infarction: What is the Optimal Therapy for Acute Myocardial Infarction?
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- Acute Myocardial Infarction Associated with Secondary Hypertension by Renal Juxtaglomerular Cell Tumor
- Acute Closure of Target and Remote Coronary Arteries Complicated by Balloon Rupture during Primary Stenting of Acute Myocardial Infarction
- Primary Coronary Stenting as a Successful Treatment of Acute Myocardial