J Pathol Transl Med.
2017 Sep;51(5):463-470. 10.4132/jptm.2017.05.25.
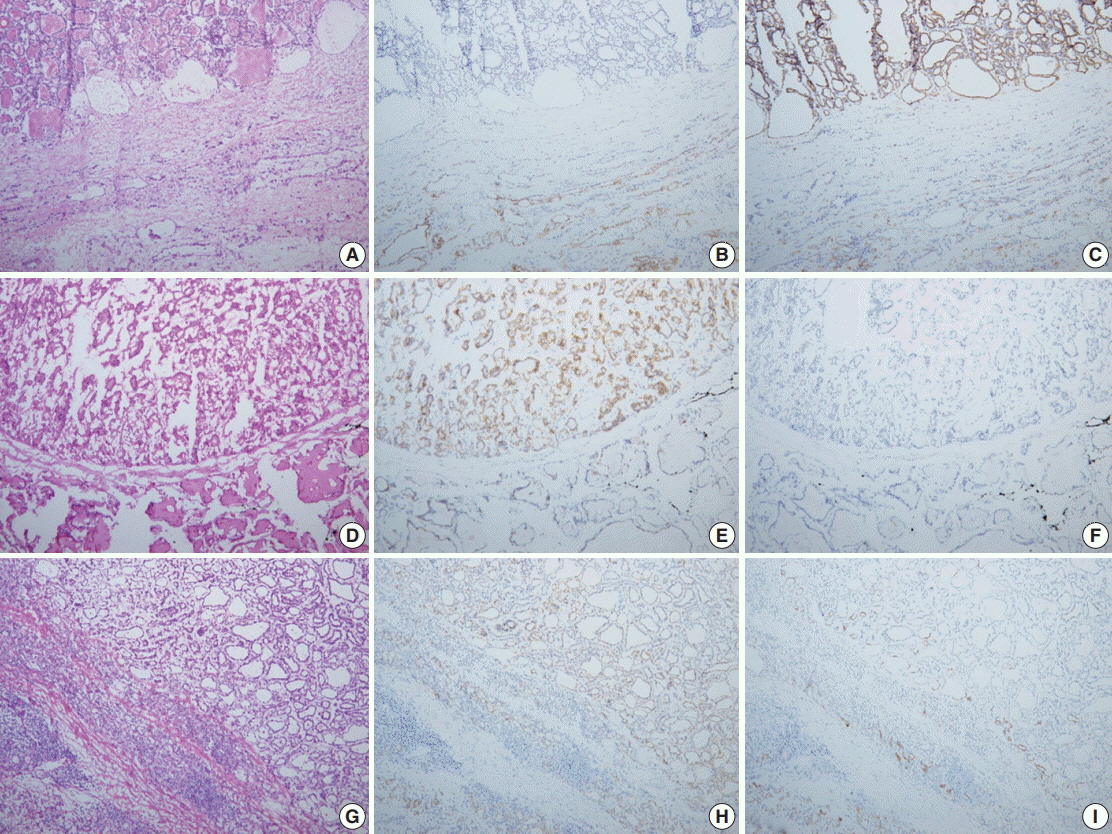
The Intraoperative Immunohistochemical Staining of CD56 and CK19 Improves Surgical Decision for Thyroid Follicular Lesions
- Affiliations
-
- 1Department of Pathology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. soonwonh@yuhs.ac
- 2Department of Pathology, CHA Gangnam Medical Center, CHA University, Seoul, Korea.
- 3Department of Pathology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2392565
- DOI: http://doi.org/10.4132/jptm.2017.05.25
Abstract
- BACKGROUND
When differential diagnosis is difficult in thyroid follicular lesions with overlapping histological features, the immunohistochemical staining can help confirm the diagnosis. We aimed to evaluate the effectiveness of rapid immunohistochemical stains of CD56 and cytokeratin 19 on frozen sections of thyroid follicular lesion and explore the possible gains and limitations of the practice.
METHODS
Eighty-six nodules of 79 patients whose intraoperative frozen sections were selected as the control group, and 53 nodules of 48 patients whose intraoperative frozen sections were subject to rapid immunohistochemistry were selected as the study group.
RESULTS
Five nodules (6%) in the control group were diagnosed as follicular neoplasm and six nodules (7%) were deferred. In the study group, six nodules (11%) were follicular neoplasm and none were deferred. Three nodules (4%) in the control group showed diagnostic discrepancy between the frozen and permanent diagnoses, but none in the study group. The average turnaround time for the frozen diagnosis of the control group was 24 minutes, whereas it was 54 minutes for the study group.
CONCLUSIONS
Intraoperative rapid immunohistochemical stains significantly decreased the diagnostic discrepancy in this study. Considering the adverse effects of indefinite frozen diagnosis or discrepancy with permanent diagnoses, the intraoperative rapid immunohistochemical stain can help to accurately diagnose and hence provide guidance to surgical treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Franssila KO, Ackerman LV, Brown CL, Hedinger CE. Follicular carcinoma. Semin Diagn Pathol. 1985; 2:101–22.2. Posillico SE, Wilhelm SM, McHenry CR. The utility of frozen section examination for determining the extent of thyroidectomy in patients with a thyroid nodule and “atypia/follicular lesion of undetermined significance”. Am J Surg. 2015; 209:552–6.
Article3. Hirokawa M, Carney JA, Goellner JR, et al. Observer variation of encapsulated follicular lesions of the thyroid gland. Am J Surg Pathol. 2002; 26:1508–14.
Article4. Franc B, de la Salmonière P, Lange F, et al. Interobserver and intraobserver reproducibility in the histopathology of follicular thyroid carcinoma. Hum Pathol. 2003; 34:1092–100.
Article5. Lloyd RV, Erickson LA, Casey MB, et al. Observer variation in the diagnosis of follicular variant of papillary thyroid carcinoma. Am J Surg Pathol. 2004; 28:1336–40.
Article6. Elsheikh TM, Asa SL, Chan JK, et al. Interobserver and intraobserver variation among experts in the diagnosis of thyroid follicular lesions with borderline nuclear features of papillary carcinoma. Am J Clin Pathol. 2008; 130:736–44.
Article7. Min HS, Kim JH, Ryoo I, Jung SL, Jung CK. The role of core needle biopsy in the preoperative diagnosis of follicular neoplasm of the thyroid. APMIS. 2014; 122:993–1000.
Article8. Na DG, Kim JH, Sung JY, et al. Core-needle biopsy is more useful than repeat fine-needle aspiration in thyroid nodules read as nondiagnostic or atypia of undetermined significance by the Bethesda system for reporting thyroid cytopathology. Thyroid. 2012; 22:468–75.
Article9. Hakala T, Kholová I, Sand J, Saaristo R, Kellokumpu-Lehtinen P. A core needle biopsy provides more malignancy-specific results than fine-needle aspiration biopsy in thyroid nodules suspicious for malignancy. J Clin Pathol. 2013; 66:1046–50.
Article10. Asa SL. The role of immunohistochemical markers in the diagnosis of follicular-patterned lesions of the thyroid. Endocr Pathol. 2005; 16:295–309.
Article11. El Demellawy D, Nasr A, Alowami S. Application of CD56, P63 and CK19 immunohistochemistry in the diagnosis of papillary carcinoma of the thyroid. Diagn Pathol. 2008; 3:5.
Article12. de Matos LL, Del Giglio AB, Matsubayashi CO, de Lima Farah M, Del Giglio A, da Silva Pinhal MA. Expression of CK-19, galectin-3 and HBME-1 in the differentiation of thyroid lesions: systematic review and diagnostic meta-analysis. Diagn Pathol. 2012; 7:97.
Article13. Nechifor-Boila A, Borda A, Sassolas G, et al. Immunohistochemical markers in the diagnosis of papillary thyroid carcinomas: The promising role of combined immunostaining using HBME-1 and CD56. Pathol Res Pract. 2013; 209:585–92.
Article14. Chem KT, Rosai J. Follicular variant of thyroid papillary carcinoma: a clinicopathologic study of six cases. Am J Surg Pathol. 1977; 1:123–30.15. LiVolsi VA, Baloch ZW. Follicular neoplasms of the thyroid: view, biases, and experiences. Adv Anat Pathol. 2004; 11:279–87.16. Kesmodel SB, Terhune KP, Canter RJ, et al. The diagnostic dilemma of follicular variant of papillary thyroid carcinoma. Surgery. 2003; 134:1005–12.
Article17. Lin HS, Komisar A, Opher E, Blaugrund SM. Follicular variant of papillary carcinoma: the diagnostic limitations of preoperative fine-needle aspiration and intraoperative frozen section evaluation. Laryngoscope. 2000; 110:1431–6.
Article18. Lee IK, Lee HD, Jeong J, et al. Intraoperative examination of sentinel lymph nodes by immunohistochemical staining in patients with breast cancer. Eur J Surg Oncol. 2006; 32:405–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CD56 and High Molecular Weight Cytokeratin as Diagnostic Markers of Papillary Thyroid Carcinoma
- Usefulness of Galectin-3, Cytokeratin 19, p53, and Ki-67 for the Differential Diagnosis of Thyroid Tumors
- Availability of Immunohistochemistry in the Diagnosis of Follicular Variant of Papillary Thyroid Carcinoma
- Diagnostic Value of Galectin-3, HBME-1, Cytokeratin 19, High Molecular Weight Cytokeratin, Cyclin D1 and p27(kip1) in the Differential Diagnosis of Thyroid Nodules
- Immunohistochemical and Molecular Characteristics of Follicular Patterned Thyroid Nodules with Incomplete Nuclear Features of Papillary Thyroid Carcinoma