J Periodontal Implant Sci.
2016 Feb;46(1):10-21. 10.5051/jpis.2016.46.1.10.
Diagnostic accuracy of a combination of salivary hemoglobin levels, self-report questionnaires, and age in periodontitis screening
- Affiliations
-
- 1Department of Preventive Dentistry & Public Oral Health, Yonsei University College of Dentistry, Seoul, Korea. drkbi@yuhs.ac
- 2BK21 PLUS Project, Yonsei University College of Dentistry, Seoul, Korea.
- 3Department of Periodontology, Research Institute for Periodontal Regeneration, Yonsei University College of Dentistry, Seoul, Korea.
- 4Department of Dental Hygiene, Gachon University College of Health Science, Incheon, Korea.
- 5Oral Science Research Institute, Yonsei University College of Dentistry, Seoul, Korea.
- KMID: 2391726
- DOI: http://doi.org/10.5051/jpis.2016.46.1.10
Abstract
- PURPOSE
This study evaluated the predictive performance of a combination of self-report questionnaires, salivary hemoglobin levels, and age as a non-invasive screening method for periodontitis.
METHODS
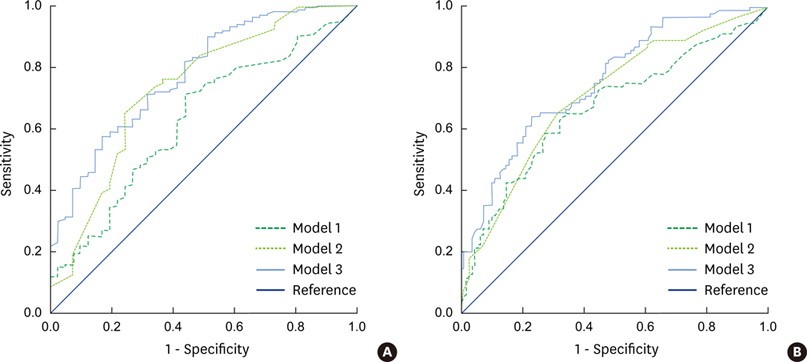
The periodontitis status of 202 adults was examined using salivary hemoglobin levels, responses to 10 questions on a self-report questionnaire, and the Community Periodontal Index (CPI). The ability of those two variables and the combination thereof with age to predict the presence of CPI scores of 3-4 and 4 was assessed using logistic regression and receiver operating characteristic (ROC) curve analysis.
RESULTS
CPI scores of 3-4 and 4 were present among 79.7% and 46.5% of the sample, respectively. The area under the ROC curves (AUROCs) of salivary hemoglobin levels for predicting prevalence of CPI scores of 3-4 and 4 were 0.63 and 0.67, respectively (with sensitivity values of 71% and 60% and specificity values of 56% and 72%, respectively). Two distinct sets of five questions were associated with CPI scores of 3-4 and 4, with AUROCs of 0.73 and 0.71, sensitivity values of 76% and 66%, and specificity values of 63% and 69%. The combined model incorporating both variables and age showed the best predictive performance, with AUROCs of 0.78 and 0.76, sensitivity values of 71% and 65%, and specificity values of 68% and 77% for CPI scores of 3-4 and 4, respectively.
CONCLUSIONS
The combination of salivary hemoglobin levels and self-report questionnaires was shown to be a valuable screening method for detecting periodontitis.
MeSH Terms
Figure
Reference
-
1. Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century--the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003; 31:Suppl 1. 3–23.2. Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe periodontitis in 1990-2010: a systematic review and meta-regression. J Dent Res. 2014; 93:1045–1053.3. Jansson H, Wahlin Å, Johansson V, Åkerman S, Lundegren N, Isberg PE, et al. Impact of periodontal disease experience on oral health-related quality of life. J Periodontol. 2014; 85:438–445.
Article4. Nam SH, Jung HI, Kang SM, Inaba D, Kwon HK, Kim BI. Validity of screening methods for periodontitis using salivary hemoglobin level and self-report questionnaires in people with disabilities. J Periodontol. 2015; 86:536–545.
Article5. Armitage GC. Research, Science and Therapy Committee of the American Academy of Periodontology. Diagnosis of periodontal diseases. J Periodontol. 2003; 74:1237–1247.6. World Health Organization. Oral health surveys: basic methods. 4th ed. Geneva: World Health Organization;1997.7. Page RC, Eke PI. Case definitions for use in population-based surveillance of periodontitis. J Periodontol. 2007; 78:1387–1399.
Article8. Eke PI, Genco RJ. CDC Periodontal Disease Surveillance Project: background, objectives, and progress report. J Periodontol. 2007; 78:1366–1371.
Article9. Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Beck JD, et al. Self-reported measures for surveillance of periodontitis. J Dent Res. 2013; 92:1041–1047.
Article10. Taylor GW, Borgnakke WS. Self-reported periodontal disease: validation in an epidemiological survey. J Periodontol. 2007; 78:1407–1420.
Article11. Miller CS, King CP Jr, Langub MC, Kryscio RJ, Thomas MV. Salivary biomarkers of existing periodontal disease: a cross-sectional study. J Am Dent Assoc. 2006; 137:322–329.12. Gursoy UK, Könönen E, Pradhan-Palikhe P, Tervahartiala T, Pussinen PJ, Suominen-Taipale L, et al. Salivary MMP-8, TIMP-1, and ICTP as markers of advanced periodontitis. J Clin Periodontol. 2010; 37:487–493.
Article13. Polson AM, Caton JG. Current status of bleeding in the diagnosis of periodontal diseases. J Periodontol. 1985; 56:1–3.
Article14. Ramseier CA, Kinney JS, Herr AE, Braun T, Sugai JV, Shelburne CA, et al. Identification of pathogen and host-response markers correlated with periodontal disease. J Periodontol. 2009; 80:436–446.
Article15. Eke PI, Dye B. Assessment of self-report measures for predicting population prevalence of periodontitis. J Periodontol. 2009; 80:1371–1379.
Article16. Slade GD. Interim analysis of validity of periodontitis screening questions in the Australian population. J Periodontol. 2007; 78:1463–1470.
Article17. Christensen GJ. Special oral hygiene and preventive care for special needs. J Am Dent Assoc. 2005; 136:1141–1143.
Article18. Morgan JP, Minihan PM, Stark PC, Finkelman MD, Yantsides KE, Park A, et al. The oral health status of 4,732 adults with intellectual and developmental disabilities. J Am Dent Assoc. 2012; 143:838–846.
Article19. Anders PL, Davis EL. Oral health of patients with intellectual disabilities: a systematic review. Spec Care Dentist. 2010; 30:110–117.
Article20. de Jongh A, van Houtem C, van der Schoof M, Resida G, Broers D. Oral health status, treatment needs, and obstacles to dental care among noninstitutionalized children with severe mental disabilities in The Netherlands. Spec Care Dentist. 2008; 28:111–115.
Article21. Flahault A, Cadilhac M, Thomas G. Sample size calculation should be performed for design accuracy in diagnostic test studies. J Clin Epidemiol. 2005; 58:859–862.
Article22. Kopczyk RA, Graham R, Abrams H, Kaplan A, Matheny J, Jasper SJ. The feasibility and reliability of using a home screening test to detect gingival inflammation. J Periodontol. 1995; 66:52–54.
Article23. Nomura Y, Tamaki Y, Eto A, Kakuta E, Ogino D, Nakamura Y, et al. Screening for periodontal diseases using salivary lactate dehydrogenase, hemoglobin level, and statistical modeling. J Dent Sci. 2012; 7:379–383.
Article24. Greenstein G, Lamster I. Understanding diagnostic testing for periodontal diseases. J Periodontol. 1995; 66:659–666.
Article25. Blicher B, Joshipura K, Eke P. Validation of self-reported periodontal disease: a systematic review. J Dent Res. 2005; 84:881–890.
Article26. Gilbert AD, Nuttall NM. Self-reporting of periodontal health status. Br Dent J. 1999; 186:241–244.
Article27. Gilbert GH, Litaker MS. Validity of self-reported periodontal status in the Florida dental care study. J Periodontol. 2007; 78:1429–1438.
Article28. Kibayashi M, Tanaka M, Nishida N, Kuboniwa M, Kataoka K, Nagata H, et al. Longitudinal study of the association between smoking as a periodontitis risk and salivary biomarkers related to periodontitis. J Periodontol. 2007; 78:859–867.
Article29. Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III. J Periodontol. 2000; 71:743–751.
Article30. Han DH, Lim S, Kim JB. The association of smoking and diabetes with periodontitis in a Korean population. J Periodontol. 2012; 83:1397–1406.
Article31. Dye BA. Global periodontal disease epidemiology. Periodontol 2000. 2012; 58:10–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Salivary soluble receptor activator of nuclear factor kappa B ligand/osteoprotegerin ratio in periodontal disease and health
- Analysis of Periodontitis Biomarker Expression in Gingival Crevicular Fluids
- Changes in the components of salivary exosomes due to initial periodontal therapy
- Usefulness of the Berlin, STOP, and STOP-Bang Questionnaires in the Diagnosis of Obstructive Sleep Apnea
- Comparative Evaluation of Salivary Neopterin Levels and Its Effects to Periodontal Therapy in Pre- and Post-Menopausal Women