Ann Rehabil Med.
2012 Oct;36(5):675-680.
Extracorporeal Shock Wave Therapy in Myofascial Pain Syndrome of Upper Trapezius
- Affiliations
-
- 1Department of Rehabilitation Medicine, School of Medicine, Ewha Womans University, Seoul 158-710, Korea. ocrystal@ewha.ac.kr
Abstract
OBJECTIVE
To evaluate the effect of extracorporeal shock wave therapy (ESWT) in myofascial pain syndrome of upper trapezius with visual analogue scale (VAS) and pressure threshold by digital algometer. METHOD: Twenty-two patients diagnosed with myofascial pain syndrome in upper trapezius were selected. They were assigned to treatment and standard care (control) groups balanced by age and sex, with eleven subjects in each group. The treated group had done four sessions of ESWT (0.056 mJ/mm2, 1,000 impulses, semiweekly) while the control group was treated by the same protocol but with different energy levels applied, 0.001 mJ/mm2. The VAS and pressure threshold were measured twice: before and after last therapy. We evaluated VAS of patients and measured the pressure threshold by using algometer.
RESULTS
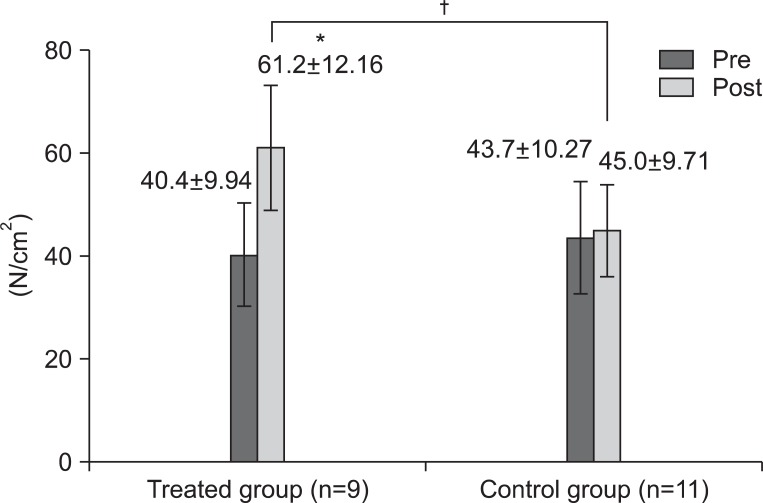
There were two withdrawals and the remaining 20 patients were three men and 17 women. Age was distributed with 11 patients in their twenties and 9 over 30 years old. There was no significant difference of age, sex, pre-VAS and pre-pressure threshold between 2 groups (p>0.05) found. The VAS significantly decreased from 4.91+/-1.76 to 2.27+/-1.27 in the treated group (p<0.01). The control group did not show any significant changes of VAS score. The pressure threshold significantly increased from 40.4+/-9.94 N to 61.2+/-12.16 N in the treated group (p<0.05), but there was no significant change in the control group.
CONCLUSION
ESWT in myofascial pain syndrome of upper trapezius is effective to relieve pain after four times therapies in two weeks. But further study will be required with more patients, a broader age range and more males.
Keyword
Figure
Reference
-
1. Sciotti VM, Mittak VL, DiMarco L, Ford LM, Plezbert J, Santipadri E, Wigglesworth J, Ball K. Clinical precision of myofascial trigger point location in the trapezius muscle. Pain. 2001; 93:259–266. PMID: 11514085.
Article2. Wade B. Trigger points in the upper trapezius or normal subtrapezial anatomy? Physiother Can. 2001; 53:219–222.3. Fischer AA. Pressure algometry over normal muscles. Standard valuses, validity and reproducibility of pressure threshold. Pain. 1987; 30:115–126. PMID: 3614975.4. Simons DG, Travell JG, Simons LS. Myofascial pain and dysfunction: upper half of body. 1999. 2nd ed. Baltimore: Lippincott Williams & Wilkins;p. 69–86.5. Borg-Stein J, Simons DG. Focused review: myofascial pain. Arch Phys Med Rehabil. 2002; 83:S40–S47. PMID: 11973695.6. Bennet R. Myofascial pain syndromes and their evaluation. Best Pract Clin Rheumatol. 2007; 21:427–445.7. De las Penas CF, Campo MS, Carnero JF, Miangolarra Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. J Bodyw Mov Ther. 2005; 9:27–34.8. Rickards LD. The effectiveness of non-invasive treatments for active myofascial trigger point pain: a systematic review of the literature. Int J Osteopath Med. 2006; 9:120–136.
Article9. Simons DG. Myofascial pain and dysfunction syndrome. J Muscoskel Pain. 1993; 1:123–132.
Article10. Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2009; 13:3–10. PMID: 18395479.11. Müller-Ehrenberg H, Licht G. Diagnosis and therapy of myofascial pain syndrome with focused shock waves (ESWT). Med Orthop Tech. 2005; 5:1–6.12. Bauermeister W. Diagnosis and therapy of myofascial trigger point syndrome through stimulation of sensitized nociceptors using focused electrohydraulic shockwaves. Med Orthop Tech. 2005; 5:65–74.13. Liang HW, Wang TG, Chen WS, Hou SM. Thinner plantar fascia predicts decreased pain after extracorporeal shock wave therapy. Clin Orthop Relat Res. 2007; 460:219–225. PMID: 17353798.
Article14. Hammer DS, Adam F, Kreutz A, Rupp S, Kohn D, Seil R. Ultrasonographic evaluation at 6-month follow-up of plantar fasciitis after extracorporeal shock wave therapy. Arch Orthop Trauma Surg. 2005; 125:6–9. PMID: 14530990.
Article15. Wang FS, Yang KD, Chen RF, Wang CJ, Sheen-Chen SM. Extracoporeal shock wave promotes growth and differentiation of bone-marrow stromal cells towards osteoprogenitors associated with induction of TGF-beta1. J Bone Joint Surg Br. 2002; 84:457–461. PMID: 12002511.16. Shah JP, Danoff JV, Desai MJ, Parikh S, Nakamura LY, Phillips TM, Gerber LH. Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Arch Phys Med Rehabil. 2008; 89:16–23. PMID: 18164325.
Article17. Ottomann C, Hartmann B, Tyler J, Maier H, Thiele R, Schaden W, Stojadinovic A. Prospective randomized trial of accelerated re-epithelization of skin graft donor sites using extracorporeal shock wave therapy. J Am Coll Surg. 2010; 211:361–367. PMID: 20800193.
Article18. Rompe JD, Hope C, Küllmer K, Heine J, Bürger R. Analgesic effect of extracorporeal shock-wave therapy on chronic tennis elbow. J Bone Joint Surg Br. 1996; 78:233–237. PMID: 8666632.
Article19. Han TR, Kim JH, Paik NJ, Lim SJ. Importance of local twitch response induced by needling in myofascial pain syndrome. J Korean Acad Rehabil Med. 1999; 23:595–600.20. Rompe JD, Meuer A, Nafe B, Hofmann A, Gerdesmeyer L. Repetitive low-energy shock wave application without local anesthesia is more efficient than repetitive low-energy shock wave application with local anesthesia in the treatment of chronic plantar fascitits. J Orthop Res. 2005; 23:931–941. PMID: 16023010.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Results of Radial and Focused Extracorporeal Shockwave Therapy on Periscapular Myofascial Pain Syndrome
- Extracorporeal Shock Wave Therapy Versus Trigger Point Injection in the Treatment of Myofascial Pain Syndrome in the Quadratus Lumborum
- The Effect of Extracorporeal Shock Wave Therapy on Myofascial Pain Syndrome
- Feasibility of Extracorporeal Shock Wave Therapy for Complex Upper Limb Morbidity in Breast Cancer Patient
- Treatment Experience of Pulsed Radiofrequency Under Ultrasound Guided to the Trapezius Muscle at Myofascial Pain Syndrome: A Case Report