Blood Res.
2017 Sep;52(3):200-206. 10.5045/br.2017.52.3.200.
Platelet to lymphocyte ratio (PLR) retains independent prognostic significance in advanced stage marginal zone lymphoma patients treated with rituximab, cyclophosphamide, vincristine, and prednisone combination chemotherapy (R-CVP): Consortium for Improving Survival of Lymphoma trial
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University Hospital, Busan, Korea. drosy@dau.ac.kr
- 2Department of Medicine, Samsung Medical Center, Sunkyunkwan University School of Medicine, Seoul, Korea.
- 3Division of Hematology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Division of Hematology and Oncology, Department of Internal Medicine, Gachon University Gil Hospital, Incheon, Korea.
- 5Division of Hematology-Oncology, Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University College of Medicine, Jinju, Korea.
- 6Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. csuh@amc.seoul.kr
- 7Department of Hemato/Oncology, Busan Paik Hospital, College of Medicine, Inje University, Busan, Korea.
- 8Department of Internal Medicine, Hallym Medical Center, Hallym University College of Medicine, Anyang, Korea.
- 9Division of Hematology, Department of Internal Medicine, Chonbuk National University Medical School, Jeonju, Korea.
- 10Division of Hematology/Oncology, Department of Internal Medicine, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea.
- 11Department of Hematology and Oncology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 12Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 13Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea.
- KMID: 2390982
- DOI: http://doi.org/10.5045/br.2017.52.3.200
Abstract
- BACKGROUND
Rituximab plus cyclophosphamide, vincristine, and prednisone (R-CVP) is one of the effective chemotherapeutic regimens for patients with advanced stage marginal zone lymphoma (MZL). However, prognostic factors that affect the outcome of treatment for MZL are not well understood.
METHODS
Between August 2006 and June 2013, patients with newly diagnosed stage III and IV MZL treated with R-CVP as a first-line therapy from 15 institutions were retrospectively analyzed. Patients' clinical and laboratory data at diagnosis were collected by review of medical records.
RESULTS
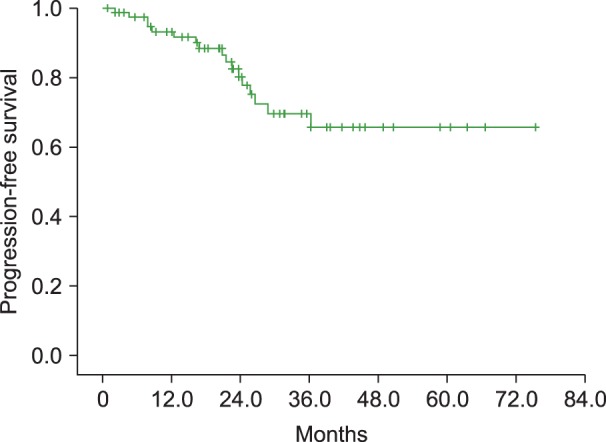
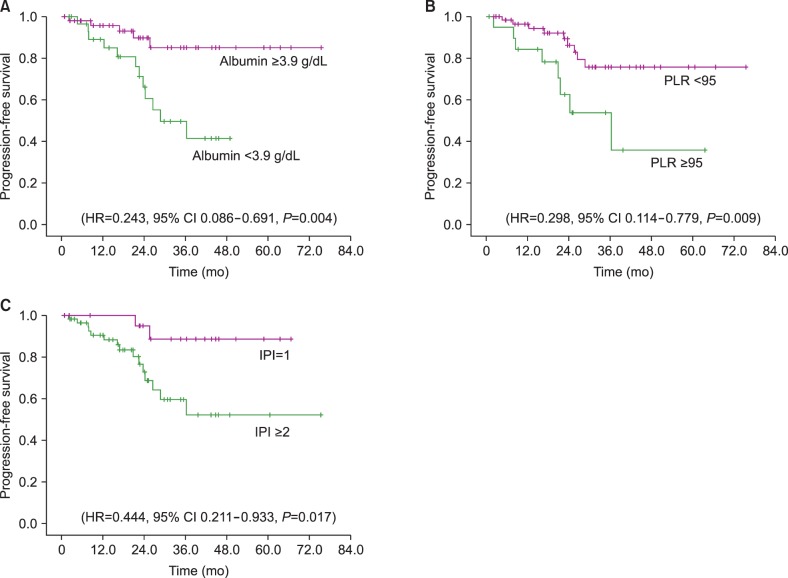
A total of 80 patients were analyzed. Bone marrow involvement was observed in 30% cases. Twelve patients (15%) had nodal MZL, and 41.3% patients exhibited multiple mucosa-associated lymphoma tissue sites. Overall response rate was 91.3%, including 73.8% achieving complete response. Advanced MZL patients treated with R-CVP showed a 3-year progression-free survival (PFS) rate of 69.6%. Prognostic markers significantly affecting PFS in univariate analysis were platelet to lymphocyte ratio (PLR, <95 vs. ≥95, P=0.014), serum albumin (≤3.9 vs. >3.9 g/dL, P=0.008), and the International Prognostic Index (IPI) score (1 vs. 2-4, P=0.032). In multivariate analysis, only PLR (<95 vs. ≥95, HR 0.367, 95% CI, 0.139-0.971, P=0.043) was an independent risk factor for PFS.
CONCLUSION
PLR ≥95 at diagnosis is an independent prognostic marker for PFS in advanced stage MZL patients treated with R-CVP. This marker may aid clinicians in predicting the response to R-CVP chemotherapy in stage III and IV MZL patients.
Keyword
MeSH Terms
-
Blood Platelets*
Bone Marrow
Cyclophosphamide*
Diagnosis
Disease-Free Survival
Drug Therapy
Drug Therapy, Combination*
Humans
Lymphocytes*
Lymphoma*
Medical Records
Multivariate Analysis
Prednisone*
Prognosis
Retrospective Studies
Risk Factors
Rituximab*
Serum Albumin
Vincristine*
Cyclophosphamide
Prednisone
Rituximab
Serum Albumin
Vincristine
Figure
Cited by 1 articles
-
Organ-specific considerations for marginal zone lymphomas in Korea, based on Consortium for Improving Survival of Lymphoma (CISL) and Korean clinical studies
Sung Yong Oh, Cheolwon Suh
Blood Res. 2019;54(1):4-6. doi: 10.5045/br.2019.54.1.4.
Reference
-
1. Oh SY, Ryoo BY, Kim WS, et al. Nongastric marginal zone B-cell lymphoma: analysis of 247 cases. Am J Hematol. 2007; 82:446–452. PMID: 17266060.
Article2. Kim JM, Ko YH, Lee SS, et al. WHO classification of malignant lymphomas in Korea: report of the third nationwide study. Korean J Pathol. 2011; 45:254–260.
Article3. Conconi A, Martinelli G, Thiéblemont C, et al. Clinical activity of rituximab in extranodal marginal zone B-cell lymphoma of MALT type. Blood. 2003; 102:2741–2745. PMID: 12842999.
Article4. Oh SY, Kim WS, Kim JS, et al. Stage IV marginal zone B-cell lymphoma--prognostic factors and the role of rituximab: Consortium for Improving Survival of Lymphoma (CISL) study. Cancer Sci. 2010; 101:2443–2447. PMID: 20831770.5. Zucca E, Conconi A, Laszlo D, et al. Addition of rituximab to chlorambucil produces superior event-free survival in the treatment of patients with extranodal marginal-zone B-cell lymphoma: 5-year analysis of the IELSG-19 Randomized Study. J Clin Oncol. 2013; 31:565–572. PMID: 23295789.6. Kang HJ, Kim WS, Kim SJ, et al. Phase II trial of rituximab plus CVP combination chemotherapy for advanced stage marginal zone lymphoma as a first-line therapy: Consortium for Improving Survival of Lymphoma (CISL) study. Ann Hematol. 2012; 91:543–551. PMID: 21922208.
Article7. International Non-Hodgkin's Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin's lymphoma. N Engl J Med. 1993; 329:987–994. PMID: 8141877.8. López-Guillermo A, Montserrat E, Bosch F, Terol MJ, Campo E, Rozman C. Applicability of the International Index for aggressive lymphomas to patients with low-grade lymphoma. J Clin Oncol. 1994; 12:1343–1348. PMID: 8021724.
Article9. Oh SY, Kwon HC, Kim WS, et al. Nongastric marginal zone B-cell lymphoma: a prognostic model from a retrospective multicenter study. Cancer Lett. 2007; 258:90–97. PMID: 17936499.
Article10. Li YJ, Jiang WQ, Huang JJ, Xia ZJ, Huang HQ, Li ZM. The Glasgow Prognostic Score (GPS) as a novel and significant predictor of extranodal natural killer/T-cell lymphoma, nasal type. Am J Hematol. 2013; 88:394–399. PMID: 23423859.
Article11. Heilgeist A, McClanahan F, Ho AD, Witzens-Harig M. Prognostic value of the Follicular Lymphoma International Prognostic Index score in marginal zone lymphoma: an analysis of clinical presentation and outcome in 144 patients. Cancer. 2013; 119:99–106. PMID: 22736411.12. Ngo L, Hee SW, Lim LC, et al. Prognostic factors in patients with diffuse large B cell lymphoma: Before and after the introduction of rituximab. Leuk Lymphoma. 2008; 49:462–469. PMID: 18297522.
Article13. Kokcu A, Kurtoglu E, Celik H, Tosun M, Malatyalıoglu E, Ozdemir AZ. May the platelet to lymphocyte ratio be a prognostic factor for epithelial ovarian cancer? Asian Pac J Cancer Prev. 2014; 15:9781–9784. PMID: 25520104.
Article14. Sun W, Zhang L, Luo M, et al. Pretreatment hematologic markers as prognostic factors in patients with nasopharyngeal carcinoma: Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Head Neck. 2016; 38(Suppl 1):E1332–E1340. PMID: 26362911.
Article15. Dalia S, Chavez J, Little B, et al. Serum albumin retains independent prognostic significance in diffuse large B-cell lymphoma in the post-rituximab era. Ann Hematol. 2014; 93:1305–1312. PMID: 24590536.
Article16. Raungkaewmanee S, Tangjitgamol S, Manusirivithaya S, Srijaipracharoen S, Thavaramara T. Platelet to lymphocyte ratio as a prognostic factor for epithelial ovarian cancer. J Gynecol Oncol. 2012; 23:265–273. PMID: 23094130.
Article17. Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010; 140:883–899. PMID: 20303878.
Article18. Sharma D, Brummel-Ziedins KE, Bouchard BA, Holmes CE. Platelets in tumor progression: a host factor that offers multiple potential targets in the treatment of cancer. J Cell Physiol. 2014; 229:1005–1015. PMID: 24374897.
Article19. Ray-Coquard I, Cropet C, Van Glabbeke M, et al. Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res. 2009; 69:5383–5391. PMID: 19549917.
Article20. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002; 420:860–867. PMID: 12490959.
Article21. Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010; 9:69. PMID: 21176210.
Article22. Cannon NA, Meyer J, Iyengar P, et al. Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non-small-cell lung cancer. J Thorac Oncol. 2015; 10:280–285. PMID: 25299234.
Article23. Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011; 104:1288–1295. PMID: 21448173.
Article24. Porrata LF, Ristow K, Habermann TM, et al. Absolute monocyte/lymphocyte count prognostic score is independent of immunohistochemically determined cell of origin in predicting survival in diffuse large B-cell lymphoma. Leuk Lymphoma. 2012; 53:2159–2165. PMID: 22551474.
Article25. Porrata LF, Ristow K, Habermann TM, Witzig TE, Inwards DJ, Markovic SN. Absolute lymphocyte count at the time of first relapse predicts survival in patients with diffuse large B-cell lymphoma. Am J Hematol. 2009; 84:93–97. PMID: 19123458.
Article26. Chae YS, Shin H, Sohn SK, et al. Absolute lymphocyte count at day + 21 predicts survival in patients with early-stage diffuse large B-cell lymphoma treated with rituximab, cyclophosphamide, adriamycin, vincristine and prednisone. Leuk Lymphoma. 2012; 53:1757–1763. PMID: 22372848.27. Aoki K, Tabata S, Yonetani N, Matsushita A, Ishikawa T. The prognostic impact of absolute lymphocyte and monocyte counts at diagnosis of diffuse large B-cell lymphoma in the rituximab era. Acta Haematol. 2013; 130:242–246. PMID: 23860478.
Article28. Ho CL, Lu CS, Chen JH, Chen YG, Huang TC, Wu YY. Neutrophil/lymphocyte ratio, lymphocyte/monocyte ratio, and absolute lymphocyte count/absolute monocyte count prognostic score in diffuse large b-cell lymphoma: useful prognostic tools in the rituximab era. Medicine (Baltimore). 2015; 94:e993. PMID: 26091479.29. Romano A, Parrinello NL, Consoli ML, et al. Neutrophil to lymphocyte ratio (NLR) improves the risk assessment of ISS staging in newly diagnosed MM patients treated upfront with novel agents. Ann Hematol. 2015; 94:1875–1883. PMID: 26223359.
Article30. Kharfan-Dabaja MA, Chavez JC, Yu D, et al. Severe hypoalbuminemia at day 90 predicts worse nonrelapse mortality and overall survival after allogeneic hematopoietic stem cell transplantation for acute myelogenous leukemia and myelodysplastic syndrome. Biol Blood Marrow Transplant. 2011; 17:384–393. PMID: 20655389.
Article31. Komrokji RS, Corrales-Yepez M, Kharfan-Dabaja MA, et al. Hypoalbuminemia is an independent prognostic factor for overall survival in myelodysplastic syndromes. Am J Hematol. 2012; 87:1006–1009. PMID: 23090887.
Article32. Mazloom A, Medeiros LJ, McLaughlin PW, et al. Marginal zone lymphomas: factors that affect the final outcome. Cancer. 2010; 116:4291–4298. PMID: 20549822.33. Arcaini L, Burcheri S, Rossi A, et al. Nongastric marginal-zone B-cell MALT lymphoma: prognostic value of disease dissemination. Oncologist. 2006; 11:285–291. PMID: 16549813.
Article34. Arcaini L, Lazzarino M, Colombo N, et al. Splenic marginal zone lymphoma: a prognostic model for clinical use. Blood. 2006; 107:4643–4649. PMID: 16493005.
Article35. Bambace NM, Holmes CE. The platelet contribution to cancer progression. J Thromb Haemost. 2011; 9:237–249. PMID: 21040448.
Article36. Trikha M, Zhou Z, Timar J, et al. Multiple roles for platelet GPIIb/IIIa and alphavbeta3 integrins in tumor growth, angiogenesis, and metastasis. Cancer Res. 2002; 62:2824–2833. PMID: 12019160.37. Leslie M. Cell biology. Beyond clotting: the powers of platelets. Science. 2010; 328:562–564. PMID: 20430990.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Rituximab, Cyclophosphamide, Vincristine, and Prednisolone (R-CVP) Chemotherapy in Patients with Ocular Adnexal Extranodal Marginal Zone B Cell Lymphoma of the Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma
- A Case of Lacrimal Gland MALT Lymphoma in a Patient with Primary Sjögren's Syndrome
- Primary diffuse large B-cell lymphoma of the bone marrow in a frail and elderly patient successfully treated with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone
- Primary Marginal Zone B-cell Lymphoma of Mucosa-associated Lymphoid Tissue of the Lacrimal Sac Mimicking Dacryocystitis
- Clinicopathologic significance of tumor microenvironment CD11c, and FOXP3 expression in diffuse large B-cell lymphoma patients receiving rituximab, cyclophosphamide, anthracycline, vincristine, and prednisone (R-CHOP) combination chemotherapy