Ann Hepatobiliary Pancreat Surg.
2017 Aug;21(3):122-130. 10.14701/ahbps.2017.21.3.122.
Mirizzi syndrome: necessity for safe approach in dealing with diagnostic and treatment challenges
- Affiliations
-
- 1King Abdullah International Medical Research Center / King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia. shirah007@ksau-hs.edu.sa
- 2Department of General Surgery, Al Ansar General Hospital, Medina, Saudi Arabia.
- 3King Abdulaziz Medical City/King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia.
- KMID: 2389988
- DOI: http://doi.org/10.14701/ahbps.2017.21.3.122
Abstract
- BACKGROUNDS/AIMS
The challenging dilemma of Mirizzi syndrome for operating surgeons arises from the difficulty to diagnose it preoperatively, and approximately 50% of cases are diagnosed intraoperatively. In this study, we analysed the effectiveness of diagnostic modalities and treatment options in our series of Mirizzi syndrome.
METHODS
Patients had a preoperative or intraoperative diagnosis of Mirizzi syndrome, and were classified into three groups: Group 1: Incidental finding of Mirizzi syndrome intraoperatively (n=34). Group 2: Patients presented with jaundice, diagnosed by endoscopic retrograde cholangiopancreatography (n=17). Group 3: Patients diagnosed initially by ultrasound (n=13). Laparoscopic cholecystectomy was conducted in all 49 patients with Cendes type I disease. Partial cholecystectomy, common bile duct exploration, repair of fistula and t-tube placement was conducted on eight patients with Cendes type II and five patients with Cendes type III. Partial cholecystectomy with Roux-en-Y hepaticojejunostomy was conducted in two patients with Cendes type IV disease.
RESULTS
Sixty-four patients were diagnosed with Mirizzi syndrome. Morbidity rate was 3.1%. Mortality rate was 0%. Group 3 (patients diagnosed initially by ultrasound) had the best treatment outcome, the least morbidity, and the shortest hospital stay.
CONCLUSIONS
Suspected cases of Mirizzi syndrome should not be underestimated. Difficulty in establishing preoperative diagnosis is the major dilemma. As it is mostly encountered intraoperatively, the approach should be careful and logical to identify the correct type of Mirizzi by a thorough diagnostic laparoscopy and thus, provide optimum treatment for the subtype to achieve the best outcome.
Keyword
MeSH Terms
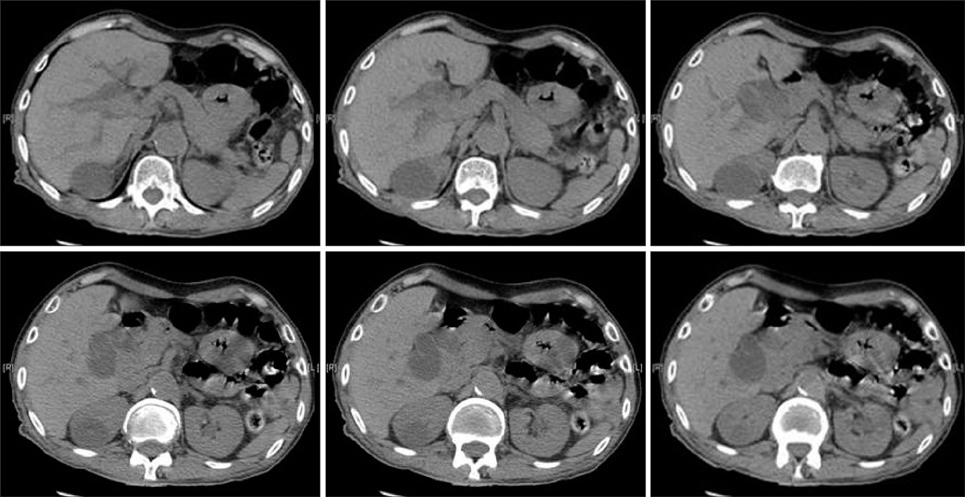
Figure
Reference
-
1. Elhanafy E, Atef E, El Nakeeb A, Hamdy E, Elhemaly M, Sultan AM. Mirizzi syndrome: How it could be a challenge. Hepatogastroenterology. 2014; 61:1182–1186.2. Johnson LW, Sehon JK, Lee WC, Zibari GB, McDonald JC. Mirizzi's syndrome: experience from a multi-institutional review. Am Surg. 2001; 67:11–14.3. Chan CY, Liau KH, Ho CK, Chew SP. Mirizzi syndrome: a diagnostic and operative challenge. Surgeon. 2003; 1:273–278.4. Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002; 97:249–254.5. Bedirli A, Kerem M, Bostanci H, Karakan T, Sahin TT, Akyurek N. Coexistence of Mirizzi syndrome with adenomyomatosis in the gallbladder: report of a case. Hepatobiliary Pancreat Dis Int. 2007; 6:438–441.6. Beltran MA, Csendes A. Mirizzi syndrome and gallstone ileus: an unusual presentation of gallstone disease. J Gastrointest Surg. 2005; 9:686–689.7. Al-Akeely MH, Alam MK, Bismar HA, Khalid K, Al-Teimi I, Al-Dossary NF. Mirizzi syndrome: ten years experience from a teaching hospital in Riyadh. World J Surg. 2005; 29:1687–1692.8. Karakoyunlar O, Sivrel E, Koc O, Denecli AG. Mirizzi's syndrome must be ruled out in the differential diagnosis of any patients with obstructive jaundice. Hepatogastroenterology. 1999; 46:2178–2182.9. Yonetci N, Kutluana U, Yilmaz M, Sungurtekin U, Tekin K. The incidence of Mirizzi syndrome in patients undergoing endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2008; 7:520–524.10. Zhong H, Gong JP. Mirizzi syndrome: experience in diagnosis and treatment of 25 cases. Am Surg. 2012; 78:61–65.11. Csendes A, Díaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989; 76:1139–1143.12. Beltrán MA. Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol. 2012; 18:4639–4650.13. Waisberg J, Corona A, de Abreu IW, Farah JF, Lupinacci RA, Goffi FS. Benign obstruction of the common hepatic duct (Mirizzi syndrome): diagnosis and operative management. Arq Gastroenterol. 2005; 42:13–18.14. Lai EC, Lau WY. Mirizzi syndrome: history, present and future development. ANZ J Surg. 2006; 76:251–257.15. Kamalesh NP, Prakash K, Pramil K, George TD, Sylesh A, Shaji P. Laparoscopic approach is safe and effective in the management of Mirizzi syndrome. J Minim Access Surg. 2015; 11:246–250.16. Hubert C, Annet L, van Beers BE, Gigot JF. The "inside approach of the gallbladder" is an alternative to the classic Calot's triangle dissection for a safe operation in severe cholecystitis. Surg Endosc. 2010; 24:2626–2632.17. Kwon AH, Inui H. Preoperative diagnosis and efficacy of laparoscopic procedures in the treatment of Mirizzi syndrome. J Am Coll Surg. 2007; 204:409–415.18. Beltran MA, Csendes A, Cruces KS. The relationship of Mirizzi syndrome and cholecystoenteric fistula: validation of a modified classification. World J Surg. 2008; 32:2237–2243.19. Safioleas M, Stamatakos M, Safioleas P, Smyrnis A, Revenas C, Safioleas C. Mirizzi syndrome: an unexpected problem of cholelithiasis. Our experience with 27 cases. Int Semin Surg Oncol. 2008; 5:12.20. Gomez D, Rahman SH, Toogood GJ, Prasad KR, Lodge JP, Guillou PJ, et al. Mirizzi's syndrome--results from a large western experience. HPB (Oxford). 2006; 8:474–479.21. Karademir S, Astarcioğlu H, Sökmen S, Atila K, Tankurt E, Akpinar H, et al. Mirizzi's syndrome: diagnostic and surgical considerations in 25 patients. J Hepatobiliary Pancreat Surg. 2000; 7:72–77.22. Tan KY, Chng HC, Chen CY, Tan SM, Poh BK, Hoe MN. Mirizzi syndrome: noteworthy aspects of a retrospective study in one centre. ANZ J Surg. 2004; 74:833–837.23. Schäfer M, Schneiter R, Krähenbühl L. Incidence and management of Mirizzi syndrome during laparoscopic cholecystectomy. Surg Endosc. 2003; 17:1186–1190.24. Lledó JB, Barber SM, Ibañez JC, Torregrosa AG, Lopez-Andujar R. Update on the diagnosis and treatment of mirizzi syndrome in laparoscopic era: our experience in 7 years. Surg Laparosc Endosc Percutan Tech. 2014; 24:495–501.25. Prasad TL, Kumar A, Sikora SS, Saxena R, Kapoor VK. Mirizzi syndrome and gallbladder cancer. J Hepatobiliary Pancreat Surg. 2006; 13:323–326.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mirizzi Syndrome-Diagnostic Dilemma for Surgeons
- Mirizzi syndrome: one case report
- Laparoscopic treatment for post-cholecystectomy Mirizzi syndrome
- Two Cases of the Endoscopic Treatment of Type I Mirizzi Syndrome
- Laparoscopic management of Mirizzi syndrome with liver cirrhosis using indocyanine green mapping: A case report and review of the literature