J Breast Cancer.
2017 Jun;20(2):176-182. 10.4048/jbc.2017.20.2.176.
The Usefulness of Intraoperative Circumferential Frozen-Section Analysis of Lumpectomy Margins in Breast-Conserving Surgery
- Affiliations
-
- 1Department of Surgery, Cheil General Hospital & Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Cheil General Hospital & Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea.
- 3Department of Surgery, Inha University Hospital, Inha University School of Medicine, Incheon, Korea. hmh1916@gmail.com
- KMID: 2389755
- DOI: http://doi.org/10.4048/jbc.2017.20.2.176
Abstract
- PURPOSE
Intraoperative frozen-section analysis of the lumpect-omy margin during breast-conserving surgery (BCS) is an excellent method in obtaining a clear resection margin. This study aimed to investigate the usefulness of intraoperative circumferential frozen-section analysis (IOCFS) of lumpectomy margin during BCS for breast cancer, and to find factors that increase the conversion into mastectomy.
METHODS
From 2007 to 2011, 509 patients with breast cancer underwent IOCFS during BCS. The outer surfaces of the shaved lumpectomy margins were evaluated. A negative margin was defined as no ink on the tumor. All margins were evaluated using the permanent section analysis.
RESULTS
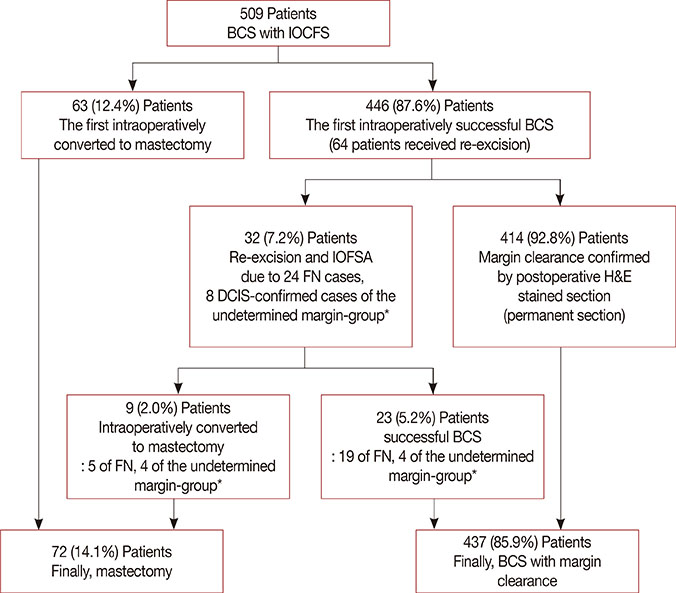
Among the 509 patients, 437 (85.9%) underwent BCS and 72 (14.1%) finally underwent mastectomy. Of the 483 pathologically confirmed patients, 338 (70.0%) were true-negative, 24 (5.0%) false-negative, 120 (24.8%) true-positive, and 1 (0.2%) false-positive. Twenty-four patients (4.7%) among total 509 patients had undetermined margins as either atypical ductal hyperplasia or ductal carcinoma in situ in the first IOCFS. The IOCFS has an accuracy of 94.8% with 83% sensitivity, 99.7% specificity, 93.4% negative predictive value, and 99.2% positive predictive value. Sixty-three cases (12.4%) were converted to mastectomy, the first intraoperatively. Of the 446 (87.6%) patients who successfully underwent BCS, 64 patients received additional excisions and 32 were reoperated to achieve clear margin (reoperation rate, 6.3%). Twenty-three of the reoperated patients underwent re-excisions using the second intraoperative frozen section analysis, and achieved BCS. Nine cases were additionally converted to mastectomy. No significant differences in age, stage, and biological factors were found between the BCS and mastectomy cases. Factors such as invasive lobular carcinoma, multiple tumors, large tumor, and multiple excisions increased the conversion to mastectomy.
CONCLUSION
The IOCFS analysis during BCS is useful in evaluating lumpectomy margins and preventing reoperation.
MeSH Terms
Figure
Reference
-
1. van Dongen JA, Voogd AC, Fentiman IS, Legrand C, Sylvester RJ, Tong D, et al. Long-term results of a randomized trial comparing breast-conserving therapy with mastectomy: European Organization for Research and Treatment of Cancer 10801 trial. J Natl Cancer Inst. 2000; 92:1143–1150.
Article2. Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002; 347:1233–1241.
Article3. Gage I, Schnitt SJ, Nixon AJ, Silver B, Recht A, Troyan SL, et al. Pathologic margin involvement and the risk of recurrence in patients treated with breast-conserving therapy. Cancer. 1996; 78:1921–1928.
Article4. Leong C, Boyages J, Jayasinghe UW, Bilous M, Ung O, Chua B, et al. Effect of margins on ipsilateral breast tumor recurrence after breast conservation therapy for lymph node-negative breast carcinoma. Cancer. 2004; 100:1823–1832.
Article5. Schnitt SJ, Abner A, Gelman R, Connolly JL, Recht A, Duda RB, et al. The relationship between microscopic margins of resection and the risk of local recurrence in patients with breast cancer treated with breast-conserving surgery and radiation therapy. Cancer. 1994; 74:1746–1751.
Article6. Smitt MC, Nowels KW, Zdeblick MJ, Jeffrey S, Carlson RW, Stockdale FE, et al. The importance of the lumpectomy surgical margin status in long-term results of breast conservation. Cancer. 1995; 76:259–267.
Article7. Aziz D, Rawlinson E, Narod SA, Sun P, Lickley HL, McCready DR, et al. The role of reexcision for positive margins in optimizing local disease control after breast-conserving surgery for cancer. Breast J. 2006; 12:331–337.
Article8. Talsma AK, Reedijk AM, Damhuis RA, Westenend PJ, Vles WJ. Re-resection rates after breast-conserving surgery as a performance indicator: introduction of a case-mix model to allow comparison between Dutch hospitals. Eur J Surg Oncol. 2011; 37:357–363.
Article9. Jacobson AF, Asad J, Boolbol SK, Osborne MP, Boachie-Adjei K, Feldman SM. Do additional shaved margins at the time of lumpectomy eliminate the need for re-excision? Am J Surg. 2008; 196:556–558.
Article10. Thill M, Baumann K, Barinoff J. Intraoperative assessment of margins in breast conservative surgery: still in use? J Surg Oncol. 2014; 110:15–20.
Article11. Cabioglu N, Hunt KK, Sahin AA, Kuerer HM, Babiera GV, Singletary SE, et al. Role for intraoperative margin assessment in patients undergoing breast-conserving surgery. Ann Surg Oncol. 2007; 14:1458–1471.
Article12. Camp ER, McAuliffe PF, Gilroy JS, Morris CG, Lind DS, Mendenhall NP, et al. Minimizing local recurrence after breast conserving therapy using intraoperative shaved margins to determine pathologic tumor clearance. J Am Coll Surg. 2005; 201:855–861.
Article13. Cao D, Lin C, Woo SH, Vang R, Tsangaris TN, Argani P. Separate cavity margin sampling at the time of initial breast lumpectomy significantly reduces the need for reexcisions. Am J Surg Pathol. 2005; 29:1625–1632.
Article14. Jorns JM, Visscher D, Sabel M, Breslin T, Healy P, Daignaut S, et al. Intraoperative frozen section analysis of margins in breast conserving surgery significantly decreases reoperative rates: one-year experience at an ambulatory surgical center. Am J Clin Pathol. 2012; 138:657–669.
Article15. Osako T, Nishimura R, Nishiyama Y, Okumura Y, Tashima R, Nakano M, et al. Efficacy of intraoperative entire-circumferential frozen section analysis of lumpectomy margins during breast-conserving surgery for breast cancer. Int J Clin Oncol. 2015; 20:1093–1101.
Article16. Park EH, Min SY, Kim Z, Yoon CS, Jung KW, Nam SJ, et al. Basic facts of breast cancer in Korea in 2014: the 10-year overall survival progress. J Breast Cancer. 2017; 20:1–11.
Article17. Cendán JC, Coco D, Copeland EM 3rd. Accuracy of intraoperative frozen-section analysis of breast cancer lumpectomy-bed margins. J Am Coll Surg. 2005; 201:194–198.
Article18. Olson TP, Harter J, Muñoz A, Mahvi DM, Breslin T. Frozen section analysis for intraoperative margin assessment during breast-conserving surgery results in low rates of re-excision and local recurrence. Ann Surg Oncol. 2007; 14:2953–2960.
Article19. Weber WP, Engelberger S, Viehl CT, Zanetti-Dallenbach R, Kuster S, Dirnhofer S, et al. Accuracy of frozen section analysis versus specimen radiography during breast-conserving surgery for nonpalpable lesions. World J Surg. 2008; 32:2599–2606.
Article20. Fukamachi K, Ishida T, Usami S, Takeda M, Watanabe M, Sasano H, et al. Total-circumference intraoperative frozen section analysis reduces margin-positive rate in breast-conservation surgery. Jpn J Clin Oncol. 2010; 40:513–520.
Article21. Morrow M, Jagsi R, Alderman AK, Griggs JJ, Hawley ST, Hamilton AS, et al. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA. 2009; 302:1551–1556.
Article22. Jorns JM, Daignault S, Sabel MS, Wu AJ. Is intraoperative frozen section analysis of reexcision specimens of value in preventing reoperation in breast-conserving therapy? Am J Clin Pathol. 2014; 142:601–608.
Article23. Chen K, Zeng Y, Jia H, Jia W, Yang H, Rao N, et al. Clinical outcomes of breast-conserving surgery in patients using a modified method for cavity margin assessment. Ann Surg Oncol. 2012; 19:3386–3394.
Article24. Huston TL, Pigalarga R, Osborne MP, Tousimis E. The influence of additional surgical margins on the total specimen volume excised and the reoperative rate after breast-conserving surgery. Am J Surg. 2006; 192:509–512.
Article25. Tan MP, Sitoh NY, Sim AS. The value of intraoperative frozen section analysis for margin status in breast conservation surgery in a nontertiary institution. Int J Breast Cancer. 2014; 2014:715404.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Atypical Hyperplasia at the Margin of Frozen Sections from Breast-Conserving Surgery
- Intraoperative Specimen Mammography for Margin Assessment in Breast-Conserving Surgery
- Predictors of Positive or Close Surgical Margins in Breast-Conserving Surgery for Patients with Breast Cancer
- A Randomized Controlled Trial for Doing vs. Omitting Intraoperative Frozen Section Biopsy for Resection Margin Status in Selected Patients Undergoing Breast-Conserving Surgery (OFF-MAP Trial)
- The Practice Patterns and Perceptions of Korean Surgeons Regarding Margin Status after Breast-Conserving Surgery