Korean Circ J.
2017 Sep;47(5):776-785. 10.4070/kcj.2016.0295.
Systematic Review of Treatment for Trapped Thrombus in Patent Foramen Ovale
- Affiliations
-
- 1Division of Cardiology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. drhyangii@hallym.or.kr
- KMID: 2389610
- DOI: http://doi.org/10.4070/kcj.2016.0295
Abstract
- BACKGROUND AND OBJECTIVES
Trapped thrombus in patent foramen ovale (PFO) is a rare complication of pulmonary embolism that may lead to tragic clinical events. The aim of this study was to identify the optimal treatment for different clinical situations in patients with trapped thrombus in a PFO by conducting a literature review.
SUBJECTS AND METHODS
A PubMed database search was conducted from 1991 through 2015, and 194 patients (185 articles) with trapped thrombus in a PFO were identified. Patient characteristics, paradoxical embolic events, and factors affecting 60-day mortality were analyzed retrospectively.
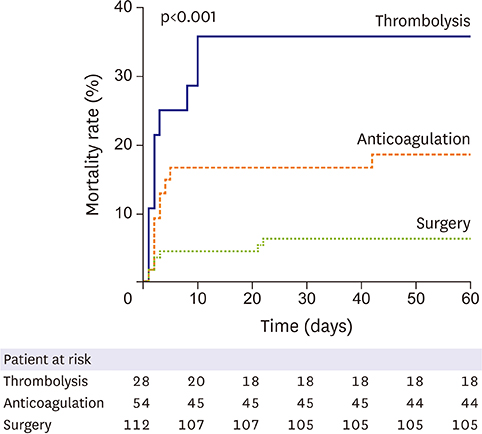
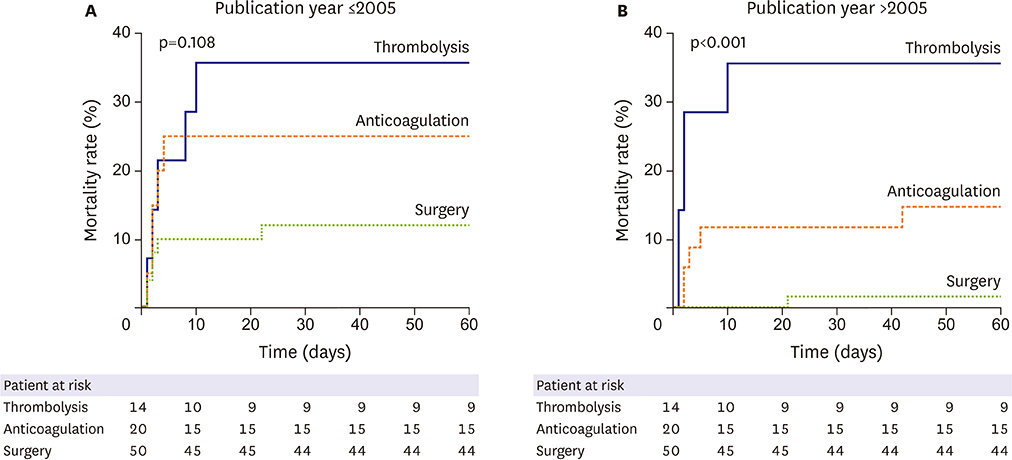
RESULTS
Among all patients, 112 (57.7%) were treated with surgery, 28 with thrombolysis, and 54 with anticoagulation alone. Dyspnea (79.4%), chest pain (33.0%), and syncope (17.5%) were the most common presenting symptoms. Pretreatment embolism was found in 37.6% of cases, and stroke (24.7%) was the most common event. Surgery was associated with fewer post-treatment embolic events than were other treatment options (p=0.044). In the multivariate analysis, initial shock or arrest, and thrombolysis were independent predictors of 60-day mortality. Thrombolysis was related with higher 60-day mortality compared with surgery in patients who had no initial shock or arrest.
CONCLUSION
This systematic review showed that surgery was associated with a lower overall incidence of post-treatment embolic events and a lower 60-day mortality in patients with trapped thrombus in a PFO. In patients without initial shock or arrest, thrombolysis was related with a higher 60-day mortality compared with surgery.
MeSH Terms
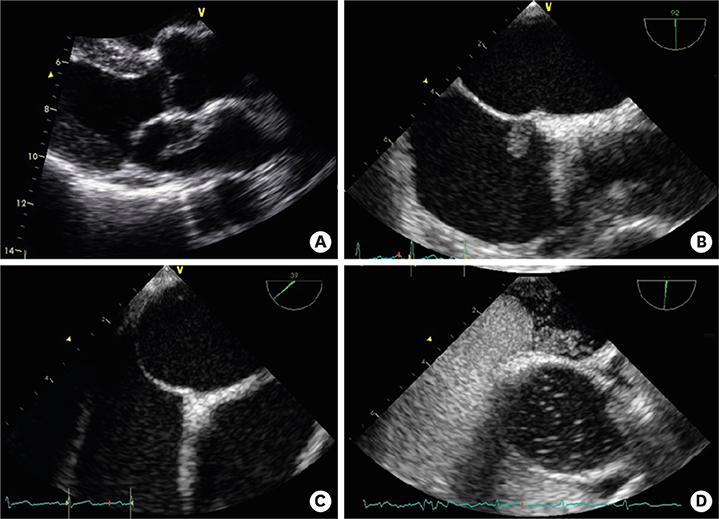
Figure
Reference
-
1. Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013; 81:619–625.2. Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984; 59:17–20.3. Konstantinides S, Geibel A, Kasper W, Olschewski M, Blümel L, Just H. Patent foramen ovale is an important predictor of adverse outcome in patients with major pulmonary embolism. Circulation. 1998; 97:1946–1951.4. Meacham RR 3rd, Headley AS, Bronze MS, Lewis JB, Rester MM. Impending paradoxical embolism. Arch Intern Med. 1998; 158:438–448.5. Fauveau E, Cohen A, Bonnet N, Gacem K, Lardoux H. Surgical or medical treatment for thrombus straddling the patent foramen ovale: impending paradoxical embolism? Report of four clinical cases and literature review. Arch Cardiovasc Dis. 2008; 101:637–644.6. Myers PO, Bounameaux H, Panos A, Lerch R, Kalangos A. Impending paradoxical embolism: systematic review of prognostic factors and treatment. Chest. 2010; 137:164–170.7. Mattox KL, Feldtman RW, Beall AC Jr, DeBakey ME. Pulmonary embolectomy for acute massive pulmonary embolism. Ann Surg. 1982; 195:726–731.8. Yalamanchili K, Fleisher AG, Lehrman SG, et al. Open pulmonary embolectomy for treatment of major pulmonary embolism. Ann Thorac Surg. 2004; 77:819–823.9. Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012; 141:e419S–e496S.10. Giannitsis E, Katus HA. Risk stratification in pulmonary embolism based on biomarkers and echocardiography. Circulation. 2005; 112:1520–1521.11. Torbicki A, Galié N, Covezzoli A, et al. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol. 2003; 41:2245–2251.12. Casazza F, Bongarzoni A, Centonze F, Morpurgo M. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol. 1997; 79:1433–1435.13. Chartier L, Béra J, Delomez M, et al. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999; 99:2779–2783.14. Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. 2002; 121:806–814.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thrombus in Transit within a Patent Foramen Ovale: Gone with the Cough!
- CT Diagnosis of Paradoxical Embolism via a Patent Foramen Ovale in a Patient with a Pulmonary Embolism and Prominent Eustachian Valve
- Tentatively Diagnosed as Myxoma : Transit Thrombus Entrapped in Patent Foramen Ovale
- Prelude of Tragedy: Entrapped Huge Thrombi into a Patent Foramen Ovale Impending Paradoxical Embolism
- Thrombus entrapped by patent foramen ovale in a patient with pulmonary embolism: a case report