Ann Rehabil Med.
2017 Jun;41(3):387-393. 10.5535/arm.2017.41.3.387.
Stroke Impact Scale 3.0: Reliability and Validity Evaluation of the Korean Version
- Affiliations
-
- 1Department of Rehabilitation Medicine, National Rehabilitation Center, Seoul, Korea. Kana69@nrc.go.kr
- 2Department of Rehabilitation Standard and Policy, National Rehabilitation Research Institute, Seoul, Korea.
- KMID: 2389453
- DOI: http://doi.org/10.5535/arm.2017.41.3.387
Abstract
OBJECTIVE
To establish the reliability and validity the Korean version of the Stroke Impact Scale (K-SIS) 3.0.
METHODS
A total of 70 post-stroke patients were enrolled. All subjects were evaluated for general characteristics, Mini-Mental State Examination (MMSE), the National Institutes of Health Stroke Scale (NIHSS), Modified Barthel Index, Hospital Anxiety and Depression Scale (HADS). The SF-36 and K-SIS 3.0 assessed their health-related quality of life. Statistical analysis after evaluation, determined the reliability and validity of the K-SIS 3.0.
RESULTS
A total of 70 patients (mean age, 54.97 years) participated in this study. Internal consistency of the SIS 3.0 (Cronbach's alpha) was obtained, and all domains had good co-efficiency, with threshold above 0.70. Test-retest reliability of SIS 3.0 required correlation (Spearman's rho) of the same domain scores obtained on the first and second assessments. Results were above 0.5, with the exception of social participation and mobility. Concurrent validity of K-SIS 3.0 was assessed using the SF-36, and other scales with the same or similar domains. Each domain of K-SIS 3.0 had a positive correlation with corresponding similar domain of SF-36 and other scales (HADS, MMSE, and NIHSS).
CONCLUSION
The newly developed K-SIS 3.0 showed high inter-intra reliability and test-retest reliabilities, together with high concurrent validity with the original and various other scales, for patients with stroke. K-SIS 3.0 can therefore be used for stroke patients, to assess their health-related quality of life and treatment efficacy.
MeSH Terms
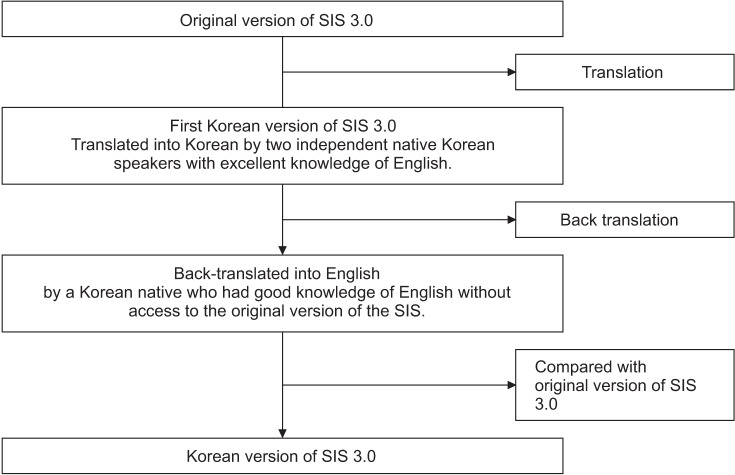
Figure
Cited by 1 articles
-
Korean Version of the Confidence of Arm and Hand Movement Scale and Its Psychometric Properties
Hanna Kim, Yeajin Ham, Joon-Ho Shin
Ann Rehabil Med. 2025;49(2):104-112. doi: 10.5535/arm.240077.
Reference
-
1. Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA. Global burden of stroke: an underestimate. Authors’ reply. Lancet. 2014; 383:1205–1206.2. Talabi OA. A 3-year review of neurologic admissions in University College Hospital Ibadan, Nigeria. West Afr J Med. 2003; 22:150–151. PMID: 14529226.
Article3. van der Zee CH, Visser-Meily JM, Lindeman E, Jaap Kappelle L, Post MW. Participation in the chronic phase of stroke. Top Stroke Rehabil. 2013; 20:52–61. PMID: 23340071.
Article4. Boosman H, Schepers VP, Post MW, Visser-Meily JM. Social activity contributes independently to life three years post stroke. Clin Rehabil. 2011; 25:460–467. PMID: 21059668.5. Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis. 2009; 27(Suppl 1):204–214.
Article6. Vellone E, Savini S, Barbato N, Carovillano G, Caramia M, Alvaro R. Quality of life in stroke survivors: first results from the reliability and validity of the Italian version of the Stroke Impact Scale 3.0. Ann Ig. 2010; 22:469–479. PMID: 21381542.7. Carod-Artal FJ, Coral LF, Trizotto DS, Moreira CM. The stroke impact scale 3.0: evaluation of acceptability, reliability, and validity of the Brazilian version. Stroke. 2008; 39:2477–2484. PMID: 18635846.8. Duncan PW, Wallace D, Lai SM, Johnson D, Embretson S, Laster LJ. The stroke impact scale version 2.0: evaluation of reliability, validity, and sensitivity to change. Stroke. 1999; 30:2131–2140. PMID: 10512918.9. Stewart JC, Cramer SC. Patient-reported measures provide unique insights into motor function after stroke. Stroke. 2013; 44:1111–1116. PMID: 23422082.
Article10. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198. PMID: 1202204.11. Appelros P, Terent A. Characteristics of the National Institute of Health Stroke Scale: results from a population-based stroke cohort at baseline and after one year. Cerebrovasc Dis. 2004; 17:21–27. PMID: 14530634.
Article12. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965; 14:61–65.13. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–370. PMID: 6880820.
Article14. Ware JE Jr, Sherbourne CD. The MOS 36-item shortform health survey (SF-36). I: Conceptual framework and item selection. Med Care. 1992; 30:473–483. PMID: 1593914.15. Duncan PW, Bode RK, Min Lai S, Perera S. Glycine Antagonist in Neuroprotection Americans Investigators. Rasch analysis of a new stroke-specific outcome scale: the Stroke Impact Scale. Arch Phys Med Rehabil. 2003; 84:950–963. PMID: 12881816.16. Poe SS, Cvach M, Dawson PB, Straus H, Hill EE. The Johns Hopkins Fall Risk Assessment Tool: postimplementation evaluation. J Nurs Care Qual. 2007; 22:293–298. PMID: 17873724.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korean Version of the Stroke Rehabilitation Motivation Scale: Reliability and Validity Evaluation
- Korean Version of the Confidence of Arm and Hand Movement Scale and Its Psychometric Properties
- Korean Version of the Revised UCLA Loneliness Scale: Reliability and Validity Test
- Reliability and Validity of Korean version of Diabetes Empowerment Scale Short Form
- Validity and Reliability of the Korean Version of Advance Directives Attitude Scale for Nurses