J Korean Acad Nurs.
2017 Aug;47(4):467-475. 10.4040/jkan.2017.47.4.467.
Health Promoting Behavior in Pregnant Couples: Actor-Partner Interdependence Model Analysis
- Affiliations
-
- 1College of Nursing Science · East-West Nursing Research Institute, Kyung Hee University, Seoul, Korea. juheekim@khu.ac.kr
- 2Department of Nursing, Ansan University, Ansan, Korea.
- KMID: 2389023
- DOI: http://doi.org/10.4040/jkan.2017.47.4.467
Abstract
- PURPOSE
This study aimed to identify the actor and partner effects of self-efficacy, marital adjustment, and social support on the health promoting behavior of Korean pregnant couples.
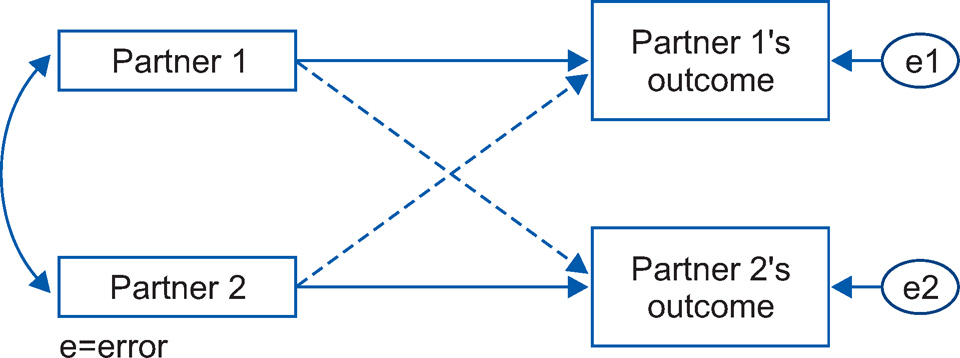
METHODS
Participants were 132 couples who met the eligibility criteria. Data were collected from June to November, 2016 at a community health center. The Actor-Partner Interdependence Model was used for analyzing the actor and partner effects of self-efficacy, marital adjustment, and social support on health promoting behavior.
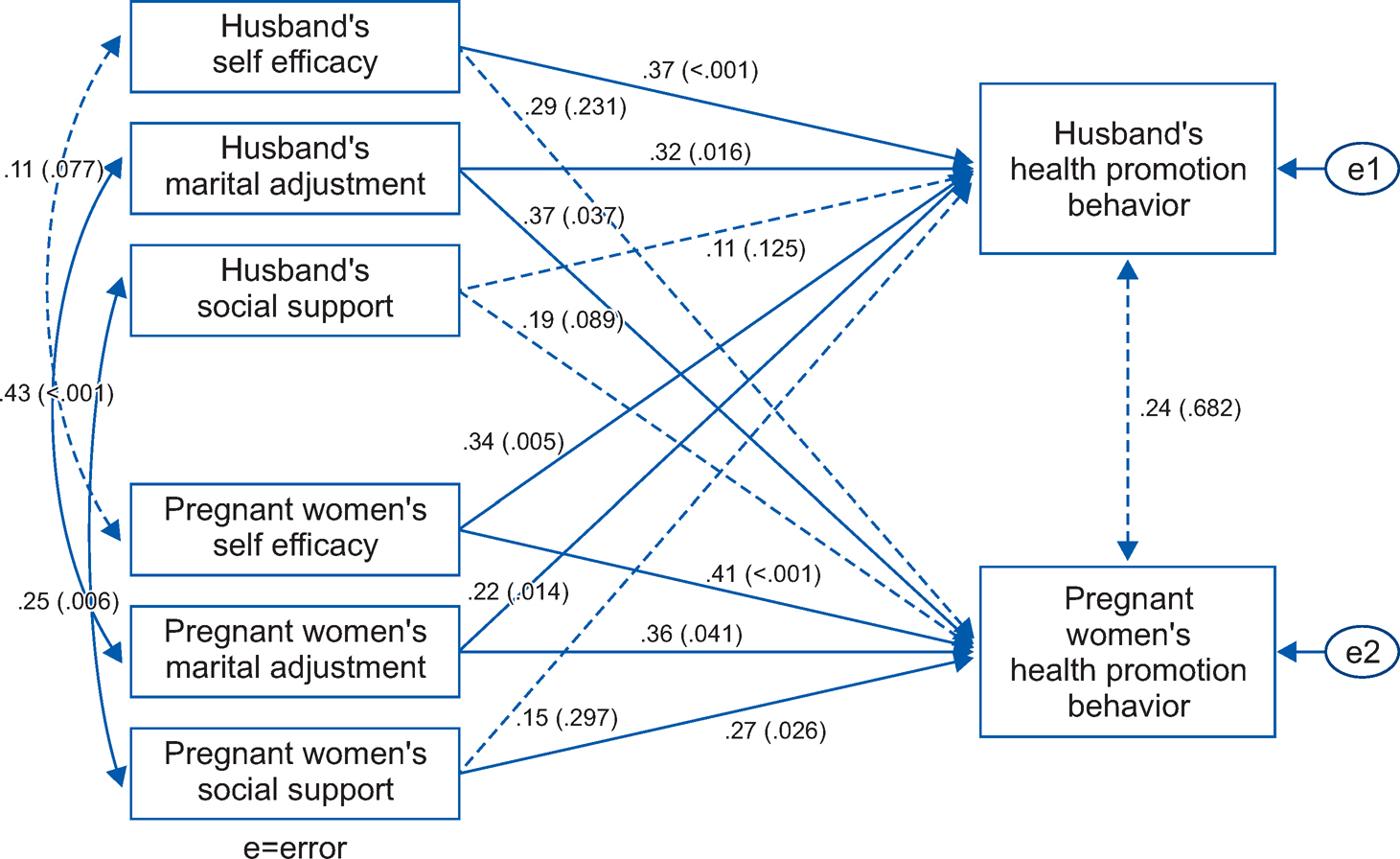
RESULTS
The fitness indices for the model were GFI=0.90, NFI=0.92, CFI=0.91, TLI=0.90, and RMSEA=0.04, which satisfied the criteria. Self-efficacy had actor and partner effect on health promoting behavior of wives, but had only actor effect of on health promoting behavior of husbands. Marital adjustment showed actor and partner effect on the health promoting behavior of pregnant couples. Social support only had an actor effect on the health promoting behavior of wives. And, marital adjustment and social support had a mutual effect.
CONCLUSION
This study indicates that the partner involvement is needed to develop health promotion programs for pregnant couples.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Factors associated with clinical nurses’ preconception health behavior in Korea: a cross-sectional survey
Yoon-Jung Park, Sun-Hee Kim
Womens Health Nurs. 2024;30(1):79-89. doi: 10.4069/whn.2024.03.08.
Reference
-
References
1. Demographic trend for Korea: 1995-2015 [Internet]. Daejeon: Statistics Korea;c2016. [cited 2016 Dec 7]. Available from. http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&parmTabId=M_01_01.2. Choi GY. Fetal origins of adult disease. Korean Journal of Obstetrics and Gynecology. 2010; 53(6):475–488. http://dx.doi.org/10.5468/kjog.2010.53.6.475.
Article3. Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. The Lancet. 1993; 341(8850):938–941. http://dx.doi.org/10.1016/0140-6736(93)91224-A.
Article4. Faa G, Manchia M, Pintus R, Gerosa C, Marcialis MA, Fanos V. Fetal programming of neuropsychiatric disorders. Birth Defects Research Part C: Embryo Today: Reviews. 2016; 108(3):207–223. http://dx.doi.org/10.1002/bdrc.21139.
Article5. Sim K, Chun WY. The relationships between indicators of the prenatal environment and behaviors associated with HPA axis dysfunction. The Korean Journal of Developmental Psychology. 2015; 28(3):1–28.6. Freathy RM, Weedon MN, Bennett A, Hypponen E, Relton CL, Knight B, et al. Type 2 diabetes TCF7L2 risk genotypes alter birth weight: a study of 24,053 individuals. American Journal of Human Genetics. 2007; 80(6):1150–1161. http://dx.doi.org/10.1086/518517.
Article7. Bailey BA, Byrom AR. Factors predicting birth weight in a low-risk sample: the role of modifiable pregnancy health behaviors. Maternal and Child Health Journal. 2007; 11(2):173–179. http://dx.doi.org/10.1007/s10995-006-0150-7.
Article8. Cheng TS, Loy SL, Cheung YB, Godfrey KM, Gluckman PD, Kwek K, et al. Demographic characteristics, health behaviors before and during pregnancy, and pregnancy and birth outcomes in mothers with different pregnancy planning status. Prevention Science. 2016; 17(8):960–969. http://dx.doi.org/10.1007/s11121-016-0694-8.
Article9. Xu J, Barinas-Mitchell E, Kuller LH, Youk AO, Catov JM. Maternal hypertension after a low-birth-weight delivery differs by race/ethnicity: evidence from the National Health and Nutrition Examination Survey (NHANES) 1999-2006. PLoS One. 2014; 9(8):e104149. http://dx.doi.org/10.1371/journal.pone.0104149.
Article10. Ornoy A, Reece EA, Pavlinkova G, Kappen C, Miller RK. Effect of maternal diabetes on the embryo, fetus, and children: congenital anomalies, genetic and epigenetic changes and developmental outcomes. Birth Defects Research Part C: Embryo Today: Reviews. 2015; 105(1):53–72. http://dx.doi.org/10.1002/bdrc.21090.
Article11. Herbst MA, Mercer BM, Beazley D, Meyer N, Carr T. Relationship of prenatal care and perinatal morbidity in low-birth-weight infants. American Journal of Obstetrics and Gynecology. 2003; 189(4):930–933. http://dx.doi.org/10.1067/S0002-9378(03)01055-X.
Article12. Zhang HL, Li CY, Kim HL. Status and influencing factors of health behavior in pregnant women in Yanbian area. Journal of the Korea Academia-Industrial Cooperation Society. 2015; 16(11):7863–7869. http://dx.doi.org/10.5762/kais.2015.16.11.7863.
Article13. Tilden EL, Caughey AB, Lee CS, Emeis C. The effect of childbirth self-efficacy on perinatal outcomes. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2016; 45(4):465–480. http://dx.doi.org/10.1016/j.jogn.2016.06.003.
Article14. Buttram ME, Kurtz SP, Surratt HL. Substance use and sexual risk mediated by social support among black men. Journal of Community Health. 2013; 38(1):62–69. http://dx.doi.org/10.1007/s10900-012-9582-8.
Article15. Hui Choi WH, Lee GL, Chan CH, Cheung RY, Lee IL, Chan CL. The relationships of social support, uncertainty, self-efficacy, and commitment to prenatal psychosocial adaptation. Journal of Advanced Nursing. 2012; 68(12):2633–2645. http://dx.doi.org/10.1111/j.1365-2648.2012.05962.x.
Article16. Mihelic M, Filus A, Morawaska A. Correlates of prenatal parenting expectations in new mothers: is better self-efficacy a potential target for preventing postnatal adjustment difficulties? Prevention Science. 2016; 17(8):949–959. http://dx.doi.org/10.1007/s11121-016-0682-z.
Article17. Cohen K, Capponi S, Nyamukapa M, Baxter J, Crawford A, Worly B. Partner involvement during pregnancy and maternal health behaviors. Maternal and Child Health Journal. 2016; 20(11):2291–2298. http://dx.doi.org/10.1007/s10995-016-2048-3.
Article18. Korja R, Piha J, Otava R, Lavanchy-Scaiola C, Ahlqvist-Björkroth S, Aromaa M, et al. Mother’s marital satisfaction associated with the quality of mother-father-child triadic interaction. Scandinavian Journal of Psychology. 2016; 57(4):305–312. http://dx.doi.org/10.1111/sjop.12294.
Article19. Alio AP, Lewis CA, Scarborough K, Harris K, Fiscella K. A community perspective on the role of fathers during pregnancy: a qualitative study. BMC Pregnancy and Childbirth. 2013; 13:60. http://dx.doi.org/10.1186/1471-2393-13-60.
Article20. Peterson BD, Newton CR, Rosen KH. Examining congruence between partners’ perceived infertility-related stress and its relationship to marital adjustment and depression in infertile couples. Family Process. 2003; 42(1):59–70. http://dx.doi.org/10.1111/j.1545-5300.2003.00059.x.
Article21. Kenny DA. Models of non-independence in dyadic research. Journal of Social and Personal Relationships. 1996; 13(2):279–294. http://dx.doi.org/10.1177/0265407596132007.
Article22. Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: the perinatal maternal health promotion model. Journal of Midwifery & Women’s Health. 2013; 58(6):613–621. http://dx.doi.org/10.1111/jmwh.12139.
Article23. Henriksen RE, Thuen F. Marital quality and stress in pregnancy predict the risk of infectious disease in the offspring: the Norwegian mother and child cohort study. PLoS One. 2015; 10(9):e0137304. http://dx.doi.org/10.1371/journal.pone.0137304.
Article24. Ayotte BJ, Margrett JA, Patrick JH. Dyadic analysis of self-efficacy and perceived support: the relationship of individual and spousal characteristics with physical activity among middle-aged and young-older adults. Psychology and Aging. 2013; 28(2):555–563. http://dx.doi.org/10.1037/a0032454.
Article25. Kim YM, Park HS. Relationship between perceived spouse support and health promoting behavior in the breast cancer patient with mastectomy. Asian Oncology Nursing. 2014; 14(4):203–211. http://dx.doi.org/10.5388/aon.2014.14.4.203.
Article26. Kelley HH, Thibaut JW. Interpersonal relations: a theory of interdependence. New York, NY: WIiley;1978. p. 25.27. Benyamini Y, Ashery L, Shiloh S. Involving husbands in their wives’ health behavior: Does it work? Health and Well-Being. 2011; 3(1):66–86. http://dx.doi.org/10.1111/j.1758-0854.2010.01041.x.28. Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychological Bulletin. 2001; 127(4):472–503. http://dx.doi.org/10.1037/0033-2909.127.4.472.
Article29. Ko SJ, Shin SH. Effects of dementia knowledge, self-efficacy and depression on dementia preventive behavior in elderly couples: dyadic data analysis. Journal of Korean Academy Nursing. 2013; 43(2):276–286. http://dx.doi.org/10.4040/jkan.2013.43.2.276.
Article30. Hair JF, Black WC, Babin B, Anderson RE, Tatham RL. Multivariate data analysis. 6th ed. Upper Saddle River, NU: Pearson Prentice Hall;2006. p. 217.31. Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The self-efficacy scale: construction and validation. Psychological Reports. 1982; 51(2):663–671. http://dx.doi.org/10.2466/pr0.1982.51.2.663.
Article32. Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976; 38(1):15–28. http://dx.doi.org/10.2307/350547.
Article33. Choi SI. Revision dyadic adjustment scale: reliability and validity (Ko Hwang Thesis No.35, 97-114). Seoul: Graduate School, Kyung Hee University;2004. p. 24.34. Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983; 13(2):99–125. http://dx.doi.org/10.1111/j.1559-1816.1983.tb02325.x.35. Walker SN, Sechrist KR, Pender NJ. The health-promoting lifestyle profile: development and psychometric characteristics. Nursing Research. 1987; 36(2):76–81. http://dx.doi.org/10.1097/00006199-198703000-00002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Sexual Attitude and Marital Intimacy on Sexual Satisfaction in Pregnant Couples: An Application of the Actor-Partner Interdependence Model
- Actor and Partner Effects of Health Status, Marital Satisfaction and Self Efficacy on Retirement Preparation of Middle Aged Couples: Actor-Partner Interdependence Model Analysis
- The Effects of Climacteric Symptom Cognition, Self-efficacy on Aging Anxiety in Middle-Aged Couples: Actor and Partner Interdependence Mediation Model
- The Effects of Self-esteem and Family Stress on Depression of Middle-aged Couples: Analysis of Actor-Partner Interdependence Model
- Mediating effect of Maternal and Paternal Family Relationship between Neuroticism and Postpartum Depression: The Actor-Partner Interdependence Mediation Model