World J Mens Health.
2017 Aug;35(2):115-119. 10.5534/wjmh.2017.35.2.115.
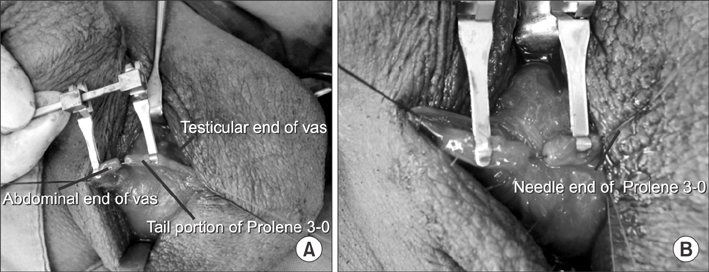
Loupe-Assisted Vasovasostomy Using a Prolene Stent: A Simpler Vasectomy Reversal Technique
- Affiliations
-
- 1Department of Urology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. urofirst@hanm ail.net
- KMID: 2388447
- DOI: http://doi.org/10.5534/wjmh.2017.35.2.115
Abstract
- PURPOSE
Microsurgical vasovasostomy is associated with high patency and pregnancy rates, but is difficult and requires significant effort and time to learn. Therefore, we assessed a simplified loupe-assisted vasovasostomy method using a Prolene stent.
MATERIALS AND METHODS
The medical records of 82 patients who underwent loupe-assisted vasovasostomy with a Prolene stent by a single surgeon between January 2004 and December 2015 were reviewed. The association between the vasal obstructive interval (VOI) and the success rate was evaluated.
RESULTS
The average age at the time of vasovasostomy was 39.8 years (range, 29~57 years). The mean VOI was 6.6 years (range, 1~19 years). The mean operation time was 87.0 minutes (range, 55.0~140.0 minutes). The overall patency and natural pregnancy rates were 90.2% and 45.1%, respectively. The success rate decreased as time after vasectomy increased (odds ratio, 0.869; 95% confidence interval, 0.760~0.993; p=0.039). The cases were divided into 2 groups according to the mean VOI: group A (>7 years) and group B (≤7 years), with 31 cases (37.8%) and 51 cases (62.2%), respectively. The patency and pregnancy rates of group A were 80.6% and 51.6%, respectively, while those of group B were 96.1% and 41.2%, respectively.
CONCLUSIONS
Loupe-assisted vasovasostomy using a Prolene stent is a safe and effective method.
Keyword
MeSH Terms
Figure
Reference
-
1. Weiske WH. Vasectomy. Andrologia. 2001; 33:125–134.
Article2. Dickey RM, Pastuszak AW, Hakky TS, Chandrashekar A, Ramasamy R, Lipshultz LI. The evolution of vasectomy reversal. Curr Urol Rep. 2015; 16:40.
Article3. Lee HY. A 20-year experience with vasovasostomy. J Urol. 1986; 136:413–415.
Article4. Herrel L, Hsiao W. Microsurgical vasovasostomy. Asian J Androl. 2013; 15:44–48.
Article5. Sharma V, Le BV, Sheth KR, Zargaroff S, Dupree JM, Cashy J, et al. Vasectomy demographics and postvasectomy desire for future children: results from a contemporary national survey. Fertil Steril. 2013; 99:1880–1885.
Article6. Silber SJ. Microscopic vasectomy reversal. Fertil Steril. 1977; 28:1191–1202.7. Silber SJ. Microsurgery in clinical urology. Urology. 1975; 6:150–153.
Article8. Singh I, Kaza RC. A case in favour of one sided microscopic vasovasostomy: the New Delhi experience. Int Urol Nephrol. 1996; 28:27–31.9. Boorjian S, Lipkin M, Goldstein M. The impact of obstructive interval and sperm granuloma on outcome of vasectomy reversal. J Urol. 2004; 171:304–306.
Article10. Belker AM, Thomas AJ Jr, Fuchs EF, Konnak JW, Sharlip ID. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. J Urol. 1991; 145:505–511.
Article11. Herrel LA, Goodman M, Goldstein M, Hsiao W. Outcomes of microsurgical vasovasostomy for vasectomy reversal: a meta-analysis and systematic review. Urology. 2015; 85:819–825.
Article12. Safarinejad MR, Lashkari MH, Asgari SA, Farshi A, Babaei AR. Comparison of macroscopic one-layer over number 1 nylon suture vasovasostomy with the standard two-layer microsurgical procedure. Hum Fertil (Camb). 2013; 16:194–199.
Article13. Silber SJ, Grotjan HE. Microscopic vasectomy reversal 30 years later: a summary of 4010 cases by the same surgeon. J Androl. 2004; 25:845–859.
Article14. Schmidt SS. Vasovasostomy. Urol Clin North Am. 1978; 5:585–592.
Article15. Sharlip ID. Vasovasostomy: comparison of two microsurgical techniques. Urology. 1981; 17:347–352.
Article16. Nyame YA, Babbar P, Almassi N, Polackwich AS, Sabanegh E. Comparative cost-effectiveness analysis of modified 1-layer versus formal 2-layer vasovasostomy technique. J Urol. 2016; 195:434–438.
Article17. Gerrard ER Jr, Sandlow JI, Oster RA, Burns JR, Box LC, Kolettis PN. Effect of female partner age on pregnancy rates after vasectomy reversal. Fertil Steril. 2007; 87:1340–1344.
Article18. Kolettis PN, Sabanegh ES, Nalesnik JG, D'Amico AM, Box LC, Burns JR. Pregnancy outcomes after vasectomy reversal for female partners 35 years old or older. J Urol. 2003; 169:2250–2252.
Article19. Fuchs EF, Burt RA. Vasectomy reversal performed 15 years or more after vasectomy: correlation of pregnancy outcome with partner age and with pregnancy results of in vitro fertilization with intracytoplasmic sperm injection. Fertil Steril. 2002; 77:516–519.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Results of modified one-layer vasocasostomy with optical loupe magnification
- Microscopic 2-Layer Vasovasostomy
- Results of modified two-layer vasovasostomy with optical loupe magnification
- The Level of FSH, LH and Testosterone in Seminal Plasma with the Procedure of Vasectomy and Vasovasostomy
- Correlation Between Histological Changes of Human Testis after and Fertility after Subsequent Vasectomy Reversal Vasectomy