Ann Surg Treat Res.
2017 Jun;92(6):436-439. 10.4174/astr.2017.92.6.436.
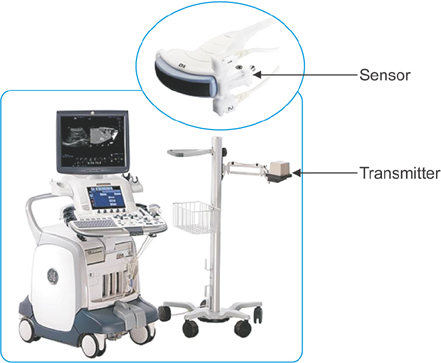
Ultrasound fusion imaging with real-time navigation for the surveillance after endovascular aortic aneurysm repair
- Affiliations
-
- 1Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea. jhjoh@khu.ac.kr
- KMID: 2387418
- DOI: http://doi.org/10.4174/astr.2017.92.6.436
Abstract
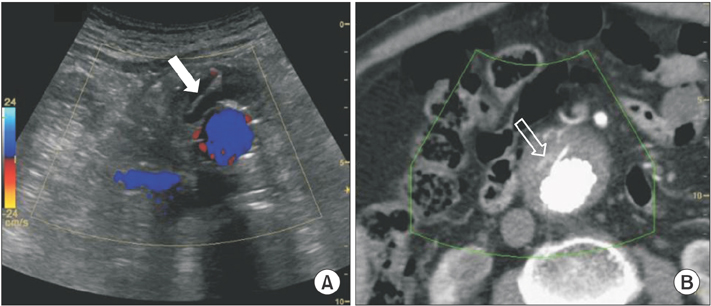
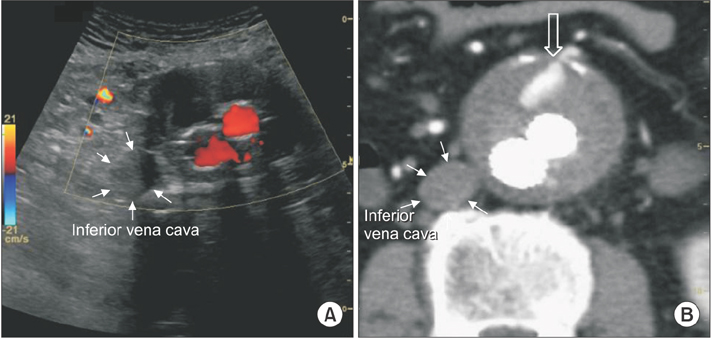
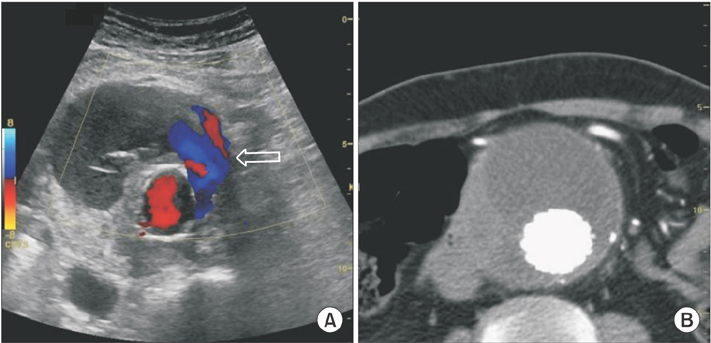
- Ultrasound can be an effective alternative to computed tomography for surveillance following endovascular aneurysm repair (EVAR). Recently, ultrasound fusion imaging with the real-time navigation system was introduced. Here we described 3 patients who underwent post-EVAR surveillance using this novel technique. Complete coregistration was achieved in all patients. The origin of left renal artery was selected for the target of coregistration. Ultrasound fusion imaging was useful to differentiate the confusing lesion and to evaluate the complete resolution of endoleak and newly developed delayed endoleak. Ultrasound fusion image with real-time navigation system can be a feasible imaging tool for post-EVAR surveillance.
MeSH Terms
Figure
Reference
-
1. Stroupe KT, Lederle FA, Matsumura JS, Kyriakides TC, Jonk YC, Ge L, et al. Cost-effectiveness of open versus endovascular repair of abdominal aortic aneurysm in the OVER trial. J Vasc Surg. 2012; 56:901–901.e2.2. Chaikof EL, Brewster DC, Dalman RL, Makaroun MS, Illig KA, Sicard GA, et al. The care of patients with an abdominal aortic aneurysm: the Society for Vascular Surgery practice guidelines. J Vasc Surg. 2009; 50:4 Suppl. S2–S49.3. Walker TG, Kalva SP, Yeddula K, Wicky S, Kundu S, Drescher P, et al. Clinical practice guidelines for endovascular abdominal aortic aneurysm repair: written by the Standards of Practice Committee for the Society of Interventional Radiology and endorsed by the Cardiovascular and Interventional Radiological Society of Europe and the Canadian Interventional Radiology Association. J Vasc Interv Radiol. 2010; 21:1632–1655.4. Pfister K, Schierling W, Jung EM, Apfelbeck H, Hennersperger C, Kasprzak PM. Standardized 2D ultrasound versus 3D/4D ultrasound and image fusion for measurement of aortic aneurysm diameter in follow-up after EVAR. Clin Hemorheol Microcirc. 2016; 62:249–260.5. Toshikuni N, Tsutsumi M, Takuma Y, Arisawa T. Real-time image fusion for successful percutaneous radiofrequency ablation of hepatocellular carcinoma. J Ultrasound Med. 2014; 33:2005–2010.6. Tomonari A, Tsuji K, Yamazaki H, Aoki H, Kang JH, Kodama Y, et al. Feasibility of the virtual needle tracking system for percutaneous radiofrequency ablation of hepatocellular carcinoma. Hepatol Res. 2013; 43:1352–1355.7. Cantisani V, Grazhdani H, Clevert DA, Iezzi R, Aiani L, Martegani A, et al. EVAR: Benefits of CEUS for monitoring stent-graft status. Eur J Radiol. 2015; 84:1658–1665.8. Ten Bosch JA, Rouwet EV, Peters CT, Jansen L, Verhagen HJ, Prins MH, et al. Contrast-enhanced ultrasound versus computed tomographic angiography for surveillance of endovascular abdominal aortic aneurysm repair. J Vasc Interv Radiol. 2010; 21:638–643.9. Yu H, Fahrig R, Pelc NJ. Co-registration of x-ray and MR fields of view in a hybrid XMR system. J Magn Reson Imaging. 2005; 22:291–301.10. Goerres GW, Schuknecht B, Schmid DT, Stoeckli SJ, Hany TF. Positron emission tomography/computed tomography for staging and restaging of head and neck cancer: comparison with positron emission tomography read together with contrast-enhanced computed tomography. Clin Imaging. 2008; 32:431–437.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Abdominal Aortic Aneurysm with Antecedent Endovascular Repair of Abdominal Aortic Aneurysm
- Endovascular Repair of Thoracic Aortic Aneurysm Using a Custom-made Fenestrated Stent Graft to Preserve the Left Subclavian Artery
- The Complications and Their Management after Endovascular Aneurysm Repair for the Treatment of Abdominal Aortic Aneurysms
- Successful Endovascular Treatment of Delayed Type Ib Endoleak with Aortic Rupture after Endovascular Repair of Abdominal Aortic Aneurysm
- Simultaneous Endovascular Aneurysm Repair for Abdominal Aortic Aneurysm Combined with Saccular Thoracic Aortic Aneurysm