J Korean Ophthalmol Soc.
2017 Jul;58(7):870-874. 10.3341/jkos.2017.58.7.870.
Intravitreal Ranibizumab Injection in Adult-onset Coats' Disease: A Case Report
- Affiliations
-
- 1Department of Ophthalmology, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea. sungpyo@hanafos.com
- KMID: 2387164
- DOI: http://doi.org/10.3341/jkos.2017.58.7.870
Abstract
- PURPOSE
To report a case of adult-onset Coats' disease which showed decreased retinal edema and improved visual acuity following intravitreal ranibizumab injection.
CASE SUMMARY
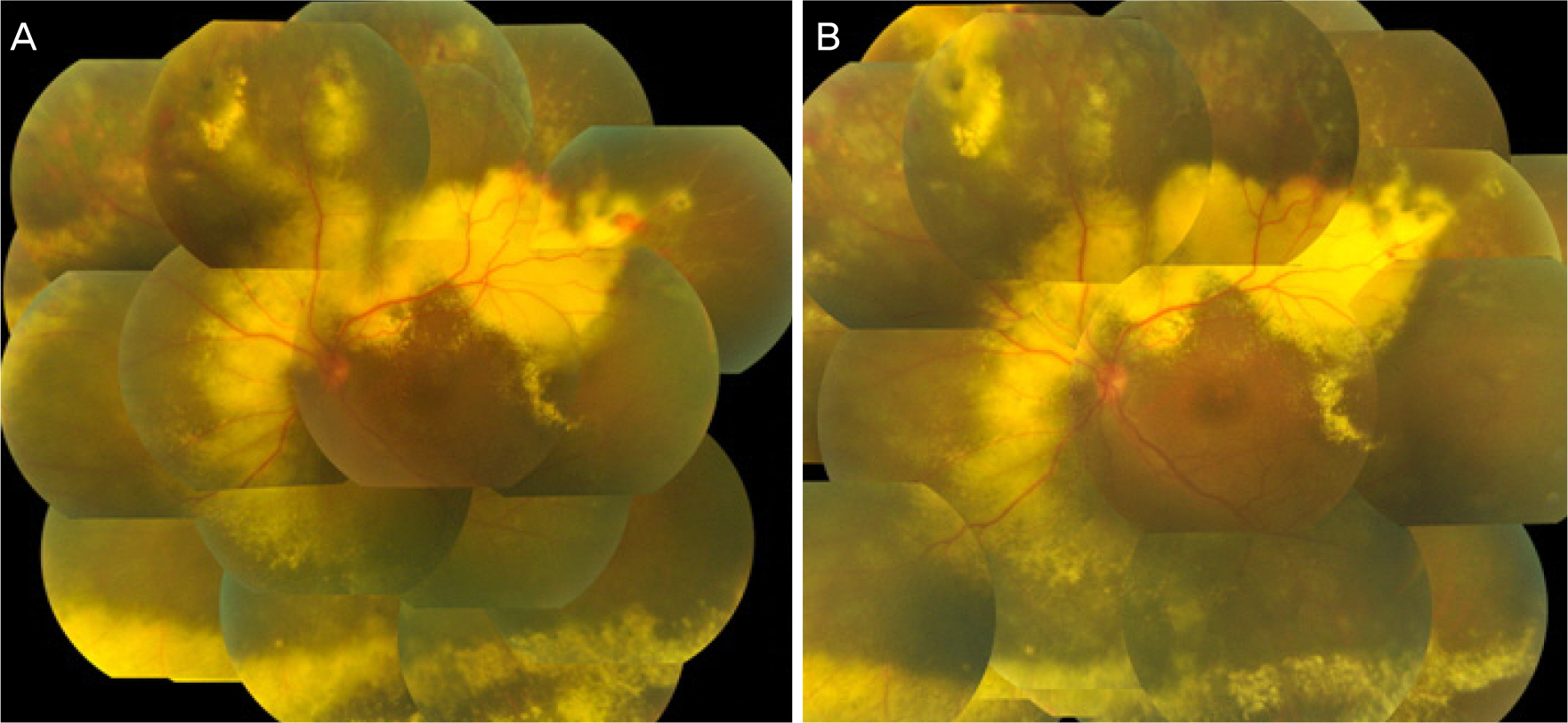
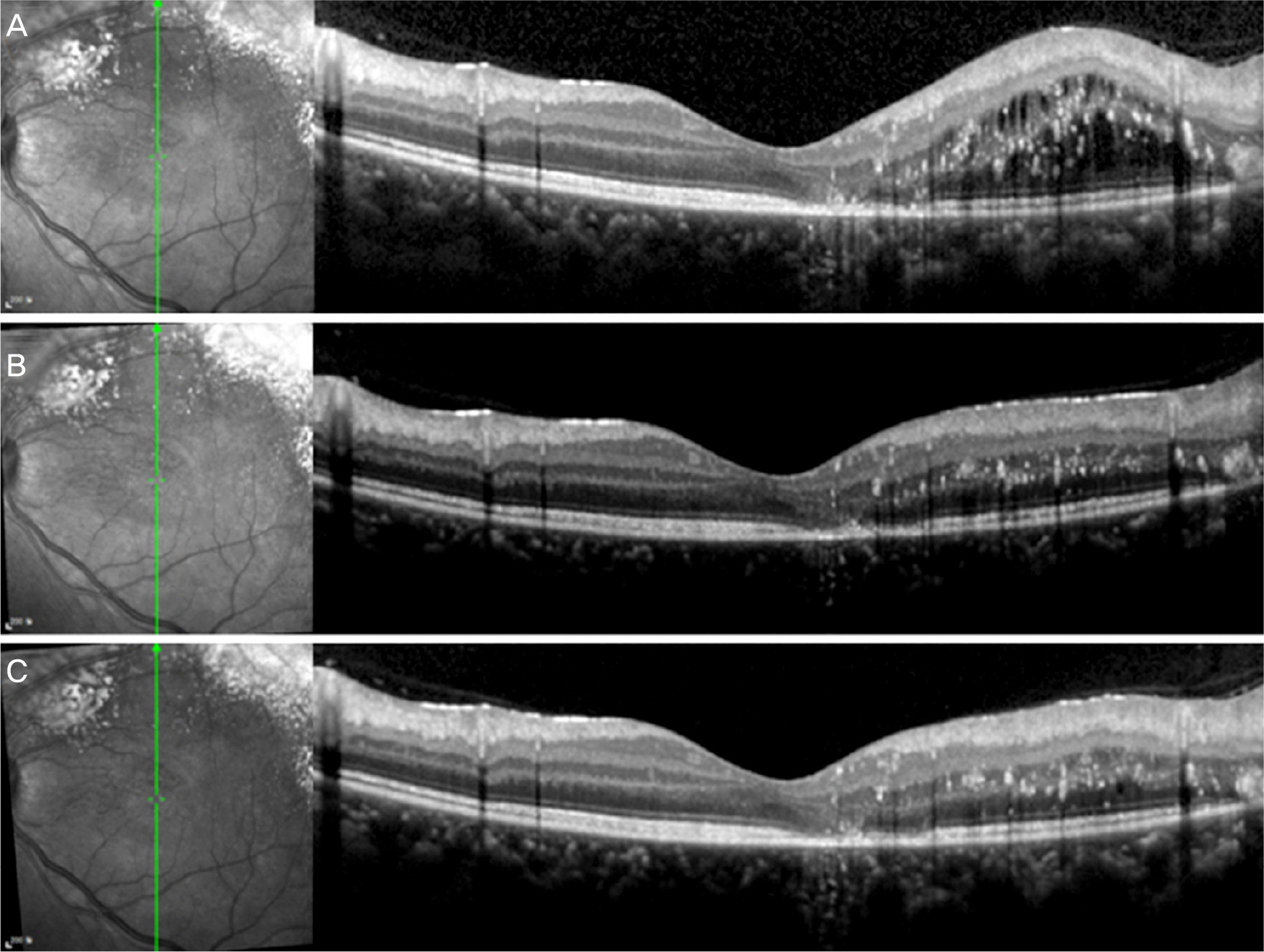
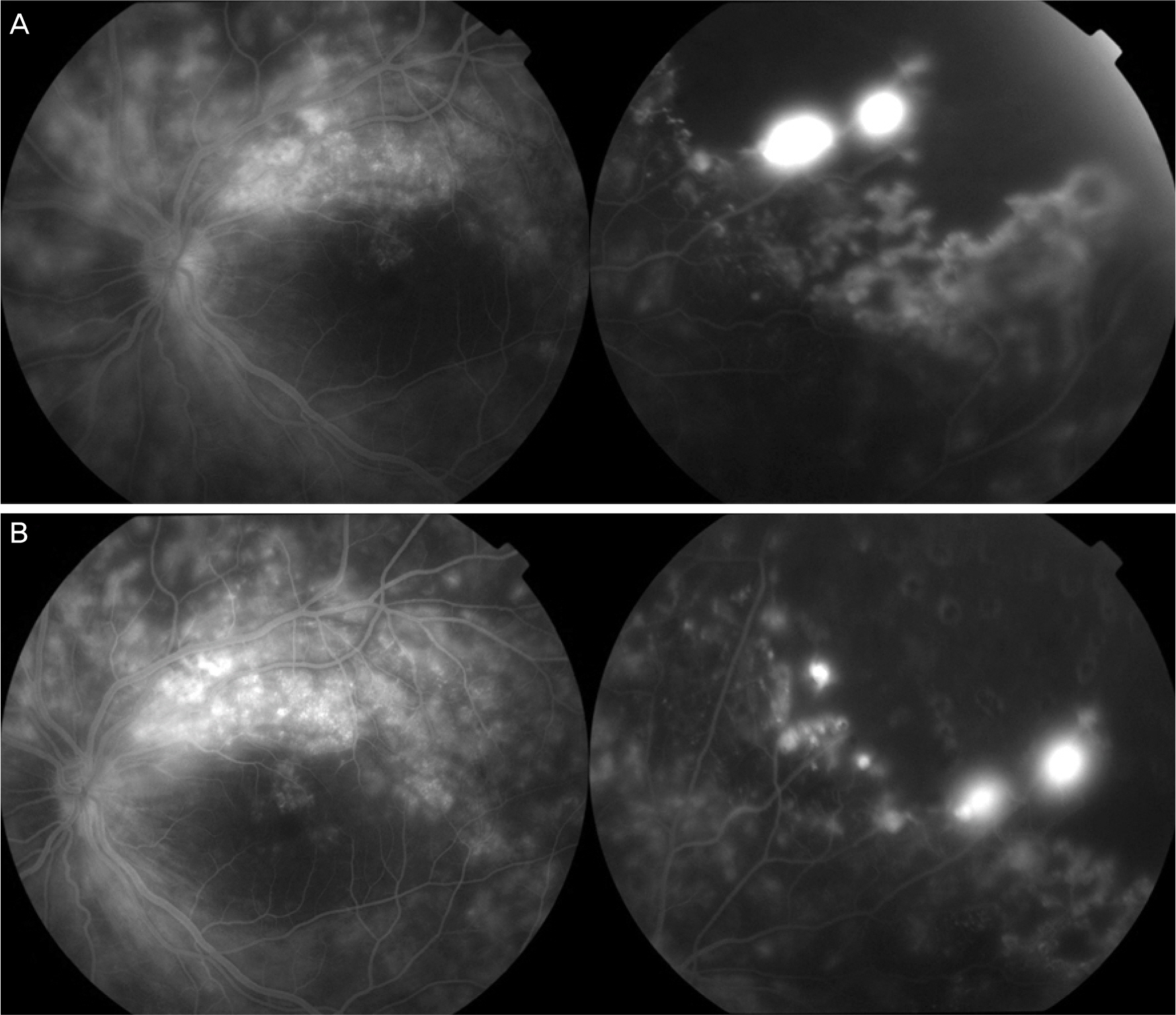
A 21-year-old woman visited our hospital for decreased visual acuity in left eye from 3 months ago. Her best corrected visual acuity was 1.0 in the right eye, and 0.4 in the left eye. The intraocular pressure was 19 mmHg in the right eye and 16 mmHg in the left eye. At anterior segment examination, no abnormal findings were found. On fundus examination, subretinal exudates, superior retinal edema at posterior pole, and telangiectasia along superortemporal vascular arcade were observed in the left eye. Upon diagnosis as Coats' disease, intravitreal ranibizumab was performed, and laser photocoagulation was done around the retinal telangiectasia and nonperfusion area. Then, the second and third intravitreal ranibizumab injections were performed by a month, and her best visual acuity was improved to 0.8 and optical coherence tomography revealed decreased retinal edema.
CONCLUSIONS
We report a case of adult-onset Coats' disease. Intravitreal ranibizumab injection is effective in rapid visual improvement and decrease of retinal edema as combination therapy with laser photocoagulation which was a generalized treatment of choice in Coats' disease.
MeSH Terms
Figure
Reference
-
References
1. Egerer I, Tasman W, Tomer TT. Coats disease. Arch Ophthalmol. 1974; 92:109–12.
Article2. Ridley ME, Shields JA, Brown GC, Tasman W. Coats' disease. Evaluation of management. Ophthalmology. 1982; 89:1381–7.3. Schefler AC, Berrocal AM, Murray TG. Advanced Coats' disease. Management with repetitive aggressive laser ablation therapy. Retina. 2008; 28:S38–41.4. Lin CJ, Hwang JF, Chen YT, Chen SN. The effect of intravitreal bevacizumab in the treatment of coats disease in children. Retina. 2010; 30:617–22.
Article5. Ray R, Barañano DE, Hubbard GB. Treatment of coats' disease with intravitreal bevacizumab. Br J Ophthalmol. 2013; 97:272–7.
Article6. Gaillard MC, Mataftsi A, Balmer A, et al. Ranibizumab in the management of advanced coats disease stages 3B and 4: long-term outcomes. Retina. 2014; 34:2275–81.7. Chang MM, McLean IW, Merritt JC. Coats' disease: a study of 62 histologically confirmed cases. J Pediatr Ophthalmol Strabismus. 1984; 21:163–8.
Article8. Fernandes BF, Odashiro AN, Maloney S, et al. Clinical-histopathological correlation in a case of Coats' disease. Diagn Pathol. 2006; 1:24.
Article9. Ghorbanian S, Jaulim A, Chatziralli IP. Diagnosis and treatment of coats' disease: a review of the literature. Ophthalmologica. 2012; 227:175–82.
Article10. Cremers FP, Maugeri A, den Hollander AI, Hoyng CB. The expanding roles of ABCA4 and CRB1 in inherited blindness. Novartis Found Symp. 2004; 255:68–79. discussion 79-84, 177–8.
Article11. Dickinson JL, Sale MM, Passmore A, et al. Mutations in the NDP gene: contribution to norrie disease, familial exudative vitreoretinopathy and retinopathy of prematurity. Clin Exp Ophthalmol. 2006; 34:682–8.
Article12. Shields JA, Shields CL, Honavar SG, et al. Classification and management of coats disease: the 2000 proctor lecture. Am J Ophthalmol. 2001; 131:572–83.
Article13. Shields JA, Shields CL. Review: coats disease: the 2001 LuEsther T. Mertz lecture. Retina. 2002; 22:80–91.15. Smithen LM, Brown GC, Brucker AJ, et al. Coats' disease diagnosed in adulthood. Ophthalmology. 2005; 112:1072–8.
Article16. Alvarez-Rivera LG, Abraham-Marín ML, Flores-Orta HJ, et al. Coat's disease treated with bevacizumab (Avastin). Arch Soc Esp Oftalmol. 2008; 83:329–31.17. Entezari M, Ramezani A, Safavizadeh L, Bassirnia N. Resolution of macular edema in coats' disease with intravitreal bevacizumab. Indian J Ophthalmol. 2010; 58:80–2.
Article18. Jun JH, Kim YC, Kim KS. Resolution of severe macular edema in adult coats' disease with intravitreal triamcinolone and bevacizumab injection. Korean J Ophthalmol. 2008; 22:190–3.
Article19. Kim J, Park KH, Woo SJ. Combined photodynamic therapy and intravitreal bevacizumab injection for the treatment of adult coats' disease: a case report. Korean J Ophthalmol. 2010; 24:374–6.
Article20. He YG, Wang H, Zhao B, et al. Elevated vascular endothelial growth factor level in coats' disease and possible therapeutic role of bevacizumab. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1519–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intravitreal Bevacizumab Injection in Adult Coats' Disease
- Efficacy of Primary Intravitreal Ranibizumab Injection for Treatment of Type 1 Retinopathy of Prematurity
- Comparison of Intravitreal Bevacizumab and Ranibizumab Injections in Aggressive and Type 1 Retinopathy of Prematurity
- Combined Photodynamic Therapy and Intravitreal Bevacizumab Injection for the Treatment of Adult Coats' Disease: A Case Report
- Macular Hole Following Intravitreal Ranibizumab Injections for Choroidal Neovascularization