Yonsei Med J.
2014 Mar;55(2):367-373.
Management of Bleeding Uterine Arteriovenous Malformation with Bilateral Uterine Artery Embolization
- Affiliations
-
- 1Department of Radiology, National Health Insurance Corporation Ilsan Hospital, Ilsan, Korea.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. jhshin@amc.seoul.kr
- 3Department of Radiology, Hanyang University College of Medicine, Hanyang University Guri Hospital, Guri, Korea.
Abstract
- PURPOSE
To evaluate the technical feasibility and clinical outcome of bilateral uterine artery embolization (UAE) as a first-line therapeutic option for bleeding uterine arteriovenous malformation (AVM).
MATERIALS AND METHODS
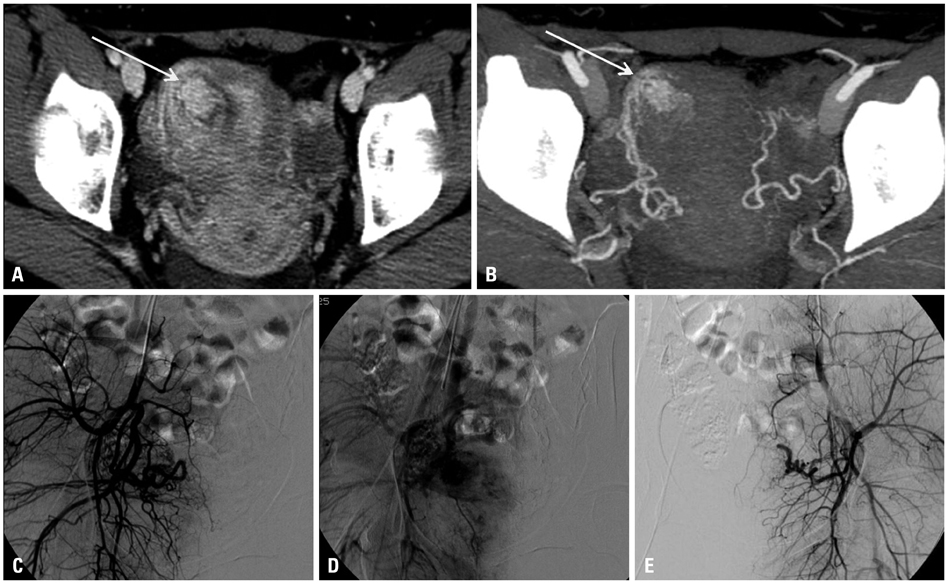
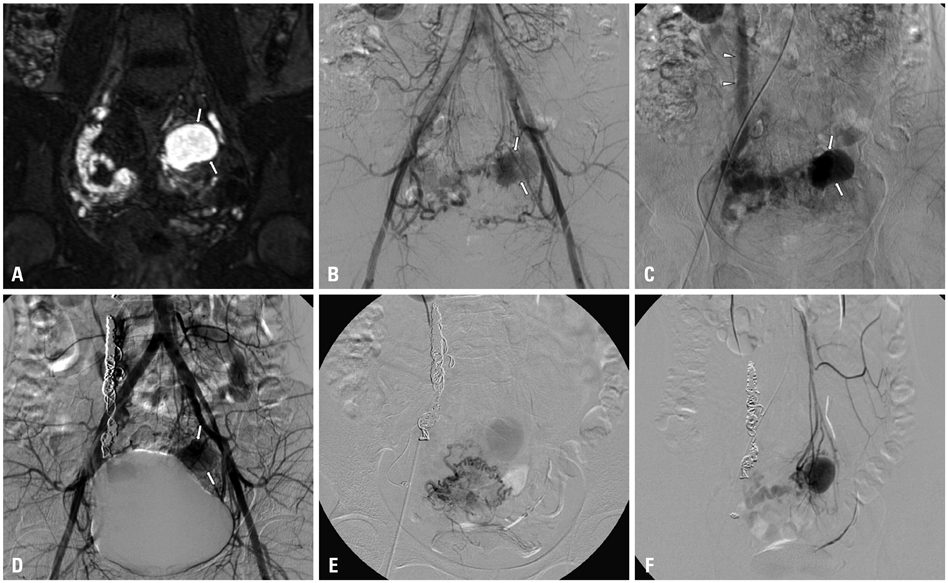
Between 2002 and 2012, 19 patients were diagnosed with acquired uterine AVM clinically and through imaging studies. The clinical characteristics, angiographic features, technical success rate of embolization, procedure-related complications, imaging, and clinical follow-up data were assessed. Clinical success was defined as immediate symptomatic resolution with disappearance of vascular abnormality on subsequent imaging studies.
RESULTS
A total of 20 bilateral UAE, with or without embolization of extra-uterine feeders, were performed as the first-line treatment. Technical and clinical success rate was 90.0% (18/20) and 89.5% (17/19), respectively. Embolization was incomplete in two patients who had residual extra-uterine fine feeders to the AVM or a procedure-related complication (ruptured uterine artery); the former showed slow regression of the vascular malformation during the observation period, while the latter underwent a successful second bilateral UAE. Immediate clinical success was achieved in the remaining 17 patients after a single session and no recurrence of bleeding was found. Recovery to normal menstrual cycle was seen in all 17 patients with clinical success within one or two months, two of whom subsequently had uneventful intrauterine pregnancies carried to term.
CONCLUSION
Bilateral UAE is a safe and effective first-line therapeutic option for the management of bleeding uterine AVMs. However, incomplete embolization due to unembolizable feeders or difficult access into the uterine artery may lead to suboptimal treatment.
MeSH Terms
Figure
Reference
-
1. Aziz N, Lenzi TA, Jeffrey RB Jr, Lyell DJ. Postpartum uterine arteriovenous fistula. Obstet Gynecol. 2004; 103(5 Pt 2):1076–1078.
Article2. Fleming H, Ostor AG, Pickel H, Fortune DW. Arteriovenous malformations of the uterus. Obstet Gynecol. 1989; 73:209–214.3. Flynn MK, Levine D. The noninvasive diagnosis and management of a uterine arteriovenous malformation. Obstet Gynecol. 1996; 88(4 Pt 2):650–652.
Article4. Cura M, Martinez N, Cura A, Dalsaso TJ, Elmerhi F. Arteriovenous malformations of the uterus. Acta Radiol. 2009; 50:823–829.
Article5. Arora R, Achla B, Pinkee S, Purba G, Bharti M. Arteriovenous malformations of the uterus. N Z Med J. 2004; 117:U1182.6. Schiller VL, Raft E, Linden R. Uterine arteriovenous malformation. AJR Am J Roentgenol. 1998; 170:219–220.
Article7. Timmerman D, Van den Bosch T, Peeraer K, Debrouwere E, Van Schoubroeck D, Stockx L, et al. Vascular malformations in the uterus: ultrasonographic diagnosis and conservative management. Eur J Obstet Gynecol Reprod Biol. 2000; 92:171–178.
Article8. O'Brien P, Neyastani A, Buckley AR, Chang SD, Legiehn GM. Uterine arteriovenous malformations: from diagnosis to treatment. J Ultrasound Med. 2006; 25:1387–1392.9. Brown JV 3rd, Asrat T, Epstein HD, Oglevie S, Goldstein BH. Contemporary diagnosis and management of a uterine arteriovenous malformation. Obstet Gynecol. 2008; 112(2 Pt 2):467–470.
Article10. Lin AC, Hung YC, Huang LC, Chiu TH, Ho M. Successful treatment of uterine arteriovenous malformation with percutaneous embolization. Taiwan J Obstet Gynecol. 2007; 46:60–63.
Article11. Lim AK, Agarwal R, Seckl MJ, Newlands ES, Barrett NK, Mitchell AW. Embolization of bleeding residual uterine vascular malformations in patients with treated gestational trophoblastic tumors. Radiology. 2002; 222:640–644.
Article12. Ghai S, Rajan DK, Asch MR, Muradali D, Simons ME, TerBrugge KG. Efficacy of embolization in traumatic uterine vascular malformations. J Vasc Interv Radiol. 2003; 14:1401–1408.
Article13. Amagada JO, Karanjgaokar V, Wood A, Wiener JJ. Successful pregnancy following two uterine artery embolisation procedures for arteriovenous malformation. J Obstet Gynaecol. 2004; 24:86–87.
Article14. Chia YN, Yap C, Tan BS. Pregnancy following embolisation of uterine arteriovenous malformation--a case report. Ann Acad Med Singapore. 2003; 32:658–660.15. Peitsidis P, Manolakos E, Tsekoura V, Kreienberg R, Schwentner L. Uterine arteriovenous malformations induced after diagnostic curettage: a systematic review. Arch Gynecol Obstet. 2011; 284:1137–1151.
Article16. Guo N, Liu H, Peng Z. Uterine arteriovenous fistula necessitating hysterectomy after two unsuccessful embolizations in an 18-year-old patient. Ann Vasc Surg. 2010; 24:827.
Article17. Wang Z, Chen J, Shi H, Zhou K, Sun H, Li X, et al. Efficacy and safety of embolization in iatrogenic traumatic uterine vascular malformations. Clin Radiol. 2012; 67:541–545.
Article18. Kwon JH, Kim GS. Obstetric iatrogenic arterial injuries of the uterus: diagnosis with US and treatment with transcatheter arterial embolization. Radiographics. 2002; 22:35–46.
Article19. Maleux G, Timmerman D, Heye S, Wilms G. Acquired uterine vascular malformations: radiological and clinical outcome after transcatheter embolotherapy. Eur Radiol. 2006; 16:299–306.
Article20. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S199–S202.
Article21. Vaknin Z, Sadeh-Mefpechkin D, Halperin R, Altshuler A, Amir P, Maymon R. Pregnancy-related uterine arteriovenous malformations: experience from a single medical center. Ultraschall Med. 2011; 32:Suppl 2. E92–E99.
Article22. Pelage JP, Walker WJ, Le Dref O, Rymer R. Ovarian artery: angiographic appearance, embolization and relevance to uterine fibroid embolization. Cardiovasc Intervent Radiol. 2003; 26:227–233.
Article23. Razavi MK, Wolanske KA, Hwang GL, Sze DY, Kee ST, Dake MD. Angiographic classification of ovarian artery-to-uterine artery anastomoses: initial observations in uterine fibroid embolization. Radiology. 2002; 224:707–712.
Article24. Dar P, Karmin I, Einstein MH. Arteriovenous malformations of the uterus: long-term follow-up. Gynecol Obstet Invest. 2008; 66:157–161.
Article25. Itoh H, Keitoku M, Fukuoka M, Sagawa N, Mori T, Togashi K. Spontaneous resolution of a postcesarean arteriovenous fistula of the uterine cervix: the usefulness of transvaginal color Doppler scanning. J Obstet Gynaecol Res. 1997; 23:439–444.
Article26. Forssman L, Lundberg J, Scherstén T. Conservative treatment of uterine arteriovenous fistula. Acta Obstet Gynecol Scand. 1982; 61:85–87.
Article27. Nonaka T, Yahata T, Kashima K, Tanaka K. Resolution of uterine arteriovenous malformation and successful pregnancy after treatment with a gonadotropin-releasing hormone agonist. Obstet Gynecol. 2011; 117(2 Pt 2):452–455.
Article28. Cho SK, Do YS, Shin SW, Kim DI, Kim YW, Park KB, et al. Arteriovenous malformations of the body and extremities: analysis of therapeutic outcomes and approaches according to a modified angiographic classification. J Endovasc Ther. 2006; 13:527–538.
Article29. Badawy SZ, Etman A, Singh M, Murphy K, Mayelli T, Philadelphia M. Uterine artery embolization: the role in obstetrics and gynecology. Clin Imaging. 2001; 25:288–295.30. Delotte J, Chevallier P, Benoit B, Castillon JM, Bongain A. Pregnancy after embolization therapy for uterine arteriovenous malformation. Fertil Steril. 2006; 85:228.
Article31. Chow TW, Nwosu EC, Gould DA, Richmond DH. Pregnancy following successful embolisation of a uterine vascular malformation. Br J Obstet Gynaecol. 1995; 102:166–168.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of angiography and transarterial embolization in arteriovenous malformation of uterus after a cesarean section episode
- Embolization of Uterine Arteriovenous Malformation
- Three Cases of Uterine Arteriovenous Malformation
- A Case of Successful Transarterial Embolization in Arteriovenous Malformation of Uterus
- Uterine arteriovenous malformation with repeated vaginal bleeding after dilatation and curettage