Yonsei Med J.
2014 Mar;55(2):345-352.
Prospective and Systematic Analysis of Unexpected Requests for Non-Cardiac Surgery or Other Invasive Procedures during the First Year after Drug-Eluting Stent Implantation
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. mkhong61@yuhs.ac
- 2Department of Cardiology, Wonju Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Cardiovascular Research Foundation, New York, NY, USA.
- 4Division of Cardiology, Severance Biomedical Science Institute, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
Unexpected requests for non-cardiac surgery requiring discontinuation of dual antiplatelet therapy (DAPT) frequently occur in daily clinical practice. The objectives of this study were to evaluate prevalence, timing and clinical outcomes of such unexpected requests for non-cardiac surgery or other invasive procedures during the first year after drug-eluting stents (DESs) implantation.
MATERIALS AND METHODS
We prospectively investigated the prevalence, timing and clinical outcomes of unexpected requests for non-cardiac surgery or other procedures during the first year after DESs implantation in 2117 patients.
RESULTS
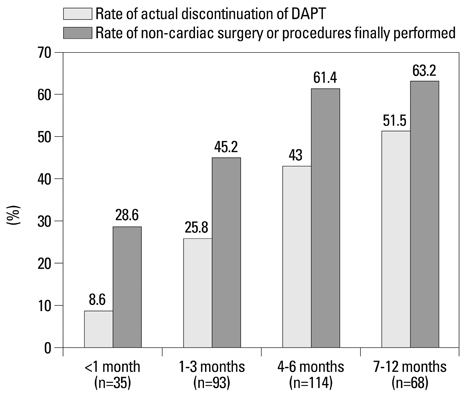
The prevalence of requested non-cardiac surgery or invasive procedures was 14.6% in 310 requests and 12.3% in 261 patients. Among 310 requests, those were proposed in 11.3% <1 month, 30.0% between 1 and 3 months, 36.8% between 4 and 6 months and 21.9% between 7 and 12 months post-DES implantation. The rates of actual discontinuation of DAPT and non-cardiac surgery or procedure finally performed were 35.8% (111 of 310 requests) and 53.2% (165 of 310 requests), respectively. On multivariate regression analysis, the most significant determinants for actual discontinuation of DAPT were Endeavor zotarolimus-eluting stent implantation with 3-month DAPT (OR=5.54, 95% CI 2.95-10.44, p<0.001) and timing of request (OR=2.84, 95% CI 1.97-4.11, p<0.001). There were no patients with any death, myocardial infarction, or stent thrombosis related with actual discontinuation of DAPT.
CONCLUSION
Those unexpected requests with premature discontinuation of DAPT were relatively common and continuously proposed during the first year following DES implantation. No death, myocardial infarction or stent thrombosis occurred in patients with actual discontinuation of DAPT.
MeSH Terms
Figure
Reference
-
1. Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005; 293:2126–2130.
Article2. Spertus JA, Kettelkamp R, Vance C, Decker C, Jones PG, Rumsfeld JS, et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation. 2006; 113:2803–2809.
Article3. Pfisterer M, Brunner-La Rocca HP, Buser PT, Rickenbacher P, Hunziker P, Mueller C, et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. J Am Coll Cardiol. 2006; 48:2584–2591.
Article4. Brar SS, Kim J, Brar SK, Zadegan R, Ree M, Liu IL, et al. Long-term outcomes by clopidogrel duration and stent type in a diabetic population with de novo coronary artery lesions. J Am Coll Cardiol. 2008; 51:2220–2227.
Article5. Ferreira-González I, Marsal JR, Ribera A, Permanyer-Miralda G, García-Del Blanco B, Martí G, et al. Background, incidence, and predictors of antiplatelet therapy discontinuation during the first year after drug-eluting stent implantation. Circulation. 2010; 122:1017–1025.
Article6. Grines CL, Bonow RO, Casey DE Jr, Gardner TJ, Lockhart PB, Moliterno DJ, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Circulation. 2007; 115:813–818.
Article7. Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007; 116:1971–1996.
Article8. Kim BK, Hong MK, Shin DH, Nam CM, Kim JS, Ko YG, et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol. 2012; 60:1340–1348.9. Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery. European Society of Cardiology (ESC). Poldermans D, Bax JJ, Boersma E, De Hert S, et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J. 2009; 30:2769–2812.
Article10. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.11. Kałuza GL, Joseph J, Lee JR, Raizner ME, Raizner AE. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol. 2000; 35:1288–1294.
Article12. Brilakis ES, Cohen DJ, Kleiman NS, Pencina M, Nassif D, Saucedo J, et al. Incidence and clinical outcome of minor surgery in the year after drug-eluting stent implantation: results from the Evaluation of Drug-Eluting Stents and Ischemic Events Registry. Am Heart J. 2011; 161:360–366.
Article13. Schouten O, van Domburg RT, Bax JJ, de Jaegere PJ, Dunkelgrun M, Feringa HH, et al. Noncardiac surgery after coronary stenting: early surgery and interruption of antiplatelet therapy are associated with an increase in major adverse cardiac events. J Am Coll Cardiol. 2007; 49:122–124.
Article14. Anwaruddin S, Askari AT, Saudye H, Batizy L, Houghtaling PL, Alamoudi M, et al. Characterization of post-operative risk associated with prior drug-eluting stent use. JACC Cardiovasc Interv. 2009; 2:542–549.
Article15. Kim JS, Jang IK, Fan C, Kim TH, Kim JS, Park SM, et al. Evaluation in 3 months duration of neointimal coverage after zotarolimus-eluting stent implantation by optical coherence tomography: the ENDEAVOR OCT trial. JACC Cardiovasc Interv. 2009; 2:1240–1247.
Article16. Lee SY, Hong M. Stent evaluation with optical coherence tomography. Yonsei Med J. 2013; 54:1075–1083.
Article17. Stone GW, Rizvi A, Newman W, Mastali K, Wang JC, Caputo R, et al. Everolimus-eluting versus paclitaxel-eluting stents in coronary artery disease. N Engl J Med. 2010; 362:1663–1674.
Article18. Meredith IT, Worthley S, Whitbourn R, Walters DL, McClean D, Horrigan M, et al. Clinical and angiographic results with the next-generation resolute stent system: a prospective, multicenter, first-in-human trial. JACC Cardiovasc Interv. 2009; 2:977–985.
Article19. Berger PB, Kleiman NS, Pencina MJ, Hsieh WH, Steinhubl SR, Jeremias A, et al. Frequency of major noncardiac surgery and subsequent adverse events in the year after drug-eluting stent placement results from the EVENT (Evaluation of Drug-Eluting Stents and Ischemic Events) Registry. JACC Cardiovasc Interv. 2010; 3:920–927.
Article20. To AC, Armstrong G, Zeng I, Webster MW. Noncardiac surgery and bleeding after percutaneous coronary intervention. Circ Cardiovasc Interv. 2009; 2:213–221.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Stent Thrombosis Occurred at 5 Years after Sirolimus-Eluting Stent Implantation
- Systemic drug therapy and restenosis after drug-eluting stent implantation
- Very Late Stent Thrombosis Related to Fracture of a Sirolimus-Eluting Stent
- A Case of Stent Strut Fracture of a Paclitaxel-Eluting Stent at the Time of Stent Implantation in a Complex Coronary Lesion
- Percutaneous Treatment of an Injured Coronary Stent Using the Looping Wire Technique