J Korean Med Sci.
2017 Sep;32(9):1552-1557. 10.3346/jkms.2017.32.9.1552.
Multidisciplinary Approach to Refractory Upper Gastrointestinal Bleeding: Case Series of Angiographic Embolization
- Affiliations
-
- 1Department of Internal Medicine, Ewha Medical Research Institute, Ewha Womans University School of Medicine, Seoul, Korea. shimkn@ewha.ac.kr
- 2Department of Health Promotion Medicine, Ewha Medical Research Institute, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Radiology, Ewha Medical Research Institute, Ewha Womans University School of Medicine, Seoul, Korea.
- KMID: 2385965
- DOI: http://doi.org/10.3346/jkms.2017.32.9.1552
Abstract
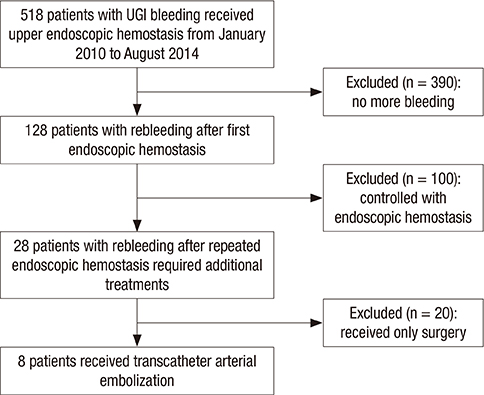
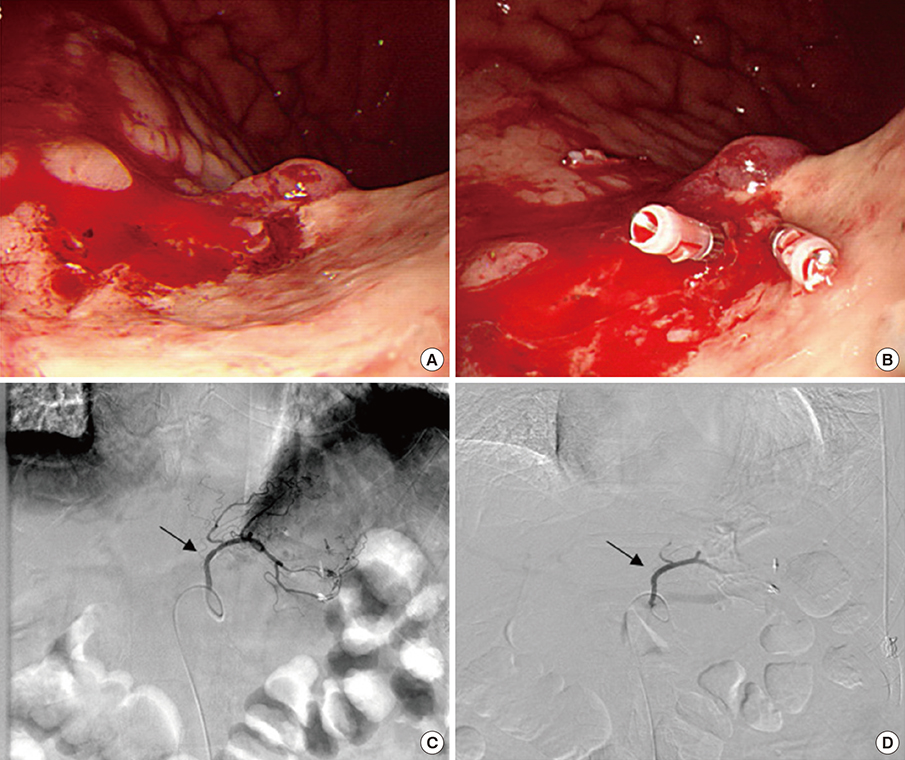
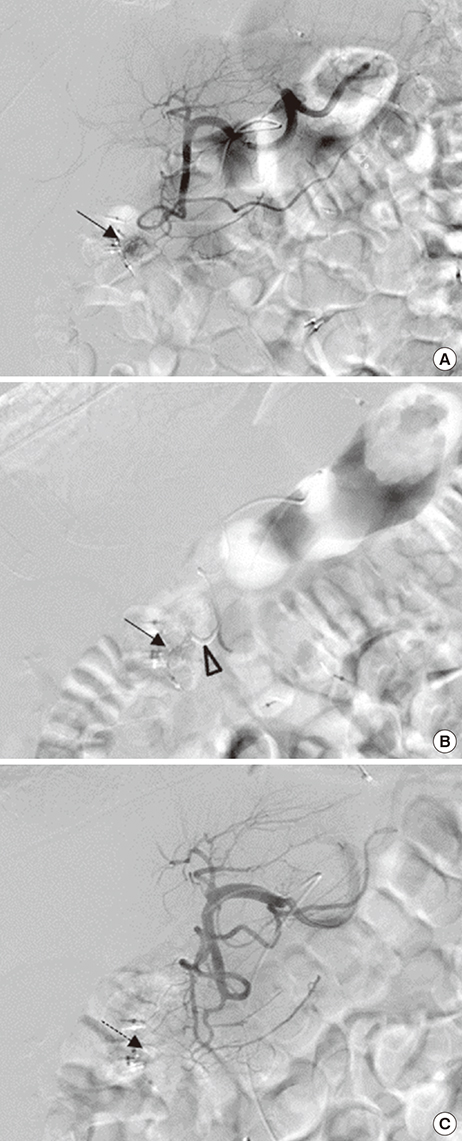
- Although medical and endoscopic hemostasis is now considered as the first-line therapy for nonvariceal upper gastrointestinal (UGI) bleeding, refractory bleeding still occurs in 5%-10% of the patients. In these patients, transcatheter arterial embolization (TAE) or surgery is required, but research on embolization for unmanageable UGI bleeding in Korea is scanty. We reviewed the medical records of 518 patients who underwent endoscopic hemostasis during 4 years. Among these subjects, 8 patients who required embolization due to failure of endoscopic hemostasis were enrolled. Mean patient age was 74.00 ± 8.25 years, and rebleeding occurred in 4 patients within 48 hours after TAE. Three patients with duodenal rebleeding underwent surgery, and the other patient with a gastric ulcer underwent endoscopic hemostasis. Nonvariceal UGI bleeding remains a serious clinical challenge, especially in older patients. A multidisciplinary approach including endoscopists, interventional radiologists, and surgeons may be important for the treatment of nonvariceal UGI bleeding.
MeSH Terms
Figure
Reference
-
1. Gralnek IM, Barkun AN, Bardou M. Management of acute bleeding from a peptic ulcer. N Engl J Med. 2008; 359:928–937.2. Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK: patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011; 60:1327–1335.3. Esrailian E, Gralnek IM. Nonvariceal upper gastrointestinal bleeding: epidemiology and diagnosis. Gastroenterol Clin North Am. 2005; 34:589–605.4. Yachimski PS, Friedman LS. Gastrointestinal bleeding in the elderly. Nat Clin Pract Gastroenterol Hepatol. 2008; 5:80–93.5. Bae S, Kim N, Kang JM, Kim DS, Kim KM, Cho YK, Kim JH, Jung SW, Shim KN. Incidence and 30-day mortality of peptic ulcer bleeding in Korea. Eur J Gastroenterol Hepatol. 2012; 24:675–682.6. Hong MJ, Lee SY, Kim JH, Sung IK, Park HS, Shim CS, Jin CJ. Rebleeding after initial endoscopic hemostasis in peptic ulcer disease. J Korean Med Sci. 2014; 29:1411–1415.7. Lee YJ, Kim ES, Hah YJ, Park KS, Cho KB, Jang BK, Chung WJ, Hwang JS. Chronic kidney disease, hemodynamic instability, and endoscopic high-risk appearance are associated with 30-day rebleeding in patients with non-variceal upper gastrointestinal bleeding. J Korean Med Sci. 2013; 28:1500–1506.8. Spiegel BM, Vakil NB, Ofman JJ. Endoscopy for acute nonvariceal upper gastrointestinal tract hemorrhage: is sooner better? A systematic review. Arch Intern Med. 2001; 161:1393–1404.9. Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC. Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion. 2011; 84:102–113.10. Suk KT, Kim HS, Lee CS, Lee IY, Kim MY, Kim JW, Baik SK, Kwon SO, Lee DK, Ham YL. Clinical outcomes and risk factors of rebleeding following endoscopic therapy for nonvariceal upper gastrointestinal hemorrhage. Clin Endosc. 2011; 44:93–100.11. Lee HH, Park JM, Chun HJ, Oh JS, Ahn HJ, Choi MG. Transcatheter arterial embolization for endoscopically unmanageable non-variceal upper gastrointestinal bleeding. Scand J Gastroenterol. 2015; 50:809–815.12. Loffroy R, Estivalet L, Cherblanc V, Sottier D, Guiu B, Cercueil JP, Krausé D. Transcatheter embolization as the new reference standard for endoscopically unmanageable upper gastrointestinal bleeding. World J Gastrointest Surg. 2012; 4:223–227.13. Guglielmi A, Ruzzenente A, Sandri M, Kind R, Lombardo F, Rodella L, Catalano F, de Manzoni G, Cordiano C. Risk assessment and prediction of rebleeding in bleeding gastroduodenal ulcer. Endoscopy. 2002; 34:778–786.14. Shin JH. Recent update of embolization of upper gastrointestinal tract bleeding. Korean J Radiol. 2012; 13:Suppl 1. S31–S39.15. Shin JH. Refractory gastrointestinal bleeding: role of angiographic intervention. Clin Endosc. 2013; 46:486–491.16. Ang D, Teo EK, Tan A, Ibrahim S, Tan PS, Ang TL, Fock KM. A comparison of surgery versus transcatheter angiographic embolization in the treatment of nonvariceal upper gastrointestinal bleeding uncontrolled by endoscopy. Eur J Gastroenterol Hepatol. 2012; 24:929–938.17. Wong TC, Wong KT, Chiu PW, Teoh AY, Yu SC, Au KW, Lau JY. A comparison of angiographic embolization with surgery after failed endoscopic hemostasis to bleeding peptic ulcers. Gastrointest Endosc. 2011; 73:900–908.18. Venclauskas L, Bratlie SO, Zachrisson K, Maleckas A, Pundzius J, Jönson C. Is transcatheter arterial embolization a safer alternative than surgery when endoscopic therapy fails in bleeding duodenal ulcer? Scand J Gastroenterol. 2010; 45:299–304.19. Mirsadraee S, Tirukonda P, Nicholson A, Everett SM, McPherson SJ. Embolization for non-variceal upper gastrointestinal tract haemorrhage: a systematic review. Clin Radiol. 2011; 66:500–509.20. Schenker MP, Duszak R Jr, Soulen MC, Smith KP, Baum RA, Cope C, Freiman DB, Roberts DA, Shlansky-Goldberg RD. Upper gastrointestinal hemorrhage and transcatheter embolotherapy: clinical and technical factors impacting success and survival. J Vasc Interv Radiol. 2001; 12:1263–1271.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes and complications of embolization for gastrointestinal bleeding
- Refractory Gastrointestinal Bleeding: Role of Angiographic Intervention
- Recent Update of Embolization of Upper Gastrointestinal Tract Bleeding
- Angiographic Embokization in the Control of Bleeding Related to Gynecologic Malignancy
- Transcatheter Arterial Embolization of Nonvariceal Upper Gastrointestinal Bleeding with N-Butyl Cyanoacrylate