J Korean Soc Spine Surg.
2017 Jun;24(2):95-102. 10.4184/jkss.2017.24.2.95.
Can Unilateral Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF) Result in Sufficient Reduction in Spondylolisthesis?: A Comparison with Open TLIF and Bilateral MIS TLIF
- Affiliations
-
- 1Department of Orthopedic Surgery, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea. drkookh@gmail.com
- KMID: 2385645
- DOI: http://doi.org/10.4184/jkss.2017.24.2.95
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
To compare the radiologic results of unilateral or bilateral minimal invasive transforaminal lumbar interbody fusion (MIS TLIF) and conventional open lumbar interbody fusion. SUMMARY OF LITERATURE REVIEW: Only a few studies have compared the slip reduction and fusion rate between unilateral or bilateral MIS TLIF and conventional open TLIF.
MATERIALS AND METHODS
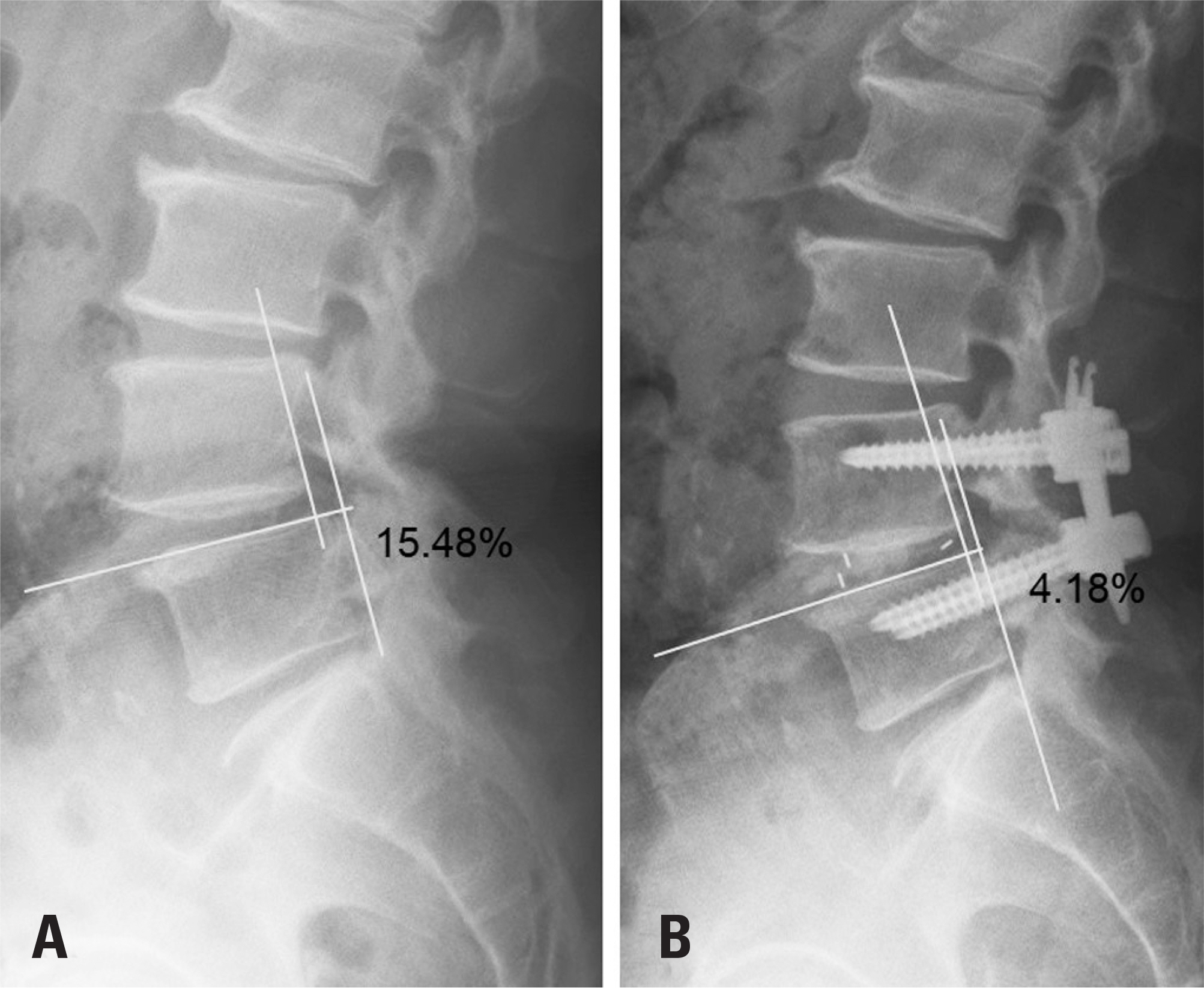
Between March 2007 and May 2015, 80 patients with single-level low-grade spondylolisthesis underwent unilateral MIS TLIF (26 patients), bilateral MIS TLIF (10 patients), or open TLIF (44 patients) by a single surgeon. Radiologic studies were performed preoperatively, 2 weeks postoperatively, and 12 months postoperatively. Slip reduction, the lumbar lordortic angle, and the fusion rate were analyzed.
RESULTS
The 3 groups exhibited significantly improved slip after operation. Significant differences were found among the 3 groups (p=0.015) and between the MIS TLIF group (31.76%±14.42%) and the open TLIF group (41.66%±15.98%) (p=0.01) in the slip reduction rate at 2 weeks after the operation. However, no significant difference was found between unilateral MIS TLIF and bilateral MIS TLIF (37.61%±15.0% vs. 29.5%±13.82%, p=0.148). In the lumbar lordotic angle, no significant difference was found among the 3 groups. There were no significant differences among the 3 groups in slip reduction or the fusion rate at 12 months after the operation.
CONCLUSIONS
Our study suggests that unilateral MIS TLIF showed a similar slip reduction and fusion rate to bilateral MIS TLIF, but that conventional open TLIF showed better slip reduction than MIS TLIF, although it had a similar fusion rate.
Keyword
Figure
Reference
-
1. Yan DL, Pei FX, Li J, et al. Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J. 2008; 17:1311–6.
Article2. Park P, Foley KT. Minimally invasive transforaminal lumbar interbody fusion with reduction of spondylolisthesis: technique and outcomes after a minimum of 2 years’ follow-up. Neurosurg Focus. 2008; 25:E16.
Article3. Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech. 2005; 18(Suppl):1–6.4. Holly LT, Schwender JD, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus. 2006; 20:E6.5. Park Y, Ha JW, Lee YT, et al. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis and degenerative spondylosis: 5-year results. Clin Orthop Relat Res. 2014; 472:1813–23.
Article6. Park Y, Ha JW, Lee YT, et al. Surgical outcomes of minimally invasive transforaminal lumbar interbody fusion for the treatment of spondylolisthesis and degenerative segmental instability. Asian Spine J. 2011; 5:228–36.
Article7. Barbagallo GM, Piccini M, Alobaid A, et al. Bilateral tubular minimally invasive surgery for low-dysplastic lumbosacral lytic spondylolisthesis (LDLLS): analysis of a series focusing on postoperative sagittal balance and review of the literature. Eur Spine J. 2014; 23(Suppl):705–13.
Article8. Barbagallo GM, Certo F, Sciacca G, Albanese V. Bilateral tubular minimally invasive approach for decompression, reduction and fixation in lumbosacral lythic spondylolisthesis. Neurosurg Focus. 2013; 35(Suppl):): Video 9.
Article9. Oh CH, Ji GY, Jeon JK, et al. Slip reduction rate between minimal invasive and conventional unilateral transforaminal interbody fusion in patients with low-grade isthmic spondylolisthesis. Korean J Spine. 2013; 10:232–6.
Article10. Min SH, Lee DH. Minimally Invasive transforaminal lumbar interbody fusion in patients with low grade spon-dylolisthesis: Comparison of the unilateral and bilateral approaches. J Korean Orthop Assoc. 2009; 44:429–35.11. Burkus JK, Foley K, Haid RW, et al. Surgical interbody research group-radiographic assessment of interbody fusion devices: fusion criteria for anterior lumbar interbody surgery. Neurosurg Focus. 2001; 10:E11.
Article12. Pan J, Li L, Qian L, et al. Spontaneous slip reduction of low-grade isthmic spondylolisthesis following circumfer-ential release via bilateral minimally invasive transforaminal lumbar interbody fusion: technical note and short-term outcome. Spine (Phila Pa 1972). 2011; 36:283–9.13. Tsahtsarlis A, Wood M. Minimally invasive transforaminal lumbar interbody fusion and spondylolisthesis. J Clin Neu-rosci. 2012; 19:858–61.
Article14. Tay KS, Bassi A, Yeo W, et al. Intraoperative reduction does not result in better outcomes in low-grade lumbar spon-dylolisthesis with neurogenic symptoms after minimally invasive transforaminal lumbar interbody fusion-a 5-year follow-up study. Spine J. 2016; 16:182–90.
Article15. Wegmann K, Gundermann S, Siewe J, et al. Correlation of reduction and clinical outcome in patients with degenerative spondylolisthesis. Arch Orthop Trauma Surg. 2013; 133:1639–44.
Article16. Benli IT, Ciç ek H, Kaya A. Comparison of sagittal plane realignment and reduction with posterior instrumentation in developmental low or high dysplastic spondylolisthesis. Kobe J Med Sci. 2006; 52:151–69.17. Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery. 2007; 60(Suppl):203–12.
Article18. Wang J, Zhou Y, Zhang ZF, et al. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010; 19:1780–4.
Article19. Wu RH, Fraser JF, Hä rtl R. Minimal access versus open transforaminal lumbar interbody fusion: meta-analysis of fusion rates. Spine (Phila Pa 1972). 2010; 35:2273–81.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biportal Endoscopic Transforaminal Lumbar Interbody Fusion with Arthroscopy
- Radiographic Results of Minimally Invasive (MIS) Lumbar Interbody Fusion (LIF) Compared with Conventional Lumbar Interbody Fusion
- Minimally Invasive Transforaminal Lumbar Interbody Fusion with the Space-D Access System
- History and Evolution of the Minimally Invasive Transforaminal Lumbar Interbody Fusion
- The Technical Feasibility of Unilateral Biportal Endoscopic Decompression for The Unpredicted Complication Following Minimally Invasive Transforaminal Lumbar Interbody Fusion: Case Report