Korean J Pain.
2017 Jul;30(3):176-182. 10.3344/kjp.2017.30.3.176.
Intravenous caffeine citrate vs. magnesium sulfate for reducing pain in patients with acute migraine headache; a prospective quasi-experimental study
- Affiliations
-
- 1Department of Emergency Medicine, Tehran University of Medical Sciences, Tehran, Iran.
- 2Department of Emergency Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 3Department of Neurology, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
- 4Faculty of Medicine, Al Azhar University, Cairo, Egypt.
- 5Medical Research Group of Egypt, El-Sharkia, Egypt. ahmed01251@medicine.zu.edu.eg
- 6Faculty of Medicine, Zagazig University, El-Sharkia, Egypt.
- KMID: 2385349
- DOI: http://doi.org/10.3344/kjp.2017.30.3.176
Abstract
- BACKGROUND
Current evidence suggests that intravenous magnesium sulfate might be effective for reducing migraine pain. In a recent pilot study, we showed that intravenous caffeine citrate could reduce the severity of migraine headache. The objective of this study is to investigate the efficacy of intravenous caffeine citrate vs. magnesium sulfate for management of acute migraine headache.
METHODS
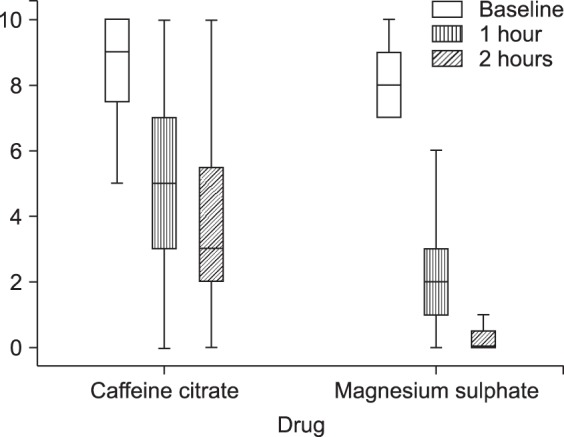
We conducted a prospective quasi-experimental study from January until May 2016 in two educational medical centers of Shahid Beheshti University of Medical Sciences (Shoahadaye Tajrish Hospital and Imam Hossein Hospital), Tehran, Iran. The study included patients who were referred to the emergency department and met the migraine diagnosis criteria of the International Headache Society. Patients were allocated into 2 groups receiving either 60 mg intravenous caffeine or 2 g intravenous magnesium sulfate. The pain scores, based on the visual analog scale, were recorded on admission, as well as one and two hours after receiving the drug. A Chi-Square test and student t-test were used for analysis of baseline characteristics. A Mann-Whitney U test and Wilcoxon singed rank test were used to analyze differences in the visual analogue scale (VAS) score between and within the groups respectively.
RESULTS
In total, 70 patients (35 patients in each group) with the mean age of 33.1 ± 11.3 years were included (64.3% female). For the Caffeine citrate group, the median pain score decreased from 9.0 (2.0) to 5.0 (4.0) after one hour and to 3.0 (4.0) after two hours. For the magnesium sulfate group, the pain score decreased from 8.0 (2.0) to 2.0 (2.0) after one hour and to 0.0 (1.0) after two hours. Both intravenous caffeine citrate and intravenous magnesium sulfate reduced pain scores significantly but the magnesium sulfate group showed more improvement than the Caffeine citrate group after one hour (P < 0.001) and after two hours (P < 0.001).
CONCLUSIONS
It is likely that both intravenous caffeine and intravenous magnesium sulfate can reduce the severity of migraine headache. Moreover, intravenous magnesium sulfate at a dose of 2 g might be superior to intravenous caffeine citrate 60 mg for the short term management of migraine headache in emergency departments.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Perampanel ameliorates nitroglycerin-induced migraine through inhibition of the cAMP/PKA/CREB signaling pathway in the trigeminal ganglion in rats
QingLing Zhai, KaiXin Wang, Defu Zhang, Jinbo Chen, XiaoMeng Dong, Yonghui Pan
Korean J Pain. 2023;36(3):335-346. doi: 10.3344/kjp.23039.
Reference
-
1. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013; 33:629–808. PMID: 23771276.2. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the american headache society evidence assessment of migraine pharmacotherapies. Headache. 2015; 55:3–20. PMID: 25600718.
Article3. Prior MJ, Codispoti JR, Fu M. A randomized, placebo-controlled trial of acetaminophen for treatment of migraine headache. Headache. 2010; 50:819–833. PMID: 20236342.
Article4. Lipton RB, Baggish JS, Stewart WF, Codispoti JR, Fu M. Efficacy and safety of acetaminophen in the treatment of migraine: results of a randomized, double-blind, placebo-controlled, population-based study. Arch Intern Med. 2000; 160:3486–3492. PMID: 11112243.
Article5. Becker WJ. Acute migraine treatment in adults. Headache. 2015; 55:778–793. PMID: 25877672.
Article6. Suthisisang C, Poolsup N, Kittikulsuth W, Pudchakan P, Wiwatpanich P. Efficacy of low-dose ibuprofen in acute migraine treatment: systematic review and meta-analysis. Ann Pharmacother. 2007; 41:1782–1791. PMID: 17878396.
Article7. Boska MD, Welch KM, Barker PB, Nelson JA, Schultz L. Contrasts in cortical magnesium, phospholipid and energy metabolism between migraine syndromes. Neurology. 2002; 58:1227–1233. PMID: 11971091.
Article8. Mauskop A, Altura BT, Altura BM. Serum ionized magnesium levels and serum ionized calcium/ionized magnesium ratios in women with menstrual migraine. Headache. 2002; 42:242–248. PMID: 12010379.
Article9. Trauninger A, Pfund Z, Koszegi T, Czopf J. Oral magnesium load test in patients with migraine. Headache. 2002; 42:114–119. PMID: 12005285.
Article10. Cete Y, Dora B, Ertan C, Ozdemir C, Oktay C. A randomized prospective placebo-controlled study of intravenous magnesium sulphate vs. metoclopramide in the management of acute migraine attacks in the emergency department. Cephalalgia. 2005; 25:199–204. PMID: 15689195.
Article11. Demirkaya S, Vural O, Dora B, Topçuoğlu MA. Efficacy of intravenous magnesium sulfate in the treatment of acute migraine attacks. Headache. 2001; 41:171–177. PMID: 11251702.
Article12. Bigal ME, Bordini CA, Tepper SJ, Speciali JG. Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. Cephalalgia. 2002; 22:345–353. PMID: 12110110.
Article13. Corbo J, Esses D, Bijur PE, Iannaccone R, Gallagher EJ. Randomized clinical trial of intravenous magnesium sulfate as an adjunctive medication for emergency department treatment of migraine headache. Ann Emerg Med. 2001; 38:621–627. PMID: 11719739.
Article14. Köseoglu E, Talaslioglu A, Gönül AS, Kula M. The effects of magnesium prophylaxis in migraine without aura. Magnes Res. 2008; 21:101–108. PMID: 18705538.15. Teigen L, Boes CJ. An evidence-based review of oral magnesium supplementation in the preventive treatment of migraine. Cephalalgia. 2015; 35:912–922. PMID: 25533715.
Article16. Baratloo A, Rouhipour A, Forouzanfar MM, Safari S, Amiri M, Negida A. The role of caffeine in pain management: a brief literature review. Anesth Pain Med. 2016; 6:e33193. PMID: 27642573.
Article17. Diener HC, Pfaffenrath V, Pageler L, Peil H, Aicher B. The fixed combination of acetylsalicylic acid, paracetamol and caffeine is more effective than single substances and dual combination for the treatment of headache: a multicentre, randomized, double-blind, single-dose, placebo-controlled parallel group study. Cephalalgia. 2005; 25:776–787. PMID: 16162254.
Article18. Goldstein J, Silberstein SD, Saper JR, Ryan RE Jr, Lipton RB. Acetaminophen, aspirin, and caffeine in combination versus ibuprofen for acute migraine: results from a multicenter, double-blind, randomized, parallel-group, single-dose, placebo-controlled study. Headache. 2006; 46:444–453. PMID: 16618262.
Article19. Silberstein SD, Winner PK, Chmiel JJ. Migraine preventive medication reduces resource utilization. Headache. 2003; 43:171–178. PMID: 12603635.
Article20. Baratloo A, Bafarani SA, Forouzanfar MM, Hashemi B, Friedman BW, Abdalvand A. Intravenous caffeine versus intravenous ketorolac for the management of moderate to severe migraine headache. Bangladesh J Pharmacol. 2016; 11:428–432.
Article21. Baratloo A, Negida A, El-Ashal G, Behnaz N. Intravenous caffeine for the treatment of acute migraine: a pilot study. J Caffeine Res. 2015; 5:125–129.
Article22. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011; 63(Suppl 11):S240–S252. PMID: 22588748.23. Alschuler KN, Jensen MP, Ehde DM. Defining mild, moderate, and severe pain in persons with multiple sclerosis. Pain Med. 2012; 13:1358–1365. PMID: 22925457.
Article24. Zelman DC, Dukes E, Brandenburg N, Bostrom A, Gore M. Identification of cut-points for mild, moderate and severe pain due to diabetic peripheral neuropathy. Pain. 2005; 115:29–36. PMID: 15836967.
Article25. Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001; 18:205–207. PMID: 11354213.
Article26. Ray BS, Wolff HG. Experimental studies on headache: pain-sensitive structures of the head and their significance in headache. Arch Surg. 1940; 41:813–856.27. Silberstein SD, Lipton RB, Dalessio DJ. Wolff's headache and other head pain. 7th ed. New York (NY): Oxford University Press;2001. p. 606.28. Lance JW, Goadsby PJ. Chapter 8: migraine: pathophysiology. In : Lance JW, Goadsby PJ, editors. Mechanism and management of headache. 7th ed. Oxford: Elsevier Butterworth-Heinemann;2005. p. 87–121.29. Silberstein SD, Lipton RB, Goadsby PJ. Headache in clinical practice. Oxford: Isis Medical Media;1998. p. 250.30. Ashina S, Bendtsen L, Ashina M. Pathophysiology of migraine and tension-type headache. Tech Reg Anesth Pain Manag. 2012; 16:14–18.
Article31. Pietrobon D, Moskowitz MA. Pathophysiology of migraine. Annu Rev Physiol. 2013; 75:365–391. PMID: 23190076.
Article32. Olesen J, Friberg L, Olsen TS, Iversen HK, Lassen NA, Andersen AR, et al. Timing and topography of cerebral blood flow, aura, and headache during migraine attacks. Ann Neurol. 1990; 28:791–798. PMID: 2285266.
Article33. Bolay H, Reuter U, Dunn AK, Huang Z, Boas DA, Moskowitz MA. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat Med. 2002; 8:136–142. PMID: 11821897.
Article34. Goadsby PJ, Lipton RB, Ferrari MD. Migraine--current understanding and treatment. N Engl J Med. 2002; 346:257–270. PMID: 11807151.35. Tepper SJ. Complementary and alternative treatments for childhood headaches. Curr Pain Headache Rep. 2008; 12:379–383. PMID: 18765145.
Article36. Taylor FR. Nutraceuticals and headache: the biological basis. Headache. 2011; 51:484–501. PMID: 21352223.
Article37. Bhaskar S, Saeidi K, Borhani P, Amiri H. Recent progress in migraine pathophysiology: role of cortical spreading depression and magnetic resonance imaging. Eur J Neurosci. 2013; 38:3540–3551. PMID: 24118449.
Article38. Eikermann-Haerter K, Ayata C. Cortical spreading depression and migraine. Curr Neurol Neurosci Rep. 2010; 10:167–173. PMID: 20425031.
Article39. D'Andrea G, Leon A. Pathogenesis of migraine: from neurotransmitters to neuromodulators and beyond. Neurol Sci. 2010; 31(Suppl 1):S1–S7. PMID: 20464574.40. Levy D. Migraine pain and nociceptor activation--where do we stand? Headache. 2010; 50:909–916. PMID: 20546325.
Article41. Olesen J, Burstein R, Ashina M, Tfelt-Hansen P. Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurol. 2009; 8:679–690. PMID: 19539239.
Article42. Pietrobon D, Striessnig J. Neurobiology of migraine. Nat Rev Neurosci. 2003; 4:386–398. PMID: 12728266.
Article43. Dunwiddie TV, Masino SA. The role and regulation of adenosine in the central nervous system. Annu Rev Neurosci. 2001; 24:31–55. PMID: 11283304.
Article44. Scher AI, Lipton RB, Stewart W. Risk factors for chronic daily headache. Curr Pain Headache Rep. 2002; 6:486–491. PMID: 12413408.
Article45. Tavares C, Sakata RK. Caffeine in the treatment of pain. Rev Bras Anestesiol. 2012; 62:387–401. PMID: 22656684.
Article46. Chiu HY, Yeh TH, Huang YC, Chen PY. Effects of intravenous and oral magnesium on reducing migraine: a meta-analysis of randomized controlled trials. Pain Physician. 2016; 19:E97–E112. PMID: 26752497.47. Bolay H, Ozge A, Saginc P, Orekici G, Uludüz D, Yalın O, et al. Gender influences headache characteristics with increasing age in migraine patients. Cephalalgia. 2015; 35:792–800. PMID: 25424708.
Article48. Vallerand AH, Polomano RC. The relationship of gender to pain. Pain Manag Nurs. 2000; 1:8–15. PMID: 11710147.
Article49. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009; 10:447–485. PMID: 19411059.
Article50. Fillingim RB. Sex, gender, and pain: women and men really are different. Curr Rev Pain. 2000; 4:24–30. PMID: 10998712.
Article51. Yezierski RP. The effects of age on pain sensitivity: preclinical studies. Pain Med. 2012; 13(Suppl 2):S27–S36. PMID: 22497745.
Article52. El Tumi H, Johnson MI, Dantas PB, Maynard MJ, Tashani OA. Age-related changes in pain sensitivity in healthy humans: a systematic review with meta-analysis. Eur J Pain. 2017; 21:955–964. PMID: 28230292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparison of ritodrine and magnesium sulfate for the suppression of preterm labor
- Magnesium: a versatile drug for anesthesiologists
- Preemptive Analgesic Effect of Magnesium Sulfate on Postoperative Pain in Patients Undergoing Gastrectomy
- Effect of intravenous magnesium on postoperative pain control for major abdominal surgery: a randomized double-blinded study
- Magnesium Sulfate in the Treatment of Torsade De Pointes