J Cardiovasc Ultrasound.
2017 Jun;25(2):47-56. 10.4250/jcu.2017.25.2.47.
Effects of Decreased Annular Height and Annular Saddle-Shaped Non-Planarity in Degenerative Severe Mitral Regurgitation with Normal Left Ventricular Ejection Fraction: Real-Time 3D Transesophageal Echocardiography
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Cardiovascular Imaging Center, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. tyche.park@gmail.com
- 2Division of Cardiology, Department of Internal Medicine, National Cancer Center, Goyang, Korea.
- 3Department of Thoracic Surgery, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2385075
- DOI: http://doi.org/10.4250/jcu.2017.25.2.47
Abstract
- BACKGROUND
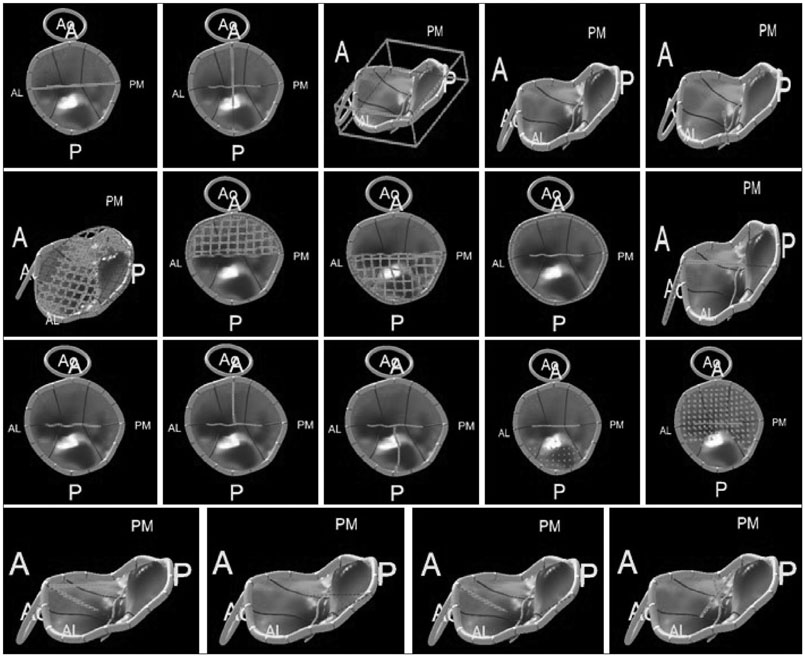
The extent of mitral annular (MA) remodeling and dysfunction is correlated with the severity of mitral regurgitation (MR) as well as left atrial (LA) and left ventricular (LV) dilation. MA dysfunction may be a useful prognostic factor for operative timing and MR recurrence after successful mitral valve (MV) repair. The aim of this study was to evaluate additive prognostic factors of MA non-planarity using real-time 3D transesophageal echocardiography (RT3D-TEE) analysis in patients with chronic severe MR and preserved LV systolic function.
METHODS
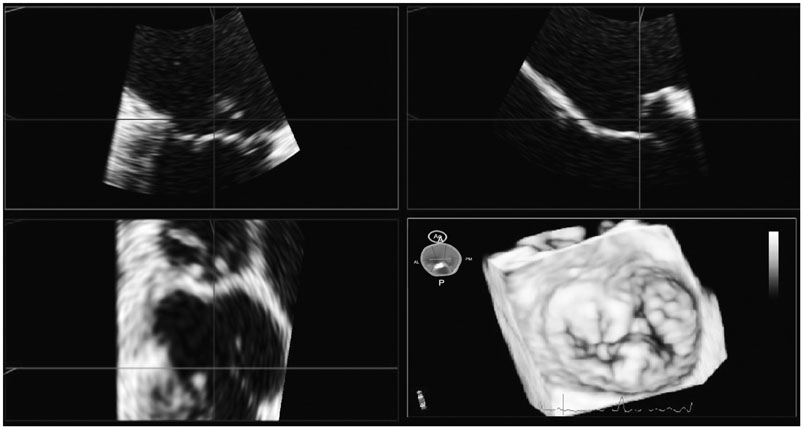
Forty-seven patients with chronic severe MR and preserved LV systolic function scheduled for MV repair were prospectively enrolled. Echocardiographic studies were performed before surgery and postoperatively within 2 weeks and at least 6 months after surgery. RT3D-TEE was performed before the operation and immediately post-operative.
RESULTS
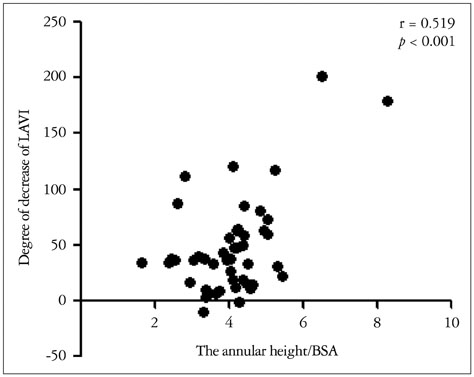
Mean age was 55.4 ± 15.1 years and 24 were male. Annulus height/body surface area (BSA) obtained via RT3D-TEE was correlated with the degree of postoperative LA remodeling. Patients were divided into two groups by average baseline annulus height/BSA. Patients with normal annular height had a smaller postoperative LV end-diastolic dimension, LV end-systolic dimension and LA volume index than patients with decreased annular height. Preoperative annulus height/BSA values strongly predicted postoperative LA remodeling.
CONCLUSION
MA height may be a useful prognostic factor for determining the timing of surgery in patients with chronic primary MR. Annulus height/BSA assessed via RT3D-TEE may provide additional information predictive of postoperative LA remodeling after successful MV repair.
Keyword
MeSH Terms
Figure
Reference
-
1. Freed LA, Levy D, Levine RA, Larson MG, Evans JC, Fuller DL, Lehman B, Benjamin EJ. Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med. 1999; 341:1–7.2. Enriquez-Sarano M, Sundt TM 3rd. Early surgery is recommended for mitral regurgitation. Circulation. 2010; 121:804–811. discussion 812.3. Flameng W, Herijgers P, Bogaerts K. Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation. 2003; 107:1609–1613.4. Flameng W, Meuris B, Herijgers P, Herregods MC. Durability of mitral valve repair in Barlow disease versus fibroelastic deficiency. J Thorac Cardiovasc Surg. 2008; 135:274–282.5. Le Tourneau T, Messika-Zeitoun D, Russo A, Detaint D, Topilsky Y, Mahoney DW, Suri R, Enriquez-Sarano M. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardiol. 2010; 56:570–578.6. Rusinaru D, Tribouilloy C, Grigioni F, Avierinos JF, Suri RM, Barbieri A, Szymanski C, Ferlito M, Michelena H, Tafanelli L, Bursi F, Mezghani S, Branzi A, Habib G, Modena MG, Enriquez-Sarano M. Mitral Regurgitation International DAtabase (MIDA) Investigators. Left atrial size is a potent predictor of mortality in mitral regurgitation due to flail leaflets: results from a large international multicenter study. Circ Cardiovasc Imaging. 2011; 4:473–481.7. Adams DH, Anyanwu AC, Rahmanian PB, Abascal V, Salzberg SP, Filsoufi F. Large annuloplasty rings facilitate mitral valve repair in Barlow's disease. Ann Thorac Surg. 2006; 82:2096–2100. discussion 2101.8. Jensen MØ, Jensen H, Nielsen SL, Smerup M, Johansen P, Yoganathan AP, Nygaard H, Hasenkam JM. What forces act on a flat rigid mitral annuloplasty ring? J Heart Valve Dis. 2008; 17:267–275. discussion 275.9. Jensen MO, Jensen H, Levine RA, Yoganathan AP, Andersen NT, Nygaard H, Hasenkam JM, Nielsen SL. Saddle-shaped mitral valve annuloplasty rings improve leaflet coaptation geometry. J Thorac Cardiovasc Surg. 2011; 142:697–703.10. Machado LR, Meneghelo ZM, Le Bihan DC, Barretto RB, Carvalho AC, Moises VA. Preoperative left ventricular ejection fraction and left atrium reverse remodeling after mitral regurgitation surgery. Cardiovasc Ultrasound. 2014; 12:45.11. Jassar AS, Vergnat M, Jackson BM, McGarvey JR, Cheung AT, Ferrari G, Woo YJ, Acker MA, Gorman RC, Gorman JH 3rd. Regional annular geometry in patients with mitral regurgitation: implications for annuloplasty ring selection. Ann Thorac Surg. 2014; 97:64–70.12. Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. American Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802.13. Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, Hagendorff A, Monin JL, Badano L, Zamorano JL. European Association of Echocardiography. European Association of Echocardiography recommendations for the assessment of valvular regurgitation. Part 2: mitral and tricuspid regurgitation (native valve disease). Eur J Echocardiogr. 2010; 11:307–332.14. Lee AP, Hsiung MC, Salgo IS, Fang F, Xie JM, Zhang YC, Lin QS, Looi JL, Wan S, Wong RH, Underwood MJ, Sun JP, Yin WH, Wei J, Tsai SK, Yu CM. Quantitative analysis of mitral valve morphology in mitral valve prolapse with real-time 3-dimensional echocardiography: importance of annular saddle shape in the pathogenesis of mitral regurgitation. Circulation. 2013; 127:832–841.15. Mahmood F, Subramaniam B, Gorman JH 3rd, Levine RM, Gorman RC, Maslow A, Panzica PJ, Hagberg RM, Karthik S, Khabbaz KR. Three-dimensional echocardiographic assessment of changes in mitral valve geometry after valve repair. Ann Thorac Surg. 2009; 88:1838–1844.16. Little SH, Ben Zekry S, Lawrie GM, Zoghbi WA. Dynamic annular geometry and function in patients with mitral regurgitation: insight from three-dimensional annular tracking. J Am Soc Echocardiogr. 2010; 23:872–879.17. Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC). European Association for Cardio-Thoracic Surgery (EACTS). Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, Baumgartner H, Borger MA, Carrel TP, De Bonis M, Evangelista A, Falk V, Iung B, Lancellotti P, Pierard L, Price S, Schäfers HJ, Schuler G, Stepinska J, Swedberg K, Takkenberg J, Von Oppell UO, Windecker S, Zamorano JL, Zembala M. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012; 33:2451–2496.18. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM 3rd, Thomas JD. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2438–2488.19. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14.20. Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, Lee MM, Park YB, Choi YS, Seo JD, Lee YW. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997; 30:474–480.21. Messika-Zeitoun D, Bellamy M, Avierinos JF, Breen J, Eusemann C, Rossi A, Behrenbeck T, Scott C, Tajik JA, Enriquez-Sarano M. Left atrial remodelling in mitral regurgitation--methodologic approach, physiological determinants, and outcome implications: a prospective quantitative Doppler-echocardiographic and electron beam-computed tomographic study. Eur Heart J. 2007; 28:1773–1781.22. Grewal J, Suri R, Mankad S, Tanaka A, Mahoney DW, Schaff HV, Miller FA, Enriquez-Sarano M. Mitral annular dynamics in myxomatous valve disease: new insights with real-time 3-dimensional echocardiography. Circulation. 2010; 121:1423–1431.23. Adams DH, Rosenhek R, Falk V. Degenerative mitral valve regurgitation: best practice revolution. Eur Heart J. 2010; 31:1958–1966.24. Salgo IS, Gorman JH 3rd, Gorman RC, Jackson BM, Bowen FW, Plappert T, St John Sutton MG, Edmunds LH Jr. Effect of annular shape on leaflet curvature in reducing mitral leaflet stress. Circulation. 2002; 106:711–717.25. Jensen MO, Hagège AA, Otsuji Y, Levine RA. Leducq Transatlantic MITRAL Network. The unsaddled annulus: biomechanical culprit in mitral valve prolapse? Circulation. 2013; 127:766–768.26. Warraich HJ, Chaudary B, Maslow A, Panzica PJ, Pugsley J, Mahmood F. Mitral annular nonplanarity: correlation between annular height/commissural width ratio and the nonplanarity angle. J Cardiothorac Vasc Anesth. 2012; 26:186–190.27. Machino-Ohtsuka T, Seo Y, Ishizu T, Sato K, Sugano A, Yamamoto M, Hamada-Harimura Y, Aonuma K. Novel Mechanistic Insights Into Atrial Functional Mitral Regurgitation-3-Dimensional Echocardiographic Study. Circ J. 2016; 80:2240–2248.28. La Canna G, Arendar I, Maisano F, Monaco F, Collu E, Benussi S, De Bonis M, Castiglioni A, Alfieri O. Real-time three-dimensional transesophageal echocardiography for assessment of mitral valve functional anatomy in patients with prolapse-related regurgitation. Am J Cardiol. 2011; 107:1365–1374.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does The Mitral Annulus Shrink or Enlarge During Systole? A Real-Time 3D Echocardiography Study
- Left ventricular function after mitral valve operation in congenital mitral regurgitation
- Evaluation of Left Ventricular Systolic Function by Tissue Doppler Imaging
- Clinical and Echocardiographic Findings in Patients who Underwent Mitral Valve repair Surgery
- Mitral Valve Replacement for Bulky, Calcified Mitral Annulus: A Case Report