Allergy Asthma Immunol Res.
2017 Sep;9(5):431-437. 10.4168/aair.2017.9.5.431.
Asthma-COPD Overlap Shows Favorable Clinical Outcomes Compared to Pure COPD in a Korean COPD Cohort
- Affiliations
-
- 1Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. littmann@yuhs.ac
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea.
- 3Regional Center for Respiratory Disease, Yeungnam University Medicial Center, Yeungnam University College of Medicine, Daegu, Korea.
- 4Division of Respiratory and Allergy Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 5Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 6Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 7Division of Pulmonary Medicine, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- KMID: 2383991
- DOI: http://doi.org/10.4168/aair.2017.9.5.431
Abstract
- PURPOSE
Comparisons of the characteristics of chronic obstructive pulmonary disease (COPD) and asthma-COPD overlap syndrome (ACOS) have been the focus of several studies since the diseases were defined by the Global Initiative for Asthma and Global Initiative for Chronic Obstructive Lung Disease guidelines. However, no consensus is available yet. In this study, we aimed to compare the characteristics of asthma-COPD overlap (ACO) and COPD.
METHODS
We retrospectively reviewed 1,504 patients with COPD in a Korean COPD Subtype Study cohort. The occurrence of ACO was defined as a positive response to a bronchodilator (an increase in forced expiratory volume in 1 second [FEV1] of 12% and 200 mL).
RESULTS
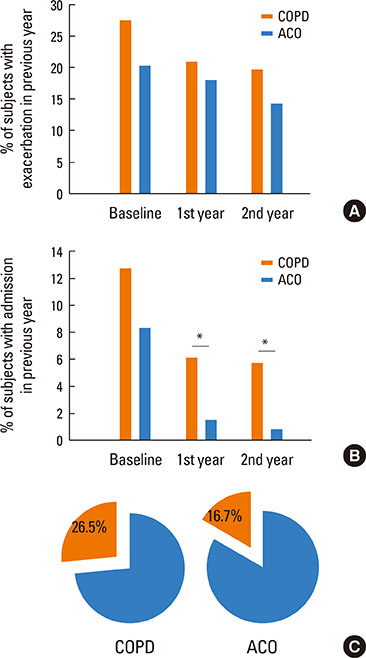
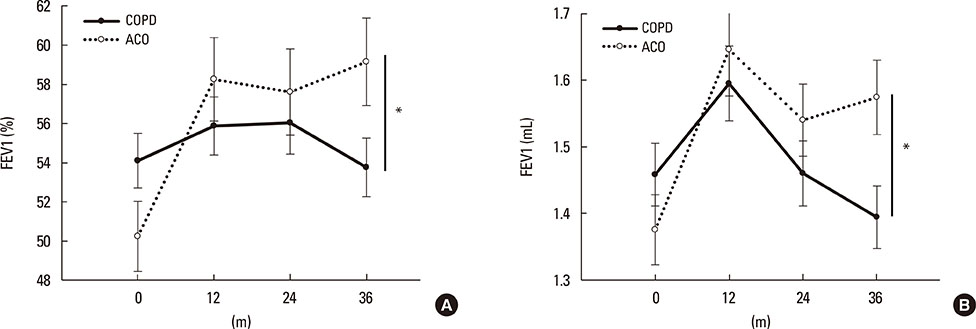
Among 1,504 patients with COPD, 223 (14.8%) were diagnosed with ACO. Men (95.5%) and current smokers (32.9%) were more prevalent in the ACO group compared with the pure COPD group (90.5% and 25.3%, respectively; P=0.015 and P=0.026, respectively). Patients with ACO had a better quality of life (St. George's Respiratory Questionnaire for COPD score=31.0±18.0 [mean±standard deviation]) than those with pure COPD (35.3±19.1) (P=0.002). Although the prevalence of acute exacerbation was not different between the 2 groups, patients with severe exacerbation required hospital admission significantly more frequently in the pure COPD group than in the ACO group. Patients with ACO showed a higher likelihood of FEV1 recovery than those with pure COPD (P<0.001).
CONCLUSIONS
We suggest that ACO is characterized by less severe symptoms, and therefore it might lead to rare severe exacerbation and the possibility of lung function recovery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Impact of the Endothelial Tight Junction Protein Claudin-5 on Clinical Profiles of Patients With COPD
Byeong-Gon Kim, Pureun-Haneul Lee, Sun-Hye Lee, Ae-Rin Baek, Jong-Sook Park, Junehyuk Lee, Sung-Woo Park, Do-Jin Kim, Choon-Sik Park, An-Soo Jang
Allergy Asthma Immunol Res. 2018;10(5):533-542. doi: 10.4168/aair.2018.10.5.533.
Reference
-
1. Yoon HI. Respiratory review of 2014: asthma. Tuberc Respir Dis. 2014; 77:237–242.2. Kim DK, Park YB, Oh YM, Jung KS, Yoo JH, Yoo KH, et al. Korean Asthma Guideline 2014: summary of major updates to the Korean Asthma Guideline 2014. Tuberc Respir Dis. 2016; 79:111–120.3. Seo JY, Hwang YI, Mun SY, Kim JH, Kim JH, Park SH, et al. Awareness of COPD in a high risk Korean population. Yonsei Med J. 2015; 56:362–367.4. Kim HY. Resveratrol in asthma: a French paradox? Allergy Asthma Immunol Res. 2017; 9:1–2.5. Caillaud D, Chanez P, Escamilla R, Burgel PR, Court-Fortune I, Nesme-Meyer P, et al. Asthma-COPD overlap syndrome (ACOS) vs ‘pure’ COPD: a distinct phenotype? Allergy. 2017; 72:137–145.6. Fu JJ, McDonald VM, Gibson PG, Simpson JL. Systemic inflammation in older adults with asthma-COPD overlap syndrome. Allergy Asthma Immunol Res. 2014; 6:316–324.7. Lee HY, Kang JY, Yoon HK, Lee SY, Kwon SS, Kim YK, et al. Clinical characteristics of asthma combined with COPD feature. Yonsei Med J. 2014; 55:980–986.8. Miravitlles M, Soriano JB, Ancochea J, Muñoz L, Duran-Tauleria E, Sánchez G, et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med. 2013; 107:1053–1060.9. Barnes PJ. Asthma-COPD overlap. Chest. 2016; 149:7–8.10. Chung WS, Lin CL, Kao CH. Comparison of acute respiratory events between asthma-COPD overlap syndrome and COPD patients: a population-based cohort study. Medicine (Baltimore). 2015; 94:e755.11. de Marco R, Marcon A, Rossi A, Antó JM, Cerveri I, Gislason T, et al. Asthma, COPD and overlap syndrome: a longitudinal study in young European adults. Eur Respir J. 2015; 46:671–679.12. Cosio BG, Soriano JB, López-Campos JL, Calle-Rubio M, Soler-Cataluna JJ, de-Torres JP, et al. Defining the asthma-COPD overlap syndrome in a COPD cohort. Chest. 2016; 149:45–52.13. Global Initiative for Asthma. 2017 GINA report, global strategy for asthma management and prevention [Internet]. place unknown: Global Initiative for Asthma;2017. cited 2017 Mar 21. Available from: http://ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention/.14. Lee JY, Chon GR, Rhee CK, Kim DK, Yoon HK, Lee JH, et al. Characteristics of patients with chronic obstructive pulmonary disease at the first visit to a pulmonary medical center in Korea: the Korea COPD subgroup study team cohort. J Korean Med Sci. 2016; 31:553–560.15. Tsiligianni IG, van der Molen T, Moraitaki D, Lopez I, Kocks JW, Karagiannis K, et al. Assessing health status in COPD. A head-to-head comparison between the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ). BMC Pulm Med. 2012; 12:20.16. Jones PW. St George's respiratory questionnaire for COPD patients (SGRQ-C): manual. London: St Geroge's University of London;2005.17. Menezes AM, Montes de Oca M, Pérez-Padilla R, Nadeau G, Wehrmeister FC, Lopez-Varela MV, et al. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest. 2014; 145:297–304.18. Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpeläinen M, Kinnula VL, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011; 48:279–285.19. Izquierdo-Alonso JL, Rodriguez-Gonzálezmoro JM, de Lucas-Ramos P, Unzueta I, Ribera X, Antón E, et al. Prevalence and characteristics of three clinical phenotypes of chronic obstructive pulmonary disease (COPD). Respir Med. 2013; 107:724–731.20. Chung JW, Kong KA, Lee JH, Lee SJ, Ryu YJ, Chang JH. Characteristics and self-rated health of overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2014; 9:795–804.21. Hardin M, Silverman EK, Barr RG, Hansel NN, Schroeder JD, Make BJ, et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011; 12:127.22. Kim SY, Jung JY, Park MS, Kang YA, Kim EY, Kim SK, et al. Increased prevalence of self-reported asthma among Korean adults: an analysis of KNHANES I and IV data. Lung. 2013; 191:281–288.23. Soler-Cataluña JJ, Cosío B, Izquierdo JL, López-Campos JL, Marín JM, Agüero R, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012; 48:331–337.24. Sin DD, Miravitlles M, Mannino DM, Soriano JB, Price D, Celli BR, et al. What is asthma-COPD overlap syndrome? Towards a consensus definition from a round table discussion. Eur Respir J. 2016; 48:664–673.25. Barrecheguren M, Román-Rodríguez M, Miravitlles M. Is a previous diagnosis of asthma a reliable criterion for asthma-COPD overlap syndrome in a patient with COPD? Int J Chron Obstruct Pulmon Dis. 2015; 10:1745–1752.26. Calverley PM, Albert P, Walker PP. Bronchodilator reversibility in chronic obstructive pulmonary disease: use and limitations. Lancet Respir Med. 2013; 1:564–573.27. Contoli M, Baraldo S, Marku B, Casolari P, Marwick JA, Turato G, et al. Fixed airflow obstruction due to asthma or chronic obstructive pulmonary disease: 5-year follow-up. J Allergy Clin Immunol. 2010; 125:830–837.28. Baarnes CB, Kjeldgaard P, Nielsen M, Miravitlles M, Ulrik CS. Identifying possible asthma-COPD overlap syndrome in patients with a new diagnosis of COPD in primary care. NPJ Prim Care Respir Med. 2017; 27:16084.29. de Marco R, Pesce G, Marcon A, Accordini S, Antonicelli L, Bugiani M, et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One. 2013; 8:e62985.30. Tamada T, Sugiura H, Takahashi T, Matsunaga K, Kimura K, Katsumata U, et al. Biomarker-based detection of asthma-COPD overlap syndrome in COPD populations. Int J Chron Obstruct Pulmon Dis. 2015; 10:2169–2176.31. Cosio BG, Soriano JB, López-Campos JL, Calle M, Soler JJ, De-Torres JP, et al. Distribution and outcomes of a phenotype-based approach to guide COPD management: results from the CHAIN cohort. PLoS One. 2016; 11:e0160770.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Status of Studies Investigating Asthma–Chronic Obstructive Pulmonary Disease Overlap in Korea: A Review
- The Relationship of Chronic Obstructive Pulmonary Disease (COPD) to Asthma
- Systemic Inflammation in Older Adults With Asthma-COPD Overlap Syndrome
- Overlap Between Asthma and COPD: Where the Two Diseases Converge
- Asthma-COPD Overlap Syndrome: What We Know and What We Don't