Ann Rehabil Med.
2017 Feb;41(1):66-71. 10.5535/arm.2017.41.1.66.
Ultrasonography Evaluation of Vulnerable Vessels Around Cervical Nerve Roots During Selective Cervical Nerve Root Block
- Affiliations
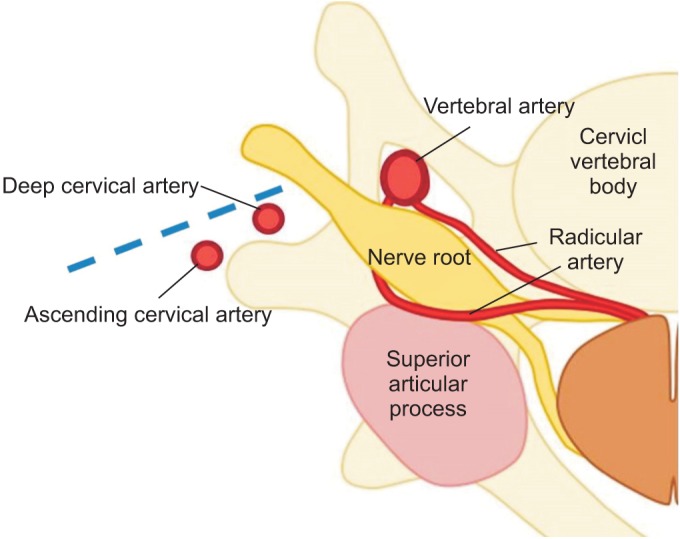
-
- 1Department of Rehabilitation Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. jseok337@snu.ac.kr
- 2Department of Rehabilitation Medicine, Daegu Fatima Hospital, Daegu, Korea.
- 3Department of Rehabilitation Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- KMID: 2383679
- DOI: http://doi.org/10.5535/arm.2017.41.1.66
Abstract
OBJECTIVE
To evaluate the prevalence of vulnerable blood vessels around cervical nerve roots before cervical nerve root block in the clinical setting.
METHODS
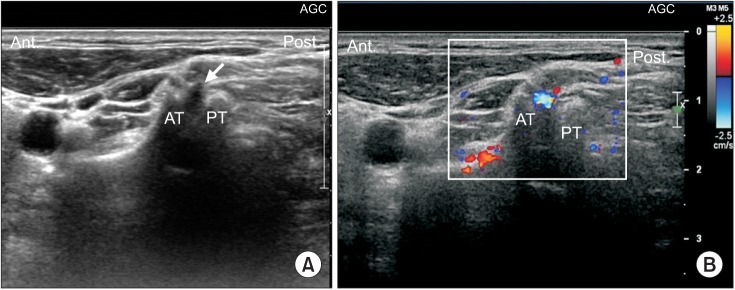
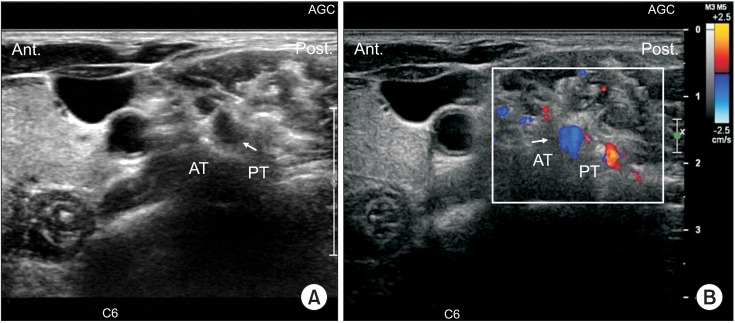
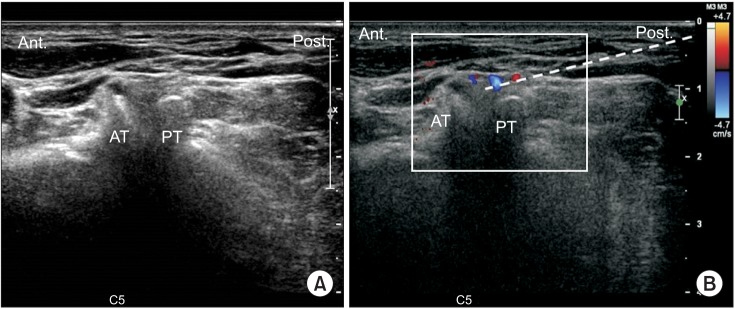
This retrospective study included 74 patients with cervical radiculopathy who received an ultrasonography-guided nerve block at an outpatient clinic from July 2012 to July 2014. Before actual injection of the steroid was performed, we evaluated the vulnerable blood vessels around each C5, C6, and C7 nerve root of each patient's painful side, with Doppler ultrasound.
RESULTS
Out of 74 cases, the C5 level had 2 blood vessels (2.7%), the C6 level had 4 blood vessels (5.45%), and the C7 level had 6 blood vessels (8.11%) close to each targeted nerve root. Moreover, the C5 level had 2 blood vessels (2.7%), the C6 level 5 blood vessels (6.75%), and the C7 level had 4 blood vessels (5.45%) at the site of an imaginary needle's projected pathway to the targeted nerve root, as revealed by axial transverse ultrasound imaging with color Doppler imaging. In total, the C5 level had 4 blood vessels (5.45%), the C6 level 9 blood vessels (12.16%), and the C7 level 10 had blood vessels (13.51%) either at the targeted nerve root or at the site of the imaginary needle's projected pathway to the targeted nerve root. There was an unneglectable prevalence of vulnerable blood vessels either at the targeted nerve root or at the site of the needle' projected pathway to the nerve root. Also, it shows a higher prevalence of vulnerable blood vessels either at the targeted nerve root or at the site of an imaginary needle's projected pathway to the nerve root as the spinal nerve root level gets lower.
CONCLUSION
To prevent unexpected critical complications involving vulnerable blood vessel injury during cervical nerve root block, it is recommended to routinely evaluate for the presence of vulnerable blood vessels around each cervical nerve root using Doppler ultrasound imaging before the cervical nerve root block, especially for the lower cervical nerve root level.
MeSH Terms
Figure
Reference
-
1. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004; 100:1595–1600. PMID: 15166582.
Article2. Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks: an analysis of 1036 injections. J Bone Joint Surg Am. 2005; 87:1025–1030. PMID: 15866965.3. Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine J. 2004; 4:468–474. PMID: 15246308.4. Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005; 117:104–111. PMID: 16055268.
Article5. Hoeft MA, Rathmell JP, Monsey RD, Fonda BJ. Cervical transforaminal injection and the radicular artery: variation in anatomical location within the cervical intervertebral foramina. Reg Anesth Pain Med. 2006; 31:270–274. PMID: 16701194.
Article6. Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009; 34:343–348. PMID: 19574867.7. Yamauchi M, Suzuki D, Niiya T, Honma H, Tachibana N, Watanabe A, et al. Ultrasound-guided cervical nerve root block: spread of solution and clinical effect. Pain Med. 2011; 12:1190–1195. PMID: 21692976.
Article8. Martinoli C, Bianchi S, Santacroce E, Pugliese F, Graif M, Derchi LE. Brachial plexus sonography: a technique for assessing the root level. AJR Am J Roentgenol. 2002; 179:699–702. PMID: 12185049.
Article9. Matula C, Trattnig S, Tschabitscher M, Day JD, Koos WT. The course of the prevertebral segment of the vertebral artery: anatomy and clinical significance. Surg Neurol. 1997; 48:125–131. PMID: 9242236.
Article10. Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injection of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215. PMID: 12749976.
Article11. Hopkins PM. Ultrasound guidance as a gold standard in regional anaesthesia. Br J Anaesth. 2007; 98:299–301. PMID: 17307777.
Article12. Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skeletal Radiol. 2013; 42:69–78. PMID: 22609989.
Article13. Kondo K, Molgaard CA, Kurland LT, Onofrio BM. Protruded intervertebral cervical disk: incidence and affected cervical level in Rochester, Minnesota, 1950 through 1974. Minn Med. 1981; 64:751–753. PMID: 7335047.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Spinal Cord Injury after Cervical Nerve Root Block
- The Ultrasound-guided Selective Nerve Root Injections in the Lower Cervical Spines
- An Anatomical Study on the Variations of the First Cervical Dorsal Root
- The Value of Selective Nerve Root Block to Predict Surgical Outcome for Spinal Surgery
- The Efficacy and Persistence of Selective Nerve Root Block under Fluoroscopic Guidance for Cervical Radiculopathy