Ann Rehabil Med.
2017 Feb;41(1):9-15. 10.5535/arm.2017.41.1.9.
Recommendation of Nasogastric Tube Removal in Acute Stroke Patients Based on Videofluoroscopic Swallow Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kyungpook National University College of Medicine, Daegu, Korea. teeed0522@hanmail.net
- 2Department of Rehabilitation Medicine, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 2383672
- DOI: http://doi.org/10.5535/arm.2017.41.1.9
Abstract
OBJECTIVE
To evaluate the safety of nasogastric tube (NGT) removal and change to oral feeding with a food thickener for acute stroke patients in whom a videofluoroscopic swallow study (VFSS) confirmed thin liquid aspiration.
METHODS
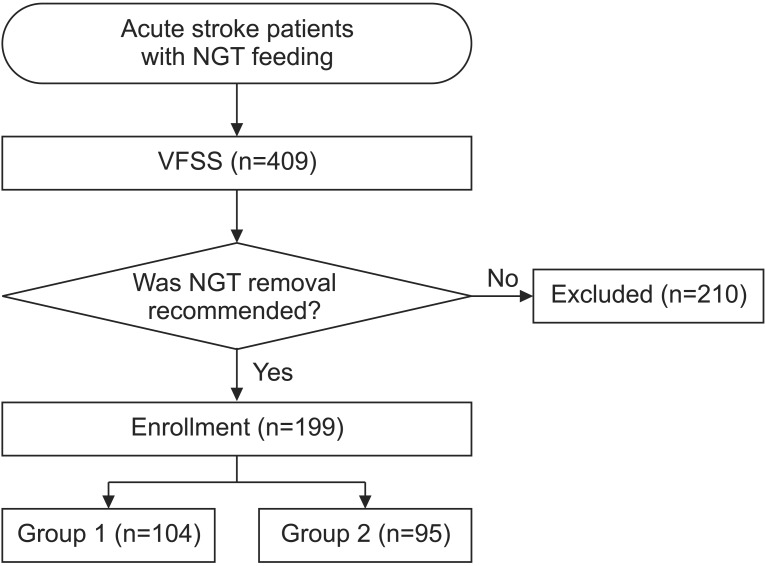
We retrospectively examined data of 199 patients with first stroke who were diagnosed with dysphagia from 2011 to 2015. Swallowing function was evaluated using VFSS. Patients included in this study were monitored for 4 weeks to identify the occurrence of aspiration pneumonia. The penetration-aspiration scale (PAS) was used to assess VFSS findings. The patients were divided into thin-liquid aspiration group (group 1, n=104) and no thin-liquid aspiration group (group 2, n=95).
RESULTS
The feeding method was changed from NGT feeding to oral feeding with food thickener (group 1) and without food thickener (group 2). The PAS scores of thin and thick liquids were 6.46±0.65 and 1.92±0.73, respectively, in group 1 and 2.65±0.74 and 1.53±0.58, respectively, in group 2. Aspiration pneumonia developed in 1.9% of group 1 and 3.2% of group 2 (p=0.578), with no significant difference between the groups.
CONCLUSION
We concluded that removing the NGT and changing to oral feeding with a food thickener is a safe food modification for acute stroke patients with thin liquid aspiration. Therefore, we recommend that VFSS should be conducted promptly in acute stroke patients to avoid unnecessary prolonged NGT feeding.
MeSH Terms
Figure
Cited by 2 articles
-
Epiglottic Retroflexion is a Key Indicator of Functional Recovery of Post-stroke Dysphagia
Ji Soo Choi, Hyun Bang, Goo Joo Lee, Han Gil Seo, Byung-Mo Oh, Tai Ryoon Han
Ann Rehabil Med. 2020;44(1):1-10. doi: 10.5535/arm.2020.44.1.1.Clinical Factors Associated With Successful Gastrostomy Tube Weaning in Patients With Prolonged Dysphagia After Stroke
Bo Seong Jang, Jun Young Park, Jae Hyun Lee, Young Joo Sim, Ho Joong Jeong, Ghi Chan Kim
Ann Rehabil Med. 2021;45(1):33-41. doi: 10.5535/arm.20149.
Reference
-
1. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204. PMID: 8685928.2. Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis. 2000; 10:380–386. PMID: 10971024.
Article3. Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil. 1995; 76:310–316. PMID: 7717830.
Article4. Holas MA, DePippo KL, Reding MJ. Aspiration and relative risk of medical complications following stroke. Arch Neurol. 1994; 51:1051–1053. PMID: 7945003.
Article5. Aslanyan S, Weir CJ, Diener HC, Kaste M, Lees KR. GAIN International Steering Committee and Investigators. Pneumonia and urinary tract infection after acute ischaemic stroke: a tertiary analysis of the GAIN International trial. Eur J Neurol. 2004; 11:49–53. PMID: 14692888.
Article6. Palmer JB, Pelletier CA, Matsuo K. Physical medicine and rehabilitation. In : Braddom RL, editor. Rehabilitation of patients with swallowing disorders. 4th ed. Philadelphia: Saunders;2011. p. 581–597.7. Jung SH, Lee KJ, Hong JB, Han TR. Validation of clinical dysphagia scale: based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:343–350.8. Eyal H. Evaluation and treatment of swallowing disorders (dysphagia): the American model as an opportunity for improving patient care and cost containment in Israel's healthcare system. Harefuah. 1997; 132:775–778. PMID: 9223821.9. Dennis MS, Lewis SC, Warlow C. FOOD Trial Collaboration. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Lancet. 2005; 365:764–772. PMID: 15733717.10. Gomes CA Jr, Lustosa SA, Matos D, Andriolo RB, Waisberg DR, Waisberg J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst Rev. 2012; (3):CD008096. PMID: 22419328.
Article11. Kuhlemeier KV, Palmer JB, Rosenberg D. Effect of liquid bolus consistency and delivery method on aspiration and pharyngeal retention in dysphagia patients. Dysphagia. 2001; 16:119–122. PMID: 11305221.
Article12. Horner J, Massey EW. Managing dysphagia. Special problems in patients with neurologic disease. Postgrad Med. 1991; 89:203–206. 211–213. PMID: 2008399.13. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-Ed;1998.14. Lim SH, Lieu PK, Phua SY, Seshadri R, Venketasubramanian N, Lee SH, et al. Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia. 2001; 16:1–6. PMID: 11213241.
Article15. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article16. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001; 344:665–671. PMID: 11228282.
Article17. Altman DG. Practical statistics for medical research. London: Chapman & Hall;1991.18. Katzan IL, Dawson NV, Thomas CL, Votruba ME, Cebul RD. The cost of pneumonia after acute stroke. Neurology. 2007; 68:1938–1943. PMID: 17536051.
Article19. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335. PMID: 19717014.
Article20. Langmore SE, Miller RM. Behavioral treatment for adults with oropharyngeal dysphagia. Arch Phys Med Rehabil. 1994; 75:1154–1160. PMID: 7944924.
Article21. Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999; 116:455–478. PMID: 9922328.
Article22. Logemann JA. Management of the patient with oropharyngeal swallowing disorders. In : Logemann JA, editor. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-Ed;1998. p. 307–326.23. Hilker R, Poetter C, Findeisen N, Sobesky J, Jacobs A, Neveling M, et al. Nosocomial pneumonia after acute stroke: implications for neurological intensive care medicine. Stroke. 2003; 34:975–981. PMID: 12637700.24. Lakshminarayan K, Tsai AW, Tong X, Vazquez G, Peacock JM, George MG, et al. Utility of dysphagia screening results in predicting poststroke pneumonia. Stroke. 2010; 41:2849–2854. PMID: 20947835.
Article25. Silveira MH, Dedivitis RA, Queija DS, Nascimento PC. Quality of life in swallowing disorders after nonsurgical treatment for head and neck cancer. Int Arch Otorhinolaryngol. 2015; 19:46–54. PMID: 25992151.
Article26. Launois R. Integration of patients' preferences in individual and collective health choices. Rev Epidemiol Sante Publique. 1994; 42:246–262. PMID: 8209082.27. Grindel CG, Whitmer K, Barsevick A. Quality of life and nutritional support in patients with cancer. Cancer Pract. 1996; 4:81–87. PMID: 8715445.28. Lazarus CL, Logemann JA, Rademaker AW, Kahrilas PJ, Pajak T, Lazar R, et al. Effects of bolus volume, viscosity, and repeated swallows in nonstroke subjects and stroke patients. Arch Phys Med Rehabil. 1993; 74:1066–1070. PMID: 8215858.
Article29. Ku DN, Ma PP, McConnel FM, Cerenko D. A kinematic study of the oropharyngeal swallowing of a liquid. Ann Biomed Eng. 1990; 18:655–669. PMID: 2281886.
Article30. Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia. 1994; 9:7–11. PMID: 8131429.
Article31. Terpenning M, Bretz W, Lopatin D, Langmore S, Dominguez B, Loesche W. Bacterial colonization of saliva and plaque in the elderly. Clin Infect Dis. 1993; 16(Suppl 4):S314–S316. PMID: 8324138.
Article32. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Nasogastric Tube on Swallowing Function in Stroke Patients with Dysphagia
- Prognostic Indicators in Dysphagia Recovery
- Self-Knotting of Nasogastric Tube in a Stroke Patient with Dysphagia: A Case Report
- A case of Nasogastric Tube Syndrome in Acute Ischemic Stroke Patient
- Gastroesophageal Reflux during Nasogastric Tube Feeding versus Oroesophageal Tube Feeding in Stroke Patients: A 24 Hour Esophageal pH-monitoring