Korean J Gastroenterol.
2016 Nov;68(5):270-273. 10.4166/kjg.2016.68.5.270.
A Case of Biliary Obstruction Caused by Liver Cyst
- Affiliations
-
- 1Department of Internal Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. cwj1225@naver.com
- 2Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2383505
- DOI: http://doi.org/10.4166/kjg.2016.68.5.270
Abstract
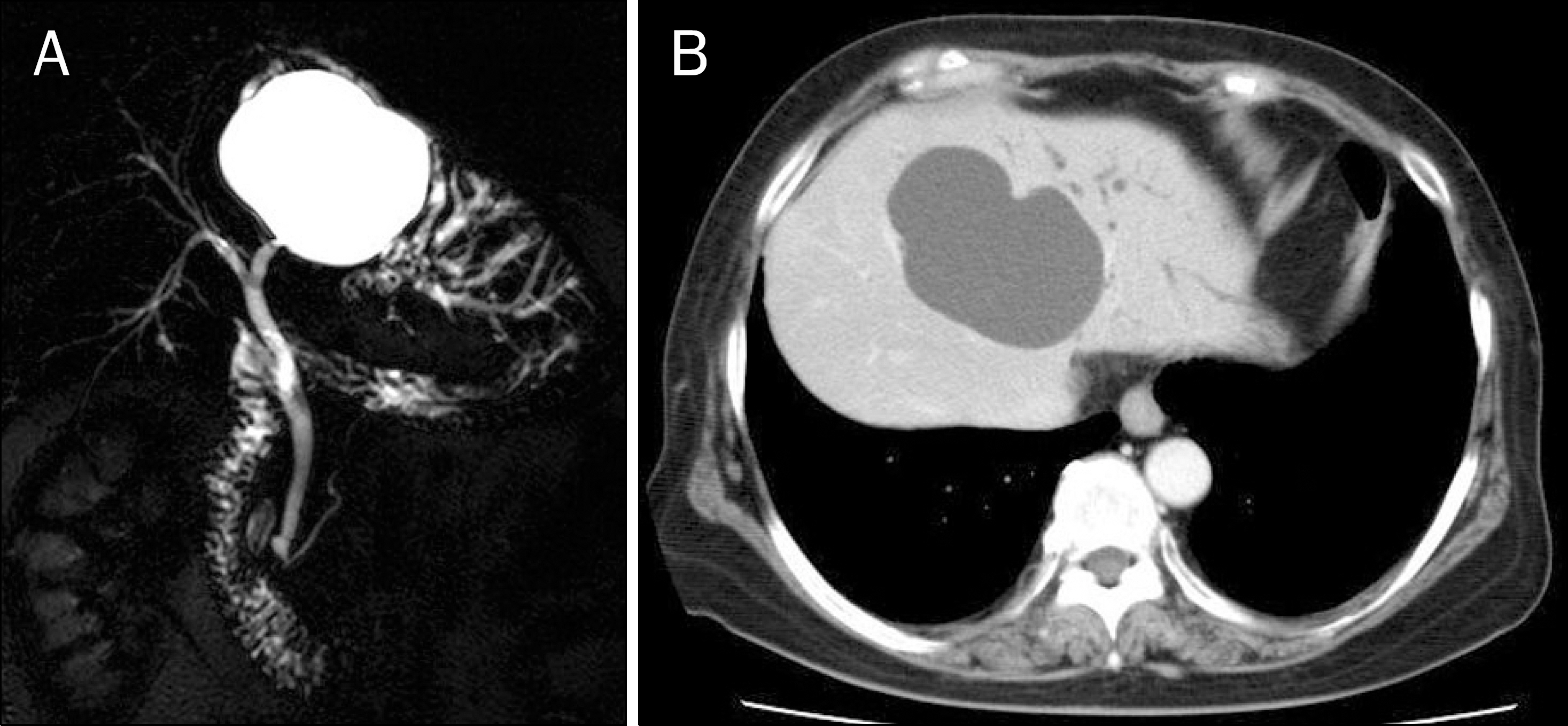
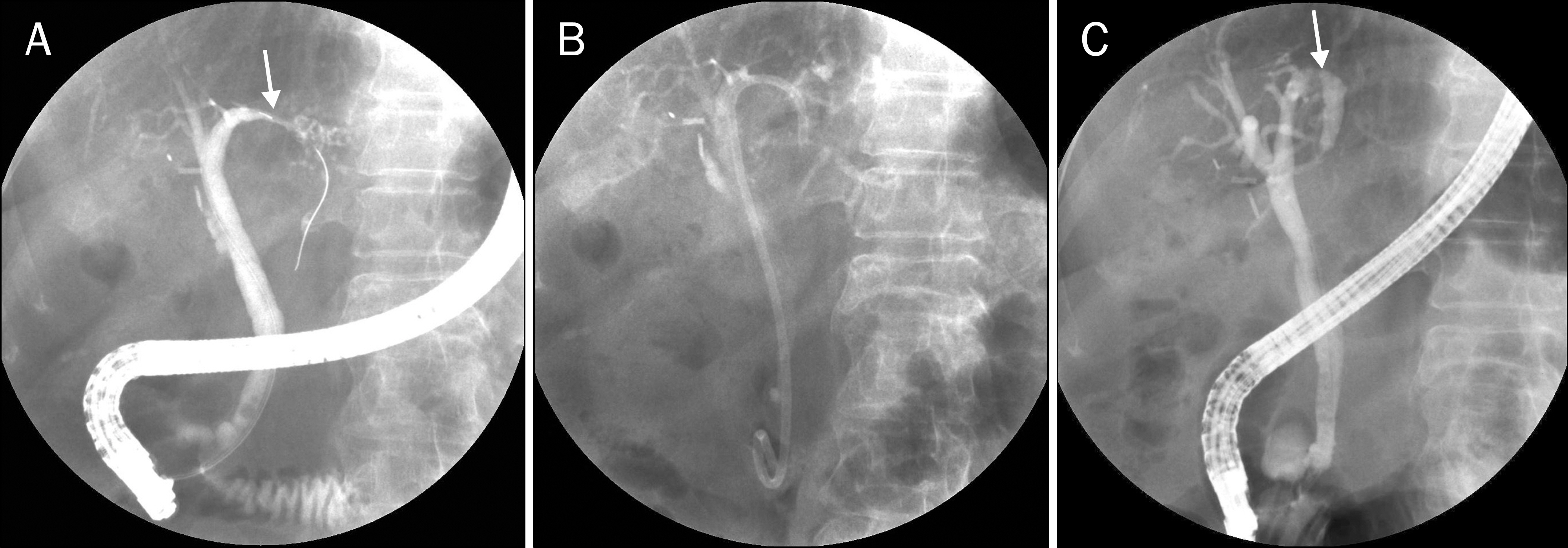
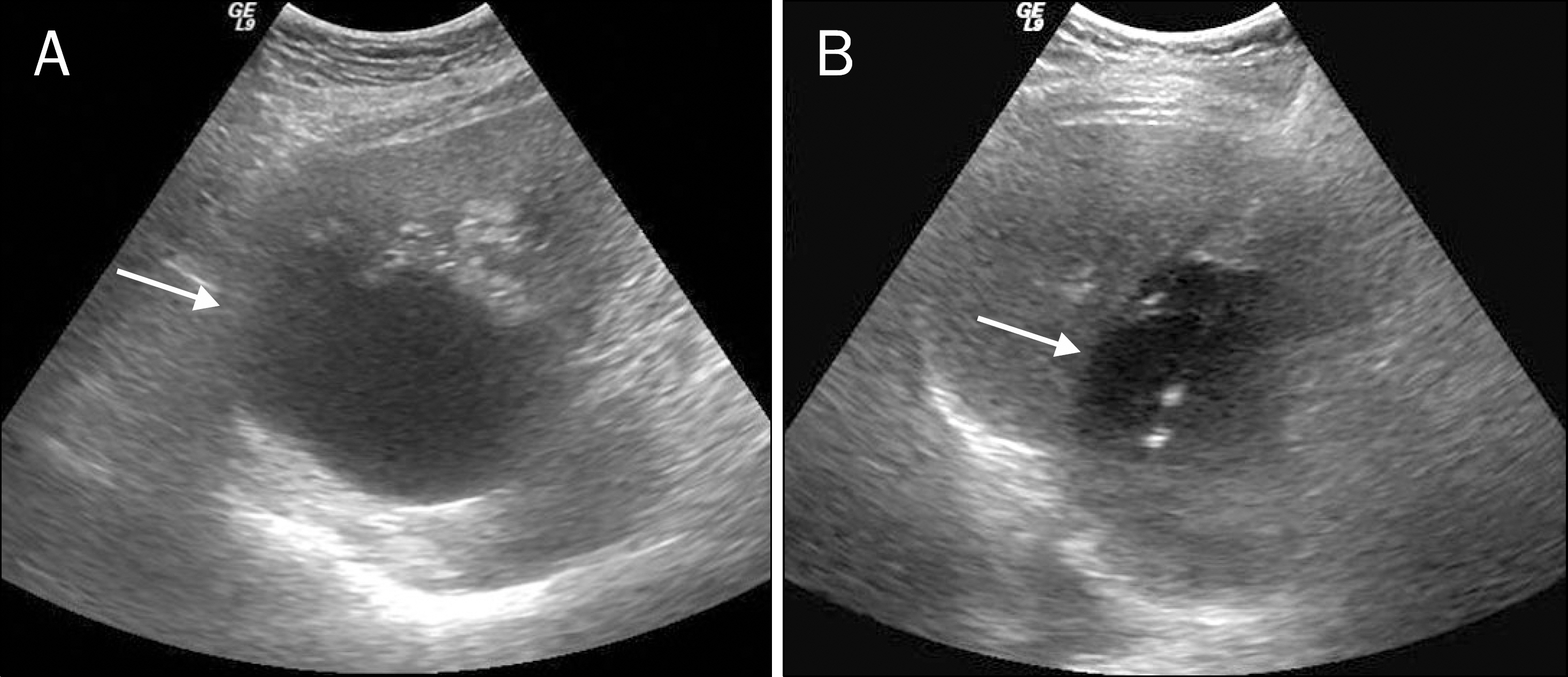
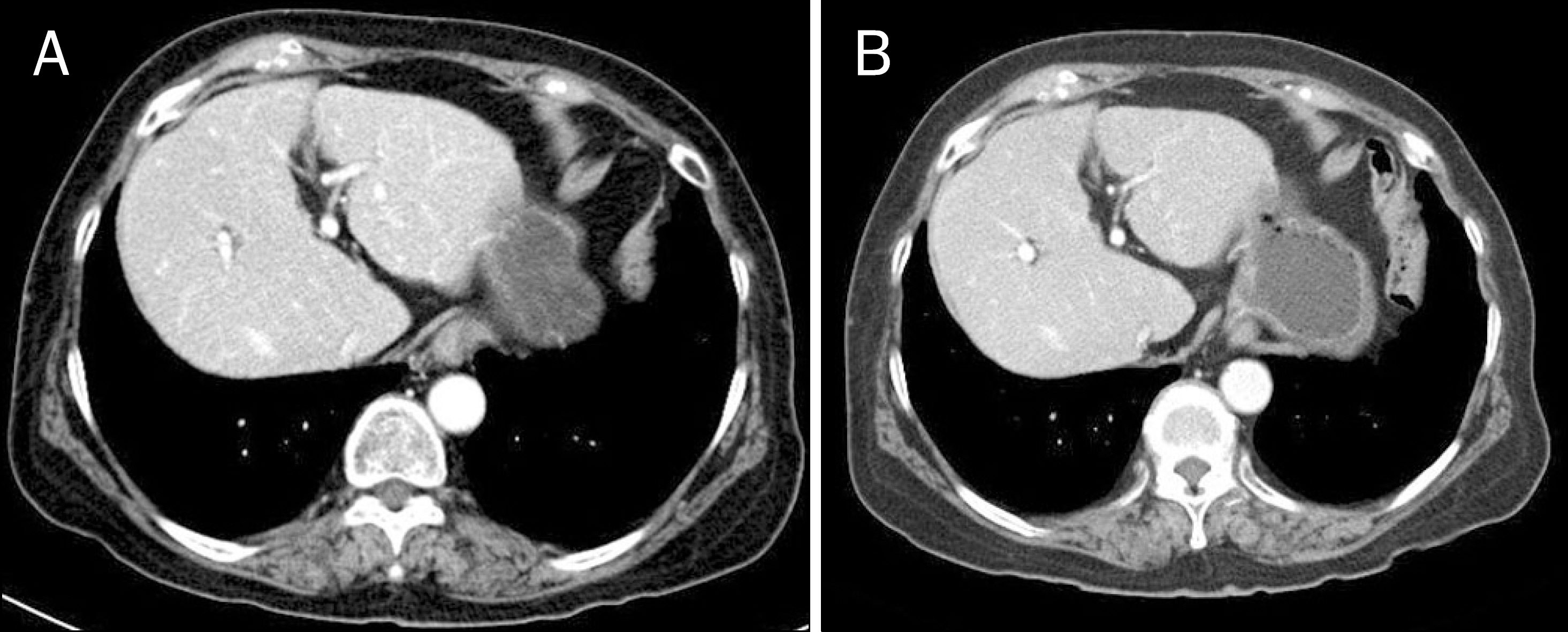
- Most cystic lesions of the liver are found incidentally in imaging studies because they are not symptomatic, and generally do not require treatment. Rarely, however, symptomatic hepatic cysts may develop complications and require treatment. Here, we describe a case of a 77-year-old woman who developed biliary obstruction with abdominal pain due to compression of the bile duct by a simple hepatic cyst. We confirmed the diagnosis based on symptoms and imaging studies. The patient's symptoms improved after simple cyst ablation by sclerotherapy.
Keyword
Figure
Reference
-
References
1. Salemis NS, Georgoulis E, Gourgiotis S, Tsohataridis E. Spontaneous rupture of a giant non parasitic hepatic cyst presenting as an acute surgical abdomen. Ann Hepatol. 2007; 6:190–193.2. Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010; 114:1–16.
Article3. Sanchez H, Gagner M, Rossi RL, et al. Surgical management of nonparasitic cystic liver disease. Am J Surg. 1991; 161:113–118.
Article4. Hai S, Hirohashi K, Uenishi T, et al. Surgical management of cystic hepatic neoplasms. J Gastroenterol. 2003; 38:759–764.
Article5. Benhamou JP, Menu Y. Nonparasitic cystic diseases of the liver and intrahepatic biliary tree. Blumgart LH, editor. Surgery of the liver and biliary tract. 2nd ed.New York: Churchill Livingstone Inc.;1994. p. 1197.6. Nisenbaum HL, Rowling SE. Ultrasound of focal hepatic lesions. Semin Roentgenol. 1995; 30:324–346.
Article7. Wijnands TF, Gevers TJ, Kool LJ, Drenth JP. Aspiration sclerotherapy combined with pasireotide to improve reduction of large symptomatic hepatic cysts (SCLEROCYST): study protocol for a randomized controlled trial. Trials. 2015; 16:82.
Article8. Wijnands TF, Lantinga MA, Drenth JP. Hepatic cyst infection following aspiration sclerotherapy: a case series. J Gastrointestin Liver Dis. 2014; 23:441–444.
Article9. Blonski WC, Campbell MS, Faust T, Metz DC. Successful aspiration and ethanol sclerosis of a large, symptomatic, simple liver cyst: case presentation and review of the literature. World J Gastroenterol. 2006; 12:2949–2954.
Article10. Masjedizadeh AR, Alavinejad P, Hormati A. A senile man with cystic lesion of liver and biliary obstruction. Gastroenterology. 2015; 148:e3–e4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Treatment of a Bronchobiliary Fistula Caused by Cholelithiasis: Case Report
- I131 Rose Bengal Liver Scanning
- Rare variant of type V choledochal cyst masquerading as a biliary cystadenoma
- Management of Obstructive Jaundice Caused by Hepatocellular Carcinoma
- A case of type IVa choledochal cyst